Académique Documents
Professionnel Documents
Culture Documents
12Lec-CNS Infections
Transféré par
Datulna Benito Mamaluba Jr.0 évaluation0% ont trouvé ce document utile (0 vote)
8 vues31 pagesfaffsfsdfgsdfwfsdfsfsfsfs
Titre original
12Lec-CNS Infections (1)
Copyright
© © All Rights Reserved
Formats disponibles
PPT, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentfaffsfsdfgsdfwfsdfsfsfsfs
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PPT, PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
8 vues31 pages12Lec-CNS Infections
Transféré par
Datulna Benito Mamaluba Jr.faffsfsdfgsdfwfsdfsfsfsfs
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PPT, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 31
MARISSA B.
LUKBAN, MD, FPPS, FPNA, FCNSP
University of the Philippines - College of Medicine
Department of Pediatrics and Neurosciences
PIDSP 19
th
Annual Convention
February 16, 2012
CNS INFECTIONS :
Spotlight on Bacterial
Meningitis
To present the epidemiological picture of
bacterial meningitis worldwide and locally
(Philippine General Hospital)
To review the clinical practice guideline on
the performance of lumbar puncture in
children with a first febrile seizures
To highlight the various ancillary tests
available in the diagnosis of bacterial
meningitis
To discuss the current recommendations on
antibiotic management of bacterial
meningitis
Objectives:
Case Fatality
Rates
Bacterial
Meningitis
A View of the
Past 90 years
(1910-2000)
Swartz, NEJM
2004
Active
Bacterial
Core
Surveillance
Whitney
NEJM 2003
Brouwer
2010
3188 pts with Bacterial Meningitis;466/3155 (14.8%) died
31% DECREASE in incidence comparing 1998-99 vs 2006-07
Median age: INCREASE from 30.3 yrs vs 41.9 yrs
Most common organism: Strep Pneumoniae, Group B Strep,
Neisseria, Hemophiluns influenze, Listeria
Thigpen NEJM 2011
Frequency Distribution of Bacterial Meningitis in
Philippine General Hospital 2002-2006
(5 year survey)
0
10
20
30
40
50
2002 2003 2004 2005 2006
HIB Pneumo Others/culture negative
0
10
20
30
40
50
2002 2003 2004 2005 2006 2010 2011
HIB Pneumo Others/culture negative
Philippne General Hospital
Department of Pediatrics
Inpatient Census (2010-2011)
Philippine General Hospital Department of
Pediatrics Inpatient Census (2011)
116 in patient admissions with meningitis
63 (54%) pts with tuberculous meningitis
46 (39% ) pts with bacterial meningitis
7 (6%) pts with viral/aseptic meningitis
Philippine General Hospital Department of
Pediatrics Inpatient Census (2011)
Diagnostic Examinations
To diagnose bacterial meningitis CSF
examination is mandatory. CSF culture
is the gold standard for diagnosis
and it is obligatory to obtain the in
vitro susceptibility of the causative
organism to rationalize treatment
Van de Beek, NEJM, 2006
PPS/PNA/CNSP 2004
Clinical Practice Guideline on the
first Febrile Seizure
Clinical Question: Among children with a first
febrile seizure, is lumbar puncture recommended
to rule out meningitis
CSF analysis is not the test that confirms the
diagnosis of febrile seizure per se
CSF analysis is the gold standard for the
alternative diagnosis of meningitis
AGE plays a crucial role in decision to do lumbar
puncture
Local Studies on the prevalence of bacterial meningitis
in children presenting with a first febrile seizure
Mangubat & Robles (East Avenue Medical Center)
Retrospective study of 198 children aged 3
months to 6 years 1% prevalence
Dilangalen & Perez (Cotabato Regional and Medical
Center)
Retrospective study of 339 children 7%
prevalence
Local Studies on the prevalence of bacterial meningitis
in children presenting with a first febrile seizure
San Nicolas & Lukban (Philippine General
Hospital)
Prospective study on validity indices of clinical
parameters in predicting lumbar puncture yield
of children with febrile seizures -11/50 (22%)
abnormal CSF suggestive of meningitis
Discrimate factors in the clinical signs and
symptoms that differentiate children with
meningitis (70% identified)
Complex febrile seizure
Fever of more than 3 days
Vomiting or drowsiness at home
Physician visit in past 48 hours
Significant Clinical Parameters
associated with Bacterial Meningitis
duration of fever of more than 3 days
the presence of anorexia, vomiting and sleep
disturbances
a physician consult within 48 hours prior to
seizures
the presence of ear discharge
abnormal neurologic findings like nuchal rigidity
and focal signs
depressed level of consciousness and
occurrence of seizures at the Emergency Room.
