Académique Documents
Professionnel Documents
Culture Documents
Lipids and Dyslipoproteinemia Nov 2012 Lab Diagnosis
Transféré par
micheal19600 évaluation0% ont trouvé ce document utile (0 vote)
30 vues39 pagesPlasma lipoproteins-transport cholesterol and esterified lipids in the blood. Large particles produced by intestine rich in triglycerides of exogenous origin. Chylomicrons accumulate as a floating creamy layer when left undisturbed for several hours.
Description originale:
Copyright
© © All Rights Reserved
Formats disponibles
PPT, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentPlasma lipoproteins-transport cholesterol and esterified lipids in the blood. Large particles produced by intestine rich in triglycerides of exogenous origin. Chylomicrons accumulate as a floating creamy layer when left undisturbed for several hours.
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PPT, PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
30 vues39 pagesLipids and Dyslipoproteinemia Nov 2012 Lab Diagnosis
Transféré par
micheal1960Plasma lipoproteins-transport cholesterol and esterified lipids in the blood. Large particles produced by intestine rich in triglycerides of exogenous origin. Chylomicrons accumulate as a floating creamy layer when left undisturbed for several hours.
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PPT, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 39
OUTLINE:
I.LIPOPROTEINS, APOLIPOPROTEINS &
RELATED PROTEINS
II.LIPID TRANSPORT AND LIPOPROTEIN
METABOLISM
III. LIPID AND LIPOPROTEIN
MEASUREMENT
IV. THE NCEP GUIDELINES
V. LIPIDS, LIPOPROTEINS AND DISEASE
Plasma lipoproteins-transport cholesterol and
esterified lipids in the blood.
4 major lipoproteins
Chylomicrons, VLDL, LDL, HDL, IDL
Apolipoproteins-play impt.roles in lipid
transport by activating or inhibiting enzymes
involved in lipid metabolism, binding
lipoproteins to cell surface lipoprotein
receptors or both.
Large particles produced by intestine rich in
triglycerides of exogenous origin and
relatively poor in free cholesterol and
phospholipids
Contain 1-2% protein
Less dense than water/floats even w/o
centrifugation due to its high lipid/protein
High chylomicron content results in milky
plasma in w/c chylomicrons accumulate as a
floating creamy layer when left undisturbed
for several hours. Apo-B48,apoA-I, IV;apoC-
I,II,III,apoE
Smaller than chylomicrons; rich in triglycerides
Lower lipid/protein ratio; float at higher density
Like chylomicrons, particles are large enough to
scatter light; w/excessive VLDL, plasma is turbid.
VLDL Triglycerides are endogenous, mainly
hepatic origin and constitute half the particle
mass.
Cholesterol and phospholipids 40% of particle
10% is protein apoB-100 and apo-C; apoE
Smaller particles poorer in 2 components
50% of total lipoprotein mass in plasma.
Smaller than TG-rich lipoproteins
Cholesterol-1/2 of LDL
25% of LDL mass is protein, apoB-100 with
traces of apoC
Small particles (50% protein) apoA-1, apoA-II
but also apoC & apoE; 20% cholesterol
(mostly esterified); 30% phospholipids & TG
traces.
HDL2 and HDL3 (differ in density, particle
size and composition)
Density range 1.055-1.085 kg/L
27% protein, 65% lipid, 8% CHO so like LDL
but in lower concentrations.
apoB, apo(a) bound thru disulfide bonds
LpX Lipoprotein
-abnormal lipoprotein found in patients with
obstructive biliary disease.
Lipids more than 90% of weight (phospholipids,
unesterified chole, little esterified chole)
B-VLDL (floating B lipoprotein) abN protein that
accum. In Type III hyperlipopoteinemia
ApoA
ApoA-I is 75% of apo of HDL; synthesized in the
liver and intestine; activates lecithin cholesterol
acyl transferase (LCAT) which esterifies
cholesterol.
ApoA-II is 20% of apo of HDL; 2 identical
peptides linked by one disulfide bond. Unknown
role
ApoB-major protein 95% of LDL; 40% of protein
of VLDL and chylomicrons. Major component is
apoB-100; synthesized by liver; found in
endogenous lipoproteins; one of d longest
ApoC-major protein component of VLDL;
minor constituent of HDL & LDL. ApoC-I-III
Minor lipoproteins- ApoD-minor constituent
of HDL protein (5% or less). Unknown function
but may be a cofactor for LCAT.
