Académique Documents
Professionnel Documents
Culture Documents
Morning Report: Supervisor Dr. Sabar P. Siregar, SP - KJ
Transféré par
Hendra SetyawanDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Morning Report: Supervisor Dr. Sabar P. Siregar, SP - KJ
Transféré par
Hendra SetyawanDroits d'auteur :
Formats disponibles
MORNING REPORT
SUPERVISOR
dr. Sabar P. Siregar, Sp.KJ
Saturday
29
th
March
2014
IDENTITY
Name : Mrs. R
Age : 27 years old
Gender : Female
Address : Kebumen
Occupation : Unemployed
Marriage status : Married
Last education : Junior High School
Name : Mr. S
Age : 31 years old
Relation : Husband
GUARDIAN PATIENT
The reason patient was brought to
the hospital :
Restless
STRESSOR
conflict with
mother in
law
PRESENT HISTORY
Patient was brought by her
family because she was
restless without any reason.
She also did not want to talk
to the other.
2013
(August)
Since then
she
admitted to
the RSJS
Magelang.
- She did not want to work
- She did not socialize with neighbours
- She did not took goodcare of herself
- She did not take care her child
She readmitted to hospital because:
Restless
Did not want to eat
Did not want to speak
Sometimes laughing and talking to
herself
Prefer to be alone
March 2014
Since then
she
admitted to
the RSJS
Magelang.
- She did not want to work
- She did not socialize with neighbours
- She did not took goodcare of herself
- She did not take care her child
Restless
Didnt want to speak
Didnt want to eat
Prefer to be alone
Day of admission
Brought to
RSJS ER
by her
husband.
- She did not want to eat, sleep and
work
- She did not socialize with neighbours
- She did not took goodcare of herself
- She did not take care her child
Since 2009, patient was admitted
to the RSJS Magelang for five
times because of paranoid
schizophrenia and
undifferentiated schizophrenia
Psychiatric
history
Head injury (-)
Hypertension (-)
Convulsion (-)
Asthma (-)
Allergy (-)
History of admission (-)
General
medical
history
Drugs consumption (-)
Alcohol consumption (-)
Cigarette Smoking (-)
Drugs, alcohol
abuse, and
smoking history
EARLY CHILDHOOD PHASE (0-3 YEARS OLD)
Patients family can not recall any impairment on growth and development.
Other milestone can not be assessed properly.
Psychomotoric (no valid data)
There is no valid data when patient:
First time lifting the head (3-6 months), rolling over (3-6 months)
Sitting (7-8 months)
Crawling (6-9 months)
Standing (6-9 months)
Walking-running (16 months)
Holding objects in her hand (3-6 months)
Putting everything in her mouth (3-6 months)
Psychosocial (no valid data)
Parents can not recall the times when patient :
started smiling when seeing another face (3-6 months)
startled by noises (3-6 months)
when the patient first laugh or squirm when asked to play, nor playing claps with
others (6-9 months)
Communication (no valid data)
They were forgot on when patient started saying words 1 year like
mom or dad. (1 year old)
Emotion (no valid data)
They were forgot of patients reaction when playing, frightened by
strangers, when starting to show jealousy or competitiveness
towards other and toilet training.
Cognitive (no valid data)
They were forgot on which age the patient can follow objects,
recognizing her mother, recognize her family members.
They were forgot on when the patient first copied sounds that were
heard, or understanding simple orders.
INTERMEDIATE CHILDHOOD (3-11 YEARS OLD)
Psychomotor (no valid data)
forgot on when patients first time playing hide and seek or if patient ever
involved in any kind of sports.
Psychosocial (no valid data)
forgot about patients social relation.
Communication (no valid data)
forgot regarding patient ability to make friends at school and how many
friends patient have during his school period
Emotional (no valid data)
forgot on patients adaptation under stress, any incidents of bedwetting were
not known.
Cognitive (no valid data)
forgot on patients cognitive.
LATE CHILDHOOD & TEENAGE PHASE
Sexual development signs & activity (no valid data)
Patient first experience of menarche, etc.
Psychomotor (no valid data)
Patient had hobby
Psychosocial(no valid data)
Parents claimed that she had some friends.
