Académique Documents
Professionnel Documents
Culture Documents
Blood Transfusion
Transféré par
rodelagapitoTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Blood Transfusion
Transféré par
rodelagapitoDroits d'auteur :
Formats disponibles
Medicine: 41 items Pedaitric: 55
Anemia: 8 items
Bleeding: 8 items
Malignancy: 8 items
Polycythemia: 2 Items
Hypercoagulable: 6 items
Blood transfusion 6 items
Stem Cell: 3 items
Anemia: 12 items
Bleeding: 12 items
Malignancy: 12 items
Polycythemia: 3 items
Hypercoagulable : 4 items
Blood transfusion: 7 items
Stem Cell: 3 items
Public Health 6 items
BLOOD TRANSFUSION
AND TRANSFUSION
REACTION
BLOOD SELECTION
Blood Groups
Phenotype
(blood Type)
Genotyp
e
Antibodies
present in the
blood serum
A
I
A
I
A
Or
I
A
I
Anti B
B
I
B
I
B
Or
I
B
I
Anti A
AB I
A
I
B
-
O ii Anti A and B
Blood Groups
Rh group Rh antigen Rh antibody
Rh positive None
Rh negative Anti- D
Selection of Blood
Red cell transfusion
There must be ABO and Rh D
compatibility between the donors red
cells and the recipients plasma.
Group A individuals can receive blood from
Group A and O donors
Group B individuals can receive blood from
Group B and O donors
World Health Organization: Blood Transfusion Safety
Selection of Blood
Red cell transfusion
There must be ABO and Rh D
compatibility between the donors red
cells and the recipients plasma.
Group O individuals can receive blood from
Group O donors only
Group AB individuals can receive blood from
Group AB donors, and also from Group A, B
and O donors
World Health Organization: Blood Transfusion Safety
Selection of Blood
Plasma and Components containing
Plasma
In plasma transfusion, group AB plasma
can be given to a patient of any ABO
group because it contains neither anti-A
nor anti-B antibody
Group AB plasma (no antibodies) can be given
to any ABO group patients
Group O plasma (anti-A + anti-B) can be given
to Group O patients only
World Health Organization: Blood Transfusion Safety
Selection of Blood
Plasma and Components containing
Plasma
In plasma transfusion, group AB plasma
can be given to a patient of any ABO
group because it contains neither anti-A
nor anti-B antibody
Group A plasma (anti-B) can be given to Group
O and A patients
Group B plasma (anti-A) can be given to Group
O and B patients
World Health Organization: Blood Transfusion Safety
BLOOD TRANSFUSION
Blood Transfusion Practice
THE DECISION to transfuse, like any
other
therapeutic decision, should be based
on
the risks, benefits, and alternatives of
treatment.
PRINCIPLES OF CLINICAL
TRANSFUSION PRACTICE
Transfusion is only one
part of the patients
management.
Prescribing should be
based on national
guidelines on the clinical
use of blood, taking
individual patient needs
into account.
Blood loss should be
minimized to reduce the
patients need for
transfusion.
The patient with acute
blood loss should receive
effective resuscitation
(intravenous replacement
fluids, oxygen, etc.) while
the need for transfusion is
being assessed
Transfusion should be
prescribed only when the
benefits to the patient are
likely to outweigh the risks.
PRINCIPLES OF CLINICAL
TRANSFUSION PRACTICE
The patients haemoglobin
value, although important,
should not be the sole
deciding factor in starting
transfusion. This decision
should be supported by the
need to relieve clinical
signs and symptoms and
prevent significant
morbidity or mortality
The clinician should be
aware of the risks of
transfusion-transmissible
infections in the blood
products that are available
for the individual patient.
The clinician should record
the reason for transfusion
clearly.