Philippine Clinical Practice Guideline on the first
Febrile Seizure
RECOMMENDATION STATEMENT
Lumbar puncture is strongly recommended for
children below 18 months for a first simple febrile
seizure.
For those children >/= 18 months of age, lumbar
puncture should be performed in the presence of
clinical signs of meningitis (meningeal signs,
sensorial changes)
Diagnostic Examinations:
The CSF
Relationship
between serum
and CSF glucose
is highly linear
For every
increase of 1
mg/dl of serum
glucose, CSF
glucose levels
increase by 0.56
mg/dl (95% CI
0.56-0.57 R2 0.94)
Nigrovic,
NEJM, 2012
The Cerebrospinal Fluid Exam
20 USA ER Departments 2001-2004
Antibiotic pretreatment = received within 72 hrs from LP
Rates of positive gram stain did not differ
Rates of positive CSF and blood cultures less
Not associated with total WBC and neutrophil count
Increased glucose and decreased protein content
Nigrovic 2008
Ancillary Diagnostic Examinations
Gram staining
Blood Culture
Latex Agglutination antisera
directed against capsular
polysaccharide of meningeal pathogen
PCR presence of bacterial DNA in
CSF
Skin biopsy
Serum inflammatory markers
Increased serum procalcitonin
Increased C reactive protein
Sensitivities of various diagnostic tests to
determine microbial etiologies of patients
with community acquired bacterial
meningitis
Brouwer 2010
Prognostic Factors related to Sequelae
and Poor Outcome
Presence of seizures
Low CSF glucose
High CSF protein
Absence of rash
Positive blood culture
Etiology Pneumococcal and Meningocoocal
Vasilopoulou, Greek Meningitis Registry
BMC Infectious Disease 2011
RECOMMENDATIONS ON
TREATMENT
Based on subgroups according to age and
common organisms
Guided by prevailing antibiotic susceptibility
and resistance in the region
Generics Law
Clinical setting
Malnutrition
Finances
Access to vaccination
CLINICAL
SUBGROUP
EMPIRIC THERAPY PREDOMINANT
ORGANISMS
NEONATE,
EARLY ONSET
Ampicillin 150 mkday [q8h]
plus Gentamicin 5mkday [q12h]
or Cefotaxime 100-150mkday
[q8-12] or Ceftriaxone 80-
100mkday [q12-24h]
S. Agalactiae,
E. Coli, Listeria
Monocytogenes
NEONATE,
LATE ONSET
Ampicilllin 200mkday [q6-8h]
plus Gentamycin 7.5 mkday [q
8h] or Cefotaxime 150-200
mkday [q6-8h]
S. Agalactiae, L.
monocytogenes
, Gram negative
bacilli
INFANTS AND
CHILDREN
Cefotaxime 225-300 mkday
[q6-8h] or Ceftriaxone 80-100
mkday [q12-24h] plus
vancomycin 60mkday [q6h]*
(if with high cephalosporin
resistance)
S. Pneumoniae,
N. meningitidis
CLINICAL
SUBGROUP
EMPIRIC THERAPY PREDOMINANT
ORGANISMS
ADULTS Expanded spectrum
cephalosporin plus
Vancomycin 3060 mkday
[q8-12h] *
Strep Pneumoniae,
Neisseria Meningitidis
ELDERLY AND
IMMUNO-
COMROMISED
Expanded spectrum
cephalosporin plus ampicillin
12g/day [q4h] plus
Vancomycin 30 60mkday [q
8-12h]*
S. Pneumoniae, N.
Meningitidis
L. Monocytogenes
COMMUNITY
ACQUIRED
RECURRENT
Expanded spectrum
cephalosporin plus
Vancomycin 3060 mkday
[q 8-12h]*
S. Pneumoniae, N.
Meningitidis, H.
Influenzae
NOSOCOMIAL Vancomycin 30-45 mkday [q
8-2] plus Ceftazidime 6g/day
[q 8h] or Meropenem 6g/day
[q 8h]
S. Aurerus, S
Epidermidis, aerobic
gram negative bacilli
MICROORGANISM STANDARD
THERAPY
ALTERNATIVE THERAPY
HEMOPHILUS
INFLUENZAE
B LACTAMASE (-) Ampicillin Ceftriaxone/Cefotaxime;
Cefipime;
Chloramphenicol;
Aztreonam;
Fluroquinolone
B LACTAMASE (+) Ceftriaxone/
Cefotaxime
Cefipime;
Chloramphenicol;
Aztreonam;
Fluroquinolone
BLNAR Ceftriaxone/
Cefotaxime plus
Meropenem
Ceftriaxone/Cefotaxime
plus Fluroquinolone
Brouwer 2010
MICROORGANISM STANDARD
THERAPY
ALTERNATIVE
THERAPY
STREPTOCOCCUS
PNEUMONIAE
PENICILLIN
MIC <0.1 UG/ML
Penicillin G or
Ampicilllin
Ceftriaxone/
Cefotaxime;
Chloramphenicol
PENICILLIN MIC
0.1-1.0 UG/ML
Ceftriaxone/
Cefotaxime
Meropenem;
Cefipime
PENICILLIN
MIC >2.0UG/ML
Vancomycin plus
third gen
cephalosporin
Ceftiaxone/
Cefotaxime plus
moxilocaxin
STREPTOCOCCUS
PYOGENES
Penicillin Ceftriaxone/
Cefotaxime
STREPTOCOCCUS
AGALACTIAE
Ampicillin or
Penicillin G
(may need to add
aminoglycoside)
Ceftriaxone/
Cefotaxime
Brouwer 2010
MICROORGANSIM STANDARD
THERAPY
ALTERNATIVE
THERAPY
NEISSERIA
MENINGITIDIS
PENICILLIN
MIC < 0.1 UG/ML
Penicillin G or
Ampicillin
Ceftriaxone/
Cefotaxime;
Chloramphenicol
PENCILLINE MIC 0.1-1
UG/ML
Ceftriaxone/
Cefotaxime
Chloraphenicol;
Fluroquinolone;
Meropenem
Brouwer 2010
MICROORGANISM STANDARD
THERAPY
ALTERNATIVE
THERAPY
STAPHYLOCOCCUS
AUREUS
METHICILLIN
SENSITIVE
Oxacillin or
nafcillin
Vancomycin,
Meropenem,
Linezolid,
Daptomycin
METHICILLIN
RESISTANT
Vancomycin Trimethoprim-
Sulfa; Linezolid;
Daptomycin
STAPHYLOCOCCUS
EPIDERMIDIS
Vancomycin Linezolid
Brouwer 2010
Vital Role of Pediatricians
There remains a lot to be done to
replicate the success of high-income
countries in decreasing the incidence of
bacterial meningitis thru wide spread
vaccination in resource-poor countries
like the Philippines.
There is a need for local government
initiatives to make vaccinations more
accessible to all beyond the EPI
program.
Vital Role of Pediatricians
The pediatrician is strategically
situated as he/she can act as an
advocate for the prevention of
meningitis and is the key to averting the
disastrous complications of this disease
thru early recognition and appropriate
management.
Thank you
Vous aimerez peut-être aussi
- RB Parcon Agri Industries bids for BARMM chicken raising projectDocument1 pageRB Parcon Agri Industries bids for BARMM chicken raising projectDatulna Benito Mamaluba Jr.Pas encore d'évaluation
- Letter To FB Batucan 2Document2 pagesLetter To FB Batucan 2Datulna Benito Mamaluba Jr.Pas encore d'évaluation
- Caravan 2021Document5 pagesCaravan 2021Datulna Benito Mamaluba Jr.Pas encore d'évaluation
- Total Ban On Smoking PolicyDocument2 pagesTotal Ban On Smoking PolicyDatulna Benito Mamaluba Jr.Pas encore d'évaluation
- Guidelines and Mechanics of Biggest Loser Arkcons EditionDocument1 pageGuidelines and Mechanics of Biggest Loser Arkcons EditionDatulna Benito Mamaluba Jr.Pas encore d'évaluation
- Holiday Notice (Immaculate Concepcion Day 2021)Document1 pageHoliday Notice (Immaculate Concepcion Day 2021)Datulna Benito Mamaluba Jr.Pas encore d'évaluation
- Letter To Other ContrtactorsDocument1 pageLetter To Other ContrtactorsDatulna Benito Mamaluba Jr.Pas encore d'évaluation
- 60th Birthday ProgramDocument3 pages60th Birthday ProgramDatulna Benito Mamaluba Jr.Pas encore d'évaluation
- DEED OF SALE OF MOTOR VEHICLE-templateDocument2 pagesDEED OF SALE OF MOTOR VEHICLE-templateIvy Mallari QuintoPas encore d'évaluation
- Human Resource Management and Development'S Main Functio NDocument8 pagesHuman Resource Management and Development'S Main Functio NDatulna Benito Mamaluba Jr.Pas encore d'évaluation
- R.A. - 7832 (Anti Pilferage Act of 1994)Document5 pagesR.A. - 7832 (Anti Pilferage Act of 1994)Vert WheelerPas encore d'évaluation
- Core Top 21 Science Research GuidelineDocument6 pagesCore Top 21 Science Research GuidelineDatulna Benito Mamaluba Jr.Pas encore d'évaluation
- Handbook On Workers Statutory Monetary Benefits 2020 EditionDocument80 pagesHandbook On Workers Statutory Monetary Benefits 2020 EditionDatulna Benito Mamaluba Jr.Pas encore d'évaluation
- Motivation Towards Teamwork: Datulna B. Mamaluba, JR., RcrimDocument20 pagesMotivation Towards Teamwork: Datulna B. Mamaluba, JR., RcrimDatulna Benito Mamaluba Jr.Pas encore d'évaluation
- Considerations in LifeDocument4 pagesConsiderations in LifeDatulna Benito Mamaluba Jr.Pas encore d'évaluation
- JANUARY 2020: Sun Mon Tue Wed Thu Fri SatDocument12 pagesJANUARY 2020: Sun Mon Tue Wed Thu Fri SatDatulna Benito Mamaluba Jr.Pas encore d'évaluation
- What Is A Research Journal?: Edited by A Professional Proofread Submitting Your PaperDocument3 pagesWhat Is A Research Journal?: Edited by A Professional Proofread Submitting Your PaperDatulna Benito Mamaluba Jr.Pas encore d'évaluation
- Ra 9262 Anti-Violence Against Women ActDocument14 pagesRa 9262 Anti-Violence Against Women Actapi-250425393Pas encore d'évaluation
- September 2020: Sunday Monday Tuesday Wednesday Thursday Friday SaturdayDocument1 pageSeptember 2020: Sunday Monday Tuesday Wednesday Thursday Friday SaturdayDatulna Benito Mamaluba Jr.Pas encore d'évaluation
- 2020 CalendarDocument12 pages2020 CalendarDatulna Benito Mamaluba Jr.Pas encore d'évaluation
- January 2020Document12 pagesJanuary 2020Datulna Benito Mamaluba Jr.Pas encore d'évaluation
- December 2020: Sunday Monday Tuesday Wednesday Thursday Friday SaturdayDocument1 pageDecember 2020: Sunday Monday Tuesday Wednesday Thursday Friday SaturdayDatulna Benito Mamaluba Jr.Pas encore d'évaluation
- October 2020 PDFDocument1 pageOctober 2020 PDFDatulna Benito Mamaluba Jr.Pas encore d'évaluation
- Notes:: New Year'S Day MlkingdayDocument12 pagesNotes:: New Year'S Day MlkingdayDatulna Benito Mamaluba Jr.Pas encore d'évaluation
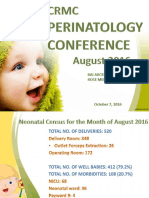
- August 2016 Perinatology Conference FinalDocument22 pagesAugust 2016 Perinatology Conference FinalDatulna Benito Mamaluba Jr.Pas encore d'évaluation
- August 2020: Sunday Monday Tuesday Wednesday Thursday Friday SaturdayDocument1 pageAugust 2020: Sunday Monday Tuesday Wednesday Thursday Friday SaturdayDatulna Benito Mamaluba Jr.Pas encore d'évaluation
- October 2020: Sunday Monday Tuesday Wednesday Thursday Friday SaturdayDocument1 pageOctober 2020: Sunday Monday Tuesday Wednesday Thursday Friday SaturdayDatulna Benito Mamaluba Jr.Pas encore d'évaluation
- June 2020 calendar with weekly viewDocument1 pageJune 2020 calendar with weekly viewDatulna Benito Mamaluba Jr.Pas encore d'évaluation
- November 2020: Sunday Monday Tuesday Wednesday Thursday Friday SaturdayDocument1 pageNovember 2020: Sunday Monday Tuesday Wednesday Thursday Friday SaturdayDatulna Benito Mamaluba Jr.Pas encore d'évaluation
- May 2020 PDFDocument1 pageMay 2020 PDFDatulna Benito Mamaluba Jr.Pas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Fitness RX For Women - April 2014Document116 pagesFitness RX For Women - April 2014Ricardo Soares100% (2)
- CT AC 72A<INV=<90A 70A<REC=<135A Part SpecDocument7 pagesCT AC 72A<INV=<90A 70A<REC=<135A Part SpecEdwin Mosos RamosPas encore d'évaluation
- Purposive Communication, Assignment 2Document3 pagesPurposive Communication, Assignment 2Myles Ninon LazoPas encore d'évaluation
- Metrology-Lab-Manual 3 Year 1semDocument41 pagesMetrology-Lab-Manual 3 Year 1semBHARATH Chandra100% (1)
- Deka Batteries PDFDocument6 pagesDeka Batteries PDFLuis Alonso Osorio MolinaPas encore d'évaluation
- Rizal 6Document11 pagesRizal 6Alexa LeePas encore d'évaluation
- Measurement of Carbon Dioxide Content: Centec Process SensorsDocument2 pagesMeasurement of Carbon Dioxide Content: Centec Process Sensorslaoying qdPas encore d'évaluation
- LADBS - Swimming PoolsDocument43 pagesLADBS - Swimming PoolsMichael James100% (1)
- Tots FaqDocument12 pagesTots FaqkbsnPas encore d'évaluation
- Manual Direct Fired 160h Through 800h PN 54000 07-12-13 - 1Document53 pagesManual Direct Fired 160h Through 800h PN 54000 07-12-13 - 1Fer YamashitaPas encore d'évaluation
- Practicing Oil AnalysisDocument62 pagesPracticing Oil AnalysisCristian SPas encore d'évaluation
- Gross Examination LabmedDocument2 pagesGross Examination Labmediishayati100% (1)
- 200 300 Series Installation Guide USDocument48 pages200 300 Series Installation Guide USLhexter Mhervin CoPas encore d'évaluation
- A History of OrnamentDocument488 pagesA History of OrnamentBrad Sommers100% (12)
- Bagi Exercise Listening and StructureDocument16 pagesBagi Exercise Listening and StructureDwiva Muna100% (1)
- Biology 5th Brooker Test BankDocument34 pagesBiology 5th Brooker Test BankRamiqq67% (3)
- Brother Printer GT-782Document126 pagesBrother Printer GT-782vitprint22Pas encore d'évaluation
- Spraying TechniquesDocument12 pagesSpraying TechniquesX800XLPas encore d'évaluation
- Chapter 16 Magnetic Fields: Electricity and MagnetismDocument11 pagesChapter 16 Magnetic Fields: Electricity and MagnetismeltytanPas encore d'évaluation
- Astm D 2113-14Document20 pagesAstm D 2113-14aswathy annie varghesePas encore d'évaluation
- Working Principle Iwind Wind TurbinesDocument25 pagesWorking Principle Iwind Wind TurbinesKarbonKalePas encore d'évaluation
- Business Operations Group AssignmentDocument7 pagesBusiness Operations Group Assignmentankit gangelePas encore d'évaluation
- Worksheet Modul 6 - Food and Beverage DivisiondDocument10 pagesWorksheet Modul 6 - Food and Beverage DivisiondIAN WIDJAYAPas encore d'évaluation
- C70Document3 pagesC70Jorge Luis Arevalo LopezPas encore d'évaluation
- Cat Marine Engine ProgramDocument4 pagesCat Marine Engine ProgramRobert BeddingfieldPas encore d'évaluation
- Statepfofileofvidarbha PDFDocument53 pagesStatepfofileofvidarbha PDFAditiPas encore d'évaluation
- D3.6.SmartAKIS - Recommendations Danemarca Cu SiteDocument47 pagesD3.6.SmartAKIS - Recommendations Danemarca Cu SitebubuhomePas encore d'évaluation
- CEEAMA-TECHNICAL-PAPER-2018 by Sunil VoraDocument6 pagesCEEAMA-TECHNICAL-PAPER-2018 by Sunil VorasunilgvoraPas encore d'évaluation
- Moral vs Non-Moral Standards ExplainedDocument2 pagesMoral vs Non-Moral Standards ExplainedLee PascuaPas encore d'évaluation