Emotional (no valid data)
There is no valid data on patients reaction on playing, scared,
showed jealously or competitiveness
Communication (no valid data)
Patient can communicate well.
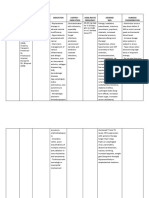
Eriksons stages of psychosocial
development
Stage Basic Conflict Important Events
Infancy
(birth to 18 months)
Trust vs mistrust Feeding
Early childhood
(2-3 years)
Autonomy vs shame and doubt Toilet training
Preschool
(3-5 years)
Initiative vs guilt Exploration
School age
(6-11 years)
Industry vs inferiority School
Adolescence
(12-18 years)
Identity vs role confusion Social relationships
Young Adulthood
(19-40 years)
Intimacy vs isolation Relationship
Middle adulthood
(40-65 years)
Generativity vs stagnation Work and parenthood
Maturity
(65- death)
Ego integrity vs despair Reflection on life
Family history
Patient is the 3rd child with six siblings
Psychiatry history in the family (+)
Genogram
Mental disorder Patient
Patient knows that she is female, her behavior is
appropriate for female, shes attracted to man.
Psychosexual history
Socio-economic history
Economic scale : low
Validity
Alloanamnesis : valid
Autoanamnesis : not valid
Progression of disorder
Symptom
Role function
2009 2014 2010
2011
2012
2013
Mental State
(Saturday, 29 March 2014)
Appearance
A female, appropriate to her age, completely
clothed.
State of Consciousness
Cloudy
Speech
Quantity : decreased
Quality : decreased
Behaviour
Hypoactive
Hyperactive
Echopraxia
Catatonia
Active negativism
Cataplexy
Streotypy
Mannerism
Automatism
Bizzare
Command automatism
Mutism
Acathysia
Tic
Somnabulism
Psychomotor agitation
Compulsive
Ataxia
Mimicry
Aggresive
Impulsive
Abulia
Non-
cooperative
Indiferrent
Apathy
Tension
Dependent
Passive
Infantile
Distrust
Labile
Rigid
Passive negativism
Stereotypy
Catalepsy
Cerea flexibility
Excitement
Emotion
Mood
Dysphoric
Euthymic
Elevated
Euphoria
Expansive
Irritable
Agitation
Cant be assesed
Affect
Appropriate
Inappropriate
Restrictive
Blunted
Flat
Labile
Disturbance of perception
Hallucination
Auditory (-)
Visual (-)
Olfactory (-)
Gustatory (-)
Tactile (-)
Somatic (-)
Illusion
Auditory (-)
Visual (-)
Olfactory (-)
Gustatory (-)
Tactile (-)
Somatic (-)
Depersonalization (-) Derealization (-)
CAN NOT BE ASSESSED
Thought progression
Neologisme
Circumtansiality
Tangential
Verbigrasi
Perseverasi
Sound association
Word salad
Echolalia
Incoherence
Irrelevant answer
Incoherence
Flight of idea
Poverty of speech
Confabulation
Loosening of
association
Quality Quantity
Logorrhea
Blocking
Remming
Mutism
Talkative
Content of thought
Idea of Reference
Idea of Guilt
Preoccupation
Obsession
Phobia
Delusion of Persecution
Delusion of Reference
Delusion of Envious
Delusion of Hipochondry
Delusion of magic-mystic
Delusion of grandiose
Delusion of Control
Delusion of Influence
Delusion of Passivity
Delusion of Perception
Delusion of Suspicious
Thought of Echo
Thought of Insertion /
withdrawal
Thought of Broadcasting
Idea of suicide
CAN NOT BE ASSESSED
Form of thought
Realistic
Non Realistic
Dereistic
Autistic
Sensorium and Cognition
Level of education : can not be assessed
General knowledge : can not be assessed
Orientation of time : can not be assessed
Orientations of place : can not be assessed
Orientations of peoples : can not be assessed
Orientations of situation : can not be assessed
Working/short/long memory: can not be assessed
Writing and reading skills : can not be assessed
Visuospatial : can not be assessed
Abstract thinking : can not be assessed
Ability to self care : bad
Impulse control when
examined
Self control: Enough
Patient response to
examiners question:
Bad
Insight
Impaired insight
Intellectual Insight
True Insight
Internal Status
Consciousnes : compos mentis
Vital sign :
Blood pressure : 130/90 mmHg
Pulse rate : 98 x/mnt
Temperature : Afebris
RR : 20 x/mnt, regular
Head : normocephali
Eyes : anemic conjungtiva -/-, icteric sclera -/-, pupil isocore
Neck : normal, no rigidity, no palpable lymph nodes
Thorax:
Cor : S 1,2 Sound and normal
Lung : vesicular sound, wheezing -/-, ronchi-/-
Abdomen : Pain (-) , normal peristaltic, tympany sound
Extremity : Warm acral, capp refill <2, tremor (-)
Neurological exam : not examined
Symptoms
-Restless
-Did not want to
speak
-Did not want to
eat
-Prefer to be
alone
Mental Status
Behavior: TIC,
psychomotor
agitation.
Mutism
Poverty of
speech
Impaired insight
Impairment
- She did not want
to eat, sleep and
work
- She did not
socialize with
neighbours
- She did not took
goodcare of
herself
- She did not take
care her child
Differential Diagnosis
F20.5 Residual Schizophrenia
F25.1 Schizoaffective Depressive Type
F32.3 Severe Depression with Psychotic
Sign
Multiaxial Diagnosis
Axis I : F32.3 Severe Depression with Psychotic Sign
Axis II : R 46.8 Delayed of Axis II diagnosis
Axis III : There is no diagnosis
Axis IV : Stressor was conflict with mother in law
Axis V : GAF on admission 30-21
Problem related to the patient
1. Problem about patients family
She had conflict with her mother in law
2. Problem abour social economy
Her economic condition was low
3. Problem about patients biological state
In Schizophrenia there is abnormal balancing of the neurotransmitter
(decreased of serotonin) limbic system which has the contribution for
the negative symptoms : Restless, did not want to speak, did not want
to eat, prefer to be alone. We need pharmacotherapy for re-balancing
the neurotransmitter
PLANNING MANAGEMENT
Inpatient (hospitalization)
Purpose of hospitalization is to decrease the
symptoms :
Restless
Did not want to speak
Did not want to eat
Prefer to be alone
Response Remission Recovery
RESPONSE PHASE
Target therapy : 50% decrease of symptom
Restless
Did not want to speak
Did not want to eat
Prefer to be alone
Emergency department
Antipsychotic: Typical (Haloperidol inj 5mg im)
Maintenance
Antidepressant: SSRI (Fluoxetine 2 x 20 mg po)
Antipsychotic: Atypical (Risperidone 2 x 2 mg po)
Re-assess patient
REMISSION PHASE
Target therapy :
100% remission of symptom within 4-9 months
Restless
Did not want to speak
Did not want to eat
Prefer to be alone
Inpatient management
1. 1. Continue the pharmacotherapy:
Antidepressant: SSRI (Fluoxetine 2 x 20 mg po)
Antipsychotic: Atypical (Risperidone 2 x 2 mg po)
1. 2. Improving the patient quality of life :
teach patient to care about herself (took a bath, toothbrushing)
Teach patient about her social & environment
( moping, clean the floor, washing the dishes)
Outpatient management
1. Pharmacotherapy
2. Psychosocial therapy
RECOVERY PHASE
Target therapy :
100% remission of symptom within 1 year.
Continue the medication,
control to psychiatric
Rehabilitation : help patient to
got & apply her skill
Family education
Thank you
Vous aimerez peut-être aussi
- Case Study Paranoid SchizoDocument46 pagesCase Study Paranoid SchizoDiksha Sharma100% (1)
- Case Presentation of DepressionDocument39 pagesCase Presentation of DepressionMithun Dey71% (28)
- Theory and Practice of CounsellingDocument12 pagesTheory and Practice of Counsellingeldho100% (1)
- Cannabinoid Es PDFDocument381 pagesCannabinoid Es PDFEduard RudenkoPas encore d'évaluation
- Gender Affirmation Surgery For The Treatment of Gender DysphoriaDocument4 pagesGender Affirmation Surgery For The Treatment of Gender DysphoriaJess Aloe100% (1)
- Gangguan Katatonik OrganikDocument41 pagesGangguan Katatonik OrganikFerji Rhenald ArdityaPas encore d'évaluation
- Morning Report: Saturday, 22 March 2014 Supervisor Dr. Sabar P. Siregar, SP - KJDocument40 pagesMorning Report: Saturday, 22 March 2014 Supervisor Dr. Sabar P. Siregar, SP - KJHendra SetyawanPas encore d'évaluation
- Supervisor Dr. Sabar P. Siregar, SP - KJ: Friday, 14 March 2014Document41 pagesSupervisor Dr. Sabar P. Siregar, SP - KJ: Friday, 14 March 2014Hendra SetyawanPas encore d'évaluation
- Morning Report: Supervisor Dr. Sabar P. Siregar, SP - KJDocument41 pagesMorning Report: Supervisor Dr. Sabar P. Siregar, SP - KJAyunita PermataPas encore d'évaluation
- Morning Report: TuesdayDocument40 pagesMorning Report: TuesdaybayuaulPas encore d'évaluation
- Morning Report: Supervisor Dr. Sabar P. Siregar, SP - KJDocument43 pagesMorning Report: Supervisor Dr. Sabar P. Siregar, SP - KJHendra SetyawanPas encore d'évaluation
- Morning Report: Supervisor Dr. Sabar P. Siregar, SP - KJDocument41 pagesMorning Report: Supervisor Dr. Sabar P. Siregar, SP - KJFerji Rhenald ArdityaPas encore d'évaluation
- Morning Report 17 SeptemberDocument42 pagesMorning Report 17 SeptemberkadibhaPas encore d'évaluation
- Morning Report: Supervisor Dr. Sabar P. Siregar, SP - KJDocument40 pagesMorning Report: Supervisor Dr. Sabar P. Siregar, SP - KJDani Fahma Qur'aniPas encore d'évaluation
- Morning Report: Supervisor Dr. Sabar P. Siregar, SP - KJDocument47 pagesMorning Report: Supervisor Dr. Sabar P. Siregar, SP - KJVike Poraddwita YuliantiPas encore d'évaluation
- Morning Report: Supervisor Dr. Sabar P. Siregar, SP - KJDocument40 pagesMorning Report: Supervisor Dr. Sabar P. Siregar, SP - KJAnastasia FebriantiPas encore d'évaluation
- Morpot 9 April 2015Document42 pagesMorpot 9 April 2015udjkwPas encore d'évaluation
- Sunday, 24 November 2013 Supervisor: DR Sabar P Siregar SP - KJDocument37 pagesSunday, 24 November 2013 Supervisor: DR Sabar P Siregar SP - KJMutiara SazkiaPas encore d'évaluation
- Case of Morning Report Sunday, 23 February 2014: Arranged byDocument19 pagesCase of Morning Report Sunday, 23 February 2014: Arranged byVike Poraddwita YuliantiPas encore d'évaluation
- Morpot Skizoafektif Tipe DepresiDocument37 pagesMorpot Skizoafektif Tipe DepresiNovina FirliaPas encore d'évaluation
- 9morning Report Dakshnamoorthy Vythinathan 300914Document43 pages9morning Report Dakshnamoorthy Vythinathan 300914AnonymousssPas encore d'évaluation
- Morning Report - 18-11-13 - Ana-LisaDocument39 pagesMorning Report - 18-11-13 - Ana-LisaYurike Natalie LengkongPas encore d'évaluation
- Aan Morning ReportDocument11 pagesAan Morning ReportImam IskandarPas encore d'évaluation
- Tuesday, July 31 TH, 2012 Supervisor: DR Sabar P Siregar SP - KJDocument44 pagesTuesday, July 31 TH, 2012 Supervisor: DR Sabar P Siregar SP - KJChristophorus RaymondPas encore d'évaluation
- 5morning Report Reagan Resadita 011014Document44 pages5morning Report Reagan Resadita 011014AnonymousssPas encore d'évaluation
- Morning: Supervisor Dr. Sabar P. Siregar, SP - KJDocument39 pagesMorning: Supervisor Dr. Sabar P. Siregar, SP - KJTasia DeastutiPas encore d'évaluation
- Tuesday, December 11th, 2012 Supervisor: DR Sabar P Siregar SP - KJDocument29 pagesTuesday, December 11th, 2012 Supervisor: DR Sabar P Siregar SP - KJCharles Hasudungan SiregarPas encore d'évaluation
- Morning Report Dels EditsDocument59 pagesMorning Report Dels EditsDella Putri Ariyani NasutionPas encore d'évaluation
- November 24 2014: MondayDocument55 pagesNovember 24 2014: MondayzakyalfaPas encore d'évaluation
- Morning: Thursday, March 19th 2015 Night ShiftDocument44 pagesMorning: Thursday, March 19th 2015 Night ShiftSakinah EceePas encore d'évaluation
- Morpot 21 SeptDocument41 pagesMorpot 21 SeptTasia DeastutiPas encore d'évaluation
- Morning Report: Friday, 20th March 2015Document37 pagesMorning Report: Friday, 20th March 2015NidaPuspitaAyuPas encore d'évaluation
- Morning Report 2017Document51 pagesMorning Report 2017udjkwPas encore d'évaluation
- MORNING REPORT 2 September 2013 (Pu Mia) NewDocument37 pagesMORNING REPORT 2 September 2013 (Pu Mia) NewWahyu AjiPas encore d'évaluation
- Morning Report 6 Aug 2012Document40 pagesMorning Report 6 Aug 2012Wilutami Rahardiyaning TyasPas encore d'évaluation
- Morning Report RevisionDocument46 pagesMorning Report RevisionKurniati HatmiPas encore d'évaluation
- Morning Report: Monday, January 26 2015Document64 pagesMorning Report: Monday, January 26 2015alvian2109Pas encore d'évaluation
- Morning: Supervisor Dr. Sabar P. Siregar, SP - KJDocument42 pagesMorning: Supervisor Dr. Sabar P. Siregar, SP - KJZahrifa Riandani PutriPas encore d'évaluation
- Morning Report 21 November 2014Document54 pagesMorning Report 21 November 2014Tiara Grhanesia DenashuryaPas encore d'évaluation
- Morning Report 11 October 2012Document37 pagesMorning Report 11 October 2012Mitha Sari IIPas encore d'évaluation
- Morning Report 13Document38 pagesMorning Report 13Charles Hasudungan SiregarPas encore d'évaluation
- Moolchand Case 01Document15 pagesMoolchand Case 01020Srishti MehtaPas encore d'évaluation
- Laporan Kasus Skizofrenia ParanoidDocument63 pagesLaporan Kasus Skizofrenia ParanoidMichi Mich100% (1)
- Morning Report 25 NovemberDocument57 pagesMorning Report 25 NovemberTiara Grhanesia DenashuryaPas encore d'évaluation
- Presentasi Kasus Non Psikotik DinnaDocument50 pagesPresentasi Kasus Non Psikotik DinnaviennnsPas encore d'évaluation
- Counselling Psychology SeminarDocument6 pagesCounselling Psychology Seminarmadhu mithaPas encore d'évaluation
- Gangguan Mental OrganikDocument19 pagesGangguan Mental Organikhaikalhj100% (1)
- Morning ReportDocument53 pagesMorning ReportTasia DeastutiPas encore d'évaluation
- Psychiatric Case Presentation: Praveenrajkumar Csu Junior InternDocument33 pagesPsychiatric Case Presentation: Praveenrajkumar Csu Junior InternRishi Du AgbugayPas encore d'évaluation
- Case StudyDocument9 pagesCase Studyapsari.mhiPas encore d'évaluation
- Lecture Case Formulation Aug 15 2016 PDFDocument18 pagesLecture Case Formulation Aug 15 2016 PDFMona ADPas encore d'évaluation
- Editan CBD Non PsychoticDocument70 pagesEditan CBD Non PsychoticviennnsPas encore d'évaluation
- Developmental DisorderDocument10 pagesDevelopmental DisorderRakesh BabuPas encore d'évaluation
- Alcohol CaseDocument6 pagesAlcohol Casepsychologist.muskanPas encore d'évaluation
- M.S.E. AlcoholDocument10 pagesM.S.E. AlcoholWillsun BhagatPas encore d'évaluation
- Case Presentation: RSJ Prof. Dr. SoerojoDocument47 pagesCase Presentation: RSJ Prof. Dr. SoerojoabinadivegaPas encore d'évaluation
- 9-Child and Adolescent PsychiatryDocument32 pages9-Child and Adolescent PsychiatryZ26Pas encore d'évaluation
- Internship ReportDocument16 pagesInternship ReportRACHANA MURALIDHAR 1833279Pas encore d'évaluation
- Adolescent Mental HealthDocument38 pagesAdolescent Mental HealthblairPas encore d'évaluation
- Bipolar Affective Disorder, Manic Episode With PsychoticDocument30 pagesBipolar Affective Disorder, Manic Episode With PsychoticCharan Pal SinghPas encore d'évaluation
- Psycho Diagnostic ReportDocument5 pagesPsycho Diagnostic ReportSmridhi Seth100% (1)
- Schizoid Personality Disorder, (The Lonely Person) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsD'EverandSchizoid Personality Disorder, (The Lonely Person) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsÉvaluation : 5 sur 5 étoiles5/5 (1)
- Emergency Trolly (Yus)Document2 pagesEmergency Trolly (Yus)Hendra SetyawanPas encore d'évaluation
- Morpot 27 MaretDocument40 pagesMorpot 27 MaretHendra SetyawanPas encore d'évaluation
- Seorang Penderita Sindrom Nefritik Akut PascaDocument7 pagesSeorang Penderita Sindrom Nefritik Akut PascaNing MaunahPas encore d'évaluation
- DislipidemiaDocument23 pagesDislipidemiaHendra SetyawanPas encore d'évaluation
- Morpot 22 Maret SoreDocument40 pagesMorpot 22 Maret SoreHendra SetyawanPas encore d'évaluation
- Monitor Tobacco Use and Prevention PoliciesDocument2 pagesMonitor Tobacco Use and Prevention PoliciesHendra SetyawanPas encore d'évaluation
- Morport Fix 17 Maret 2014 FiiiixDocument40 pagesMorport Fix 17 Maret 2014 FiiiixHendra SetyawanPas encore d'évaluation
- CPG 12Document41 pagesCPG 12AMessi YoungPas encore d'évaluation
- Morning Report: Supervisor Dr. Sabar P. Siregar, SP - KJDocument43 pagesMorning Report: Supervisor Dr. Sabar P. Siregar, SP - KJHendra SetyawanPas encore d'évaluation
- Toxic Megacolon Presentation FinalDocument33 pagesToxic Megacolon Presentation FinalHendra SetyawanPas encore d'évaluation
- Yes, Materi 16 Januari 2013Document42 pagesYes, Materi 16 Januari 2013Hendra SetyawanPas encore d'évaluation
- Publications and Documents WHO WetMarketDocument42 pagesPublications and Documents WHO WetMarketHendra SetyawanPas encore d'évaluation
- Medical Skills of Radiology - Normal Thorax & AbdomenDocument8 pagesMedical Skills of Radiology - Normal Thorax & AbdomenHendra SetyawanPas encore d'évaluation
- Trauma and Emergencies Block: HighlightDocument10 pagesTrauma and Emergencies Block: HighlightHendra SetyawanPas encore d'évaluation
- Monitor Tobacco Use and Prevention PoliciesDocument2 pagesMonitor Tobacco Use and Prevention PoliciesHendra SetyawanPas encore d'évaluation
- Trauma and Emergencies Block: HighlightDocument10 pagesTrauma and Emergencies Block: HighlightHendra SetyawanPas encore d'évaluation
- Alkes 08Document3 pagesAlkes 08Hendra SetyawanPas encore d'évaluation
- Trauma and Emergencies Block: HighlightDocument10 pagesTrauma and Emergencies Block: HighlightHendra SetyawanPas encore d'évaluation
- AgeepDocument4 pagesAgeepHendra SetyawanPas encore d'évaluation
- 5 MisoprostolDocument8 pages5 MisoprostolEko Arya SandiPas encore d'évaluation
- Medical Skills of Radiology - Normal Thorax & AbdomenDocument8 pagesMedical Skills of Radiology - Normal Thorax & AbdomenHendra SetyawanPas encore d'évaluation
- Trauma and Emergencies Block: HighlightDocument10 pagesTrauma and Emergencies Block: HighlightHendra SetyawanPas encore d'évaluation
- Medical Skills of Radiology - Normal Thorax & AbdomenDocument8 pagesMedical Skills of Radiology - Normal Thorax & AbdomenHendra SetyawanPas encore d'évaluation
- Mucoadhesive Polymers: Means of Improving Drug Delivery: MucoadhesionDocument4 pagesMucoadhesive Polymers: Means of Improving Drug Delivery: MucoadhesionBrijesh RayPas encore d'évaluation
- Atrigel A Potential Parenteral Controlled Drug Delivery SystemDocument8 pagesAtrigel A Potential Parenteral Controlled Drug Delivery SystemMaria RoswitaPas encore d'évaluation
- HDHDHDocument22 pagesHDHDHraduben5403Pas encore d'évaluation
- Practical Invertebrate AnatomyDocument2 pagesPractical Invertebrate Anatomydee.aira2955Pas encore d'évaluation
- Viva XT Brochure - 201203539IEp3Document6 pagesViva XT Brochure - 201203539IEp3Lubna LuaiPas encore d'évaluation
- Nurs 3020 FinalDocument9 pagesNurs 3020 Finalapi-240933601Pas encore d'évaluation
- PJBL 2Document2 pagesPJBL 2BeyLha Ituwh Aquh0% (2)
- B Lrs Advice PhysioDocument10 pagesB Lrs Advice PhysiodracoscribdPas encore d'évaluation
- Assessing Dehydration in ChildrenDocument40 pagesAssessing Dehydration in ChildrenDr. Jayesh PatidarPas encore d'évaluation
- L S V L C L: Ymphoma Eries: Ariants of Arge-Ell YmphomaDocument9 pagesL S V L C L: Ymphoma Eries: Ariants of Arge-Ell YmphomaRastuPas encore d'évaluation
- Bile Duct DilatedDocument4 pagesBile Duct DilatedAmit GauravPas encore d'évaluation
- 1st Anno ASMIHA 25 0k 12112015Document17 pages1st Anno ASMIHA 25 0k 12112015VeritasIIPas encore d'évaluation
- Nifedipine and Prednisone Drug StudyDocument4 pagesNifedipine and Prednisone Drug StudyJomer GonzalesPas encore d'évaluation
- Nasal Polyp DR Eva 2018Document37 pagesNasal Polyp DR Eva 2018hudaPas encore d'évaluation
- Reading Sub-Test - Question Paper: Parts B & CDocument16 pagesReading Sub-Test - Question Paper: Parts B & CShyju Paul100% (1)
- A Brief Introduction To HypnotherapyDocument10 pagesA Brief Introduction To HypnotherapyEndy MulioPas encore d'évaluation
- HyteriaDocument4 pagesHyteriaHarinderPas encore d'évaluation
- Lipobelle Soyaglycone - Dermatological Application of Soy Isoflavones To Prevent Skin Aging in Postmenopausal Women - CTMWW 2001 PDFDocument5 pagesLipobelle Soyaglycone - Dermatological Application of Soy Isoflavones To Prevent Skin Aging in Postmenopausal Women - CTMWW 2001 PDFrahulPas encore d'évaluation
- Mucocele 5Document4 pagesMucocele 5Devi Alfiani100% (1)
- Traditional Chinese MedicineDocument40 pagesTraditional Chinese MedicineDoktormin106Pas encore d'évaluation
- Application of Fascial Manipulation Technique in Chronic Shoulder PainDocument8 pagesApplication of Fascial Manipulation Technique in Chronic Shoulder PainEnyaw DroffatsPas encore d'évaluation
- Piis 1360859215001679Document6 pagesPiis 1360859215001679api-318417723Pas encore d'évaluation
- Neonatal Hyperbilirubinaemia 5.0Document25 pagesNeonatal Hyperbilirubinaemia 5.0Anca AdamPas encore d'évaluation
- Clinical Protocol by EktaDocument24 pagesClinical Protocol by EktaEkta SharmaPas encore d'évaluation
- Lester Et Al Cognitive ErrorsDocument11 pagesLester Et Al Cognitive ErrorsДоникаPas encore d'évaluation
- Positive End Expiratory PressureDocument5 pagesPositive End Expiratory PressureIrving H Torres LopezPas encore d'évaluation
- Wounds Part OneDocument15 pagesWounds Part Onemei robiwidodoPas encore d'évaluation