ApoE-arginine-rich apolipoprotein; found in
VLDL, IDL, remnant lipoproteins,
chylomicrons and HDL.
Lipolytic enzymes: 2 triglyceride hydrolases
(lipoprotein lipase LPL and hepatic
triglyceride lipase) found in post-heparin
plasma.
LPL: derived from adipose tissue; hydrolyzes
TG in chylomicrons and VLDL; located on the
surface of capillary endothelial cells of
adipose tissue and skeletal & heart muscles.
Chylomicron TG is hydrolyzed ff attachment
of these particles to capillary endothelial
cells.
PL & apoC-II are cofactors for TG hydrolysis by
LPL.
Hepatic TG lipase (HTGL)-secreted by
hepatocytes; assoc. with surface membrane
of nonparenchymal liver cells. Limited
capacity to hydrolyze TG in chylomicrons &
VLDL; not require apoC-II as cofactor. May
participate in conversion of VLDL remnants
and IDL to LDL. Most active in hydrolysis of PL
& TG of HDL and may play a role in HDL
metabolism.
LCAT-catalyzes the esterification of
cholesterol by promoting transfer of FA from
lecithin to cholesterol w/c results in the
formation of lysolecithin and cholesterol
ester; synthesized in the liver & circulates in
plasma assoc. with HDL.
Lipid Transport in Lipoproteins: Transport of
TG and chole from sites of origin in intestine
(exogenous) and the liver (endogenous) to
sites of energy storage and utilization.
TG & chole enter plasma as TG-rich
lipoprotein particles (chylomicrons & VLDL)
that supply tissues with FA for energy reqts
and storage.
Chylomicrons & VLDL undergo intravascular
change almost immed.after their entry into the
circulation thru the action of lipoprotein
lipase.
LDL-2/3 removed via hepatic LDL-receptors
HDL-secreted from liver and intestine as disk-
shaped particles that contain cholesterol and
phospholipid; thought to be vehicle for reverse
chole transport where excess chole is removed
from tissues peripheral to the liver &
transported back to the liver for reuse or
disposal in the bile.
Component CVp (%) CVp (%)
Total Cholesterol 5.0 6.4
Triglycerides 17.8 23.7
LDL-cholesterol 7.8 8.2
HDL-cholesterol 7.1 7.5
ApoA-1 7.1 --
ApoB 6.4 --
Cholesterol-all of sterol in plasma; mixture of
unesterified (30-40%) & esterified (60-70%)
Enzymatic Methods-less subject to interference
by nonsterol substances;
not absolutely specific for cholesterol coz chole
oxidase can react w/other sterol.
Reducing subs. Like ascorbic acid and bilirubin
can interfere w/measurements by consuming
H2O2.
Bili may react w/an intermed. in the peroxidase
reaction.
Turbidity (inc.TG) can interfere.
Uric acid, Hgb and other subs. not affect chole.
Formaldehyde: reaction w/sulf.acid soln of
chromotropic acid to produce pink chromophore.
Peroxidate oxidation not specific for glycerol.
a-glycerophosphate oxidized by periodate to form
formaldehyde.
Enzymatic methods: specific, rapid and easy to use.
Directly in plasma or serum; not subj to interference
by PL or glucose.
TG are hydrolyzed and glycerol formed is converted
to glycerophosphate and measured. Rgts are
commercially available as lyophilized prepns still for
reconstitution.
TG blanks: Free glycerol interfere w/enzymatic
method
Omits hydrolysis step. Use for standardization &QC of
TG
Phosphatidyl choline and sphingomyelin
90% of PL & 80% of this is phosphatidyl choline.
Others: phosphatidyl serine & ethanolamine
Dses: obstructive jaundice, a/hypo
betalipoproteinemia, Tangier dse or LCAT
def.
Where conc., composition or LP distr. of PL
Released phosphate converted to
phosphomolybdate by rxn w/ammonium
molybdate & mixture is treated w/mild
reducing agent.
Ultracentrifugal methods: Lipid content w/ lower
densities than other plasma macromolecules.
Different densities so chylomicrons and VLDL
float at plasma density
LDL&HDL sedimented.
Analytical ultracentrifugation: reference method,
rates of flotation under specific cond
Prep.ultracentrif: separated at diff.densities
Electrophoretic methods: Support med. Is
agarose gel due to speed, sensi & resolution
Migration rates HDL, VLDL, LDL
Lipid-staining dye Oil Red O, fat red 7B or Sudan
BlackB
React w/ester bonds in TG & cholesteryl esters.
Polyanion precipitation methods: Heparin
sulfate, dextran sulfate, phosphotungstate
in(+)of Ca,Mg, Mn.
Influenced by rgt conc, pH, ionic strength,
(+)serum proteins and anticoag, relative amts
of lipid&protein in LP particles & duration and
conds of sample storage.
Not gained wide acceptance
MC used to remove apoB-cont. LP prior to
analysis of HDL-chole.
ApoB-cont. LP (chylomicrons, VLDL, IDL, LDL,
Lp(a)) are removed by polyanion-divalent cation
precipitation &HDL-chole is analyzed directly in
the supernatant.
Combined methods: Hyperlipidemic to measure
plasma chole, VLDL, LDL, HDL, TG
Assessment if w/chylomicrons in fasting state, (+)
or (-)B-VLDL seen in Type III hyperlipoprot.
Lp(a) indep. Risk factor for coronary dse.
Combi of preparative ultracentrif, polyanion precip,
& electrophoresis.
Plasma Total Chole, HDL-chole, TG
1. HDL-chole: direct measurement
2. LDL-chole = infranatant chole HDL-chole
3. VLDL-chole = TC infranatant chole
4. LDL-chole = TC HDL-chole Plasma TG
2.175
VLDL-chole = plasma TG
2.175
Plasma TG
6.5
Standing plasma test: for chylomicrons
Floating ice cream layer and detected visually
Plasma sample turbid after standing overnight
has VLDL so if (+) so chylomicrons are
present
Detection of B-VLDL and Lp(a):
electrophoretically examined for B-VLDL
(floating b-lipo)
VLDL-chole/plasma ratio
Consistent
with
Analyte Total Error Bias CV
Cholesterol Less than 9% Less than 3% Less than 3%
TG Less than 15% Less than 5% Less than 5%
HDL-chole Less than 22% Less than 10% Less than 6%
1. Unlike chole, none of these analytes has
unique chem. structure.
2. In the case of LDL, clinical & epid. Database
in w/c estimates of coronary risk are based
are estab. using either combined
ultracentrifug.-polyanion precipn of
Friedewald methods, HDL method is heparin
Mn procedure,
3. Either combi method or Friedewald equation,
some non-LDL LP primarily IDL &Lp(a) are
atherogenic.
Fasting, posture, venous occlusion,
anticoagulants, recent MI, stroke, cardiac
catheterization, trauma, acute infection,
pregnancy.
Total Chole
Desirable less than 200 mg/dL
Borderline High 200-239
High more than 240
HDL-chole
Low HDL-chole less than 35
1. NCEP Lab Standardization Panel
recommendations for chole used separate
specifications for bias and precision (CV) &
consistent w/total error of 8.9% or less. Set
in single value, total error considers both
bias & imprecision at the same time.
% total error = % bias + 1.96 (% CV)
2. Recom. HDL-chole apply to levels of 42
mg/dL
3. More rigorous guidelines for HDL-chole for
adoption provided that HDL-chole
measurement method is available.
Diet Therapy
Init. Level LDL Goal
W/o CHD &*fewer
than 2 risk factors more 160 less 160
W/o CHD w/2 or few more 130 less 130
W/ CHD more 100 less 100
Drug Tx
W/o CHD fewer
than 2 risk factors more 190 less 160
W/o CHD & 2 or more more 160 less 130
W/ CHD more 130 less 100
1. Apolipoprotein immunoassays
2. Radioimmunoassay (RIA)
3. Radial immunodiffusion (RID)
4. Electroimmunoassay
5. Immunonephelometry
6. Enzyme-linked (ELISA) & Fluorescence
Immunoassay
7. Probs with (1)
Qualitative apolipoprotein analysis
Simple immunodiffusion technique can
determine (+) or (-) of apolipoprotein
Evaluation of LP disorders where particular
apoLP may not be present (Tangier,
abetalipo, apoC-II deficiency
Gel electrophoresis techniques; isoelectric
focusing (separates by charge).
Total chole
Desirable blood chole less than 200 mg/dL
Borderline-high blood chole 200-239
High-blood chole more than 240
HDL-chole
Low HDL-chole less than 35
Positive risk factors
Age Male more than 45 Female more 55yo or
premature menopause w/o ERT
Family Hx of prem. CHD (defin MI or sudden
death before 55yo in father or other male first-
degree relative
Current cigarette smoking
HPN (more than 140/90 mmHg on antiHPNsive
meds
Low HDL-chole (more than 35mg/dL)
DM
Negative risk factor High HDL-chole (more than
60)
Category TC (mg/dL) LDL-chole (mg/dL)
Acceptable Less than 170 Less than 110
Borderline 170-199 110-129
High More than 200 More than 130
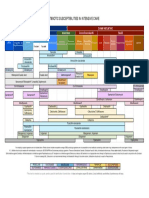
LP
Phenotype
Prem.CAD Xanthomas Pancrea
titis
I. Disorders in exog.
LP pathway
A.Defective or absent
LPL
I No Eruptive Yes
B.def.of apoLP C-II I or V No Eruptive Yes
II.Disorders of
endog,LP
A.Familial combined
hyperlipidemia
IIa, IIIB, IV
rarely V
Yes Isolated
xanthelasma
Rarely
1. Hyperapobeta-
Lpnemi
B.Familial hyperTG
N, IV Yes same No
IV, occ IIb Can occur No
(occ.eruptiv
e)
Occ.
LP
Phenotype
Prem.CAD Xanthomas Pancrea
titis
C.Familial hyperchole Iia (occ. Iib) Yes Tendon,
tuberous
No
D. Familial defective
apoB-100
N, IIa Yes Occ. tendon No
III. Disorders of both
exo & endo LP
pathway
A. Type V
hyperLPnemia
V Can occur Eruptive Yes
B.DysLPtenemia
(Type III)
III Yes Yes No
C.Def,pf apoB-cont
LP
1.AbetaLP/Hypo Hypo or
abeta
No No
LP
Phenotype
Prem.CAD Xanthomas Pancrea
titis
IV. Disorders of
reverse chole
transport pathway
A. Dec.HDL synthesis Hypo a Yes Planar No
B. Inc.HDL
catabolism
1.ApoLP A-1
variants
Hypo a No No No
2. Tangier disease Hypo a Can occur No No
C.LCAT deficiency Hypo a Can occur No No
D.CETP def Hyper Decreased No No
Although ultracentrifugation and
electrophoretic techniques are of historical
significance, most useful lipid and lipoprotein
testing methods are now enzymatic.
Low-density lipoprotein cholesterol can be
measured directly but is usually calculated
using the Friedewald formula.
Calculated values require evaluation of
fasting samples.
Low-density lipoprotein cholesterol is
currently considered the most important
value in assessing cardiac risk and directing
therapy.
The profile currently recommended for initial
screening in adults, age 20 or older, includes
total cholesterol, LDL, HDL cholesterol, and
triglycerides. Testing should be repeated
at least once every 5 years.
Other tests, including apolipoprotein levels
and lipoprotein subclasses,may prove
valuable in fine-tuning risk assessment and
evaluating response to therapy.
New guidelines elevate the perceived
atherosclerotic risk of diabetes and support
aggressive intervention in diabetic patients
and patients with metabolic syndrome.
Vous aimerez peut-être aussi
- Kid StonesDocument5 pagesKid Stonesmicheal1960Pas encore d'évaluation
- A Better Test Than HbA1c Oct 19, 2016Document5 pagesA Better Test Than HbA1c Oct 19, 2016micheal1960Pas encore d'évaluation
- MBF2306162Document137 pagesMBF2306162DrHassan Ahmed ShaikhPas encore d'évaluation
- Tests Distinguish Pneumonia Types in MinutesDocument3 pagesTests Distinguish Pneumonia Types in Minutesmicheal1960100% (1)
- Lipid Lowering With Statin Is Better Than Adding Other AgentDocument1 pageLipid Lowering With Statin Is Better Than Adding Other Agentmicheal1960Pas encore d'évaluation
- Normal ValuesDocument6 pagesNormal ValuesMc Crister SilangPas encore d'évaluation
- Taylors.10 Minute - Diagnosis.manual - Symptoms.and - Signs.in - The.time Limited - Encounter.Document656 pagesTaylors.10 Minute - Diagnosis.manual - Symptoms.and - Signs.in - The.time Limited - Encounter.micheal1960Pas encore d'évaluation
- Normal ValuesDocument6 pagesNormal ValuesMc Crister SilangPas encore d'évaluation
- AKI MGMT 2005-11-1 AAFP p1739Document8 pagesAKI MGMT 2005-11-1 AAFP p1739micheal1960Pas encore d'évaluation
- New Guidelines On Nonstatin Lipid Lowering 2016-8-16Document7 pagesNew Guidelines On Nonstatin Lipid Lowering 2016-8-16micheal1960Pas encore d'évaluation
- Simple Depression Anxiety 2 Simple Screenin QuestionsDocument2 pagesSimple Depression Anxiety 2 Simple Screenin Questionsmicheal1960Pas encore d'évaluation
- Nail Diseases, Hand in Diagnosis, Terry's NailDocument35 pagesNail Diseases, Hand in Diagnosis, Terry's Nailmicheal1960Pas encore d'évaluation
- ABX Common Effects of Antibiotics On Other Drugs MMDocument3 pagesABX Common Effects of Antibiotics On Other Drugs MMmicheal1960Pas encore d'évaluation
- Serotonin SyndromeDocument5 pagesSerotonin Syndromemicheal1960Pas encore d'évaluation
- Anal Cancer 2016-2-9Document17 pagesAnal Cancer 2016-2-9micheal1960Pas encore d'évaluation
- Low SodiumDocument4 pagesLow Sodiummicheal1960Pas encore d'évaluation
- Ezetimibe Simvastatin Post-Acute Coronary SyndromeDocument12 pagesEzetimibe Simvastatin Post-Acute Coronary Syndromemicheal1960Pas encore d'évaluation
- Trigeminal N Tables SummaryDocument14 pagesTrigeminal N Tables Summarymicheal1960Pas encore d'évaluation
- RaynaudDocument11 pagesRaynaudmicheal1960Pas encore d'évaluation
- Cold Agglutinin Disease 2015-4-28Document9 pagesCold Agglutinin Disease 2015-4-28micheal1960Pas encore d'évaluation
- 13 Can'T-Miss Findings On Pediatric Imaging 2015-12-2Document29 pages13 Can'T-Miss Findings On Pediatric Imaging 2015-12-2micheal1960Pas encore d'évaluation
- Iron Deficiency Anemia 2007-3-1 AAFP p671Document8 pagesIron Deficiency Anemia 2007-3-1 AAFP p671micheal1960Pas encore d'évaluation
- Rheumatoid Arthritis 2015-6-9Document22 pagesRheumatoid Arthritis 2015-6-9micheal1960Pas encore d'évaluation
- Clinical Challenge Bright Plaques, Papules On The ThumbDocument4 pagesClinical Challenge Bright Plaques, Papules On The Thumbmicheal1960Pas encore d'évaluation
- Athlete's Heart or Cardiomyopathy 2016-3-1Document2 pagesAthlete's Heart or Cardiomyopathy 2016-3-1micheal1960Pas encore d'évaluation
- AF & Oral Anticoagulants 2016Document11 pagesAF & Oral Anticoagulants 2016micheal1960100% (1)
- Prostate Cancer 2015-5-7Document27 pagesProstate Cancer 2015-5-7micheal1960Pas encore d'évaluation
- RaynaudDocument11 pagesRaynaudmicheal1960Pas encore d'évaluation
- Superficial Venous Insufficiency 2015-6-4Document16 pagesSuperficial Venous Insufficiency 2015-6-4micheal1960Pas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Fundamentals of Occlusion and Restorative DentistryDocument9 pagesFundamentals of Occlusion and Restorative Dentistrypablo_elguezábalPas encore d'évaluation
- JUSTINE Medical-for-Athletes-2-1Document2 pagesJUSTINE Medical-for-Athletes-2-1joselito papa100% (1)
- 4400 SystemDocument24 pages4400 SystemRaniel Aris LigsayPas encore d'évaluation
- Feasibility of Malunggay & Coconut Vinegar as Natural Cleaning AgentDocument7 pagesFeasibility of Malunggay & Coconut Vinegar as Natural Cleaning AgentCharles Dave AvenidoPas encore d'évaluation
- Case Control Study For MedicDocument41 pagesCase Control Study For Medicnunu ahmedPas encore d'évaluation
- Nursing Interventions for Ineffective Airway ClearanceDocument3 pagesNursing Interventions for Ineffective Airway Clearanceaurezea100% (3)
- SGLGB Form 1 Barangay ProfileDocument3 pagesSGLGB Form 1 Barangay ProfileMark Lenon Par Mapaye100% (1)
- Pit VeriscolorDocument5 pagesPit VeriscolorNida Fithria FadhilaPas encore d'évaluation
- Detailed Advertisement of Various GR B & C 2023 - 0 PDFDocument47 pagesDetailed Advertisement of Various GR B & C 2023 - 0 PDFMukul KostaPas encore d'évaluation
- List of Pakistani Government Ministries and DivisionsDocument2 pagesList of Pakistani Government Ministries and DivisionsbasitaleePas encore d'évaluation
- Acute Tracheobronchitis Causes, Symptoms, TreatmentDocument2 pagesAcute Tracheobronchitis Causes, Symptoms, TreatmentNicole Shannon CariñoPas encore d'évaluation
- Veritas D1.3.1Document272 pagesVeritas D1.3.1gkoutPas encore d'évaluation
- 'No Evidence That CT Scans, X-Rays Cause Cancer' - Medical News TodayDocument3 pages'No Evidence That CT Scans, X-Rays Cause Cancer' - Medical News TodayDr-Aditya ChauhanPas encore d'évaluation
- Transmission Substation Work Practice Manual 2016-07-22Document499 pagesTransmission Substation Work Practice Manual 2016-07-22Edmund YoongPas encore d'évaluation
- Revision in Obstetrics&Gynecology Revision in Obstetrics&GynecologyDocument136 pagesRevision in Obstetrics&Gynecology Revision in Obstetrics&GynecologySiam Weng Loong100% (3)
- Ijspt 10 734 PDFDocument14 pagesIjspt 10 734 PDFasmaPas encore d'évaluation
- Management of Class I Type 3 Malocclusion Using Simple Removable AppliancesDocument5 pagesManagement of Class I Type 3 Malocclusion Using Simple Removable AppliancesMuthia DewiPas encore d'évaluation
- Stressors and Coping Mechanisms of Psychologically Distressed MSU-IIT StudentsDocument22 pagesStressors and Coping Mechanisms of Psychologically Distressed MSU-IIT StudentsDarleen Rizel CalumbaPas encore d'évaluation
- Diagram Alir Dan Deskripsi Proses: Tugas 4Document11 pagesDiagram Alir Dan Deskripsi Proses: Tugas 4FevitaPas encore d'évaluation
- Design and Estimation of Rain Water Harvesting Scheme in VIVA Institute of TechnologyDocument4 pagesDesign and Estimation of Rain Water Harvesting Scheme in VIVA Institute of TechnologyVIVA-TECH IJRIPas encore d'évaluation
- Above Knee Amputation Exc PDFDocument5 pagesAbove Knee Amputation Exc PDFSenthilkumar ThiyagarajanPas encore d'évaluation
- ICU antibiotic susceptibilities guideDocument1 pageICU antibiotic susceptibilities guideFaisal Reza AdiebPas encore d'évaluation
- Home Economics LiteracyDocument43 pagesHome Economics LiteracyAndrea Fidel Raymundo100% (3)
- Autism Case Report on 3-Year-Old MaleDocument24 pagesAutism Case Report on 3-Year-Old MaleMichael John CanoyPas encore d'évaluation
- Labcorp: Patient ReportDocument4 pagesLabcorp: Patient ReportAsad PrincePas encore d'évaluation
- TMH ResumeDocument2 pagesTMH Resumeapi-257873078Pas encore d'évaluation
- Case Report: Communication Strategies For Empowering and Protecting ChildrenDocument9 pagesCase Report: Communication Strategies For Empowering and Protecting ChildrennabilahPas encore d'évaluation
- GIGITAN ULAR BERBISA: GEJALA, PENANGANAN DAN JENIS ULAR PALING BERBISADocument19 pagesGIGITAN ULAR BERBISA: GEJALA, PENANGANAN DAN JENIS ULAR PALING BERBISAYudhistira ArifPas encore d'évaluation
- Gurr2011-Probleme Psihologice Dupa Atac CerebralDocument9 pagesGurr2011-Probleme Psihologice Dupa Atac CerebralPaulPas encore d'évaluation
- Pediatric PharmacotherapyDocument4 pagesPediatric PharmacotherapyRiriPas encore d'évaluation