Blood Products
(Definition of Terms)
Blood product
Whole blood
Any therapeutic substance
prepared from human blood
Unseparated blood collected
into an approved container
containing an anticoagulant-
preservative solution
Blood Products
(Definition of Terms)
Blood
component
A constituent of blood,
separated from whole blood,
such as:
Red cell concentrate
Red cell suspension
Plasma
Platelet concentrates
Plasma or platelets collected
by apheresis
Cryoprecipitate, prepared from
fresh frozen plasma: rich in
Factor VIII and fibrinogen
Blood Products
(Definition of Terms)
Plasma
derivative
Human plasma proteins
prepared under pharmaceutical
manufacturing conditions, such
as:
Albumin
Coagulation factor
concentrates
Immunoglobulins
RED CELL
TRANSFUSION
WHOLE BLOOD
(450 ml whole blood donation contains:)
Description Up to 510 ml total volume
(volume may vary in
accordance with local policies)
450 ml donor blood
63 ml anticoagulant-
preservative solution
Hgb approximately: 12 g/ml
Haematocrit: 35%45%
No functional platelets
No labile coagulation factors
(V and VIII)
WHOLE BLOOD
(450 ml whole blood donation contains:)
Infection risk Not sterilized, so capable of
transmitting any agent present
in cells or plasma which has
not been detected by routine
screening for transfusion-
transmissible infections,
including HIV-1 and HIV-2,
Hepatitis B and C, other
hepatitis viruses, syphilis,
malaria and Chagas disease
WHOLE BLOOD
(450 ml whole blood donation contains:)
Indications
Contraindication
s
Red cell replacement in Acute
Blood Loss with Hypovolaemia
Exchange transfusion
Patients needing red cell
transfusions where red cell
concentrates or suspensions
are not available
Risk of volume overload in
patients with:
Chronic anaemia
Incipient cardiac failure
Ideal component for patients who have
sustained acute hemorrhage of 25% total
blood volume loss
Provides both oxygen-carrying capacity
and volume expansion.
WHOLE BLOOD
(450 ml whole blood donation contains:)
Administration Must be ABO and RhD
compatible with the recipient
Never add medication to a unit
of blood
Complete transfusion within 4
hours of commencement
Transfusion should be started
within 30 minutes of removal
from refrigerator
RED CELL CONCENTRATE
(Packed red cells, plasma-reduced
blood)
Description 150200 ml red cells from
which most of the plasma has
been removed
Hgb approximately: 20 g/100
ml (not less than 45 g per unit)
Haematocrit: 55%75%
RED CELL CONCENTRATE
(Packed red cells, plasma-reduced
blood)
Infection risk
Storage
Indications
Administration
Same as whole blood
Same as whole blood
Replacement of red cells in
anaemic patients
Use with crystalloid
replacement fluids or colloid
solution in acute blood loss
Same as whole blood
RED CELL CONCENTRATE
(Packed red cells, plasma-reduced
blood)
3 mL PRBC/kg will raise
Hb by approximately 1 gm/dl
Hct by approximately 3%
In normal sized adult (70 kg) 1 unit
PRBC will raise the
Hct by 3 - 4% or 1 gm/dl
RED CELL CONCENTRATE
(Packed red cells, plasma-reduced
blood)
Exchange transfusion
Term infants -- 80-160ml/kg
Preterm infants -- 100-200ml/kg
Routine (neonates and children)
10-20 ml/kg
Desired Hct actual Hct x weight (kg)
Desired Hb actual Hb x weight (kg) x 3
Red Cell Transfusion
Increases oxygen-carrying capacity in
the anemic patient.
Adequate oxygenation can be
maintained with a Hemoglobin content of
70 g/L in the normo-volemic patient
without cardiac disease;
Co-morbid factors often necessitate
transfusion at a higher threshold
Red Cell Transfusion
The decision to transfuse should be
guided by the clinical situation and not by
an arbitrary laboratory value.
In the critical care setting,
Liberal use of transfusions to maintain near-
normal levels of hemoglobin may have
unexpected negative effects on survival.
In most patients requiring transfusion
Levels of hemoglobin of 100 g/L are sufficient
to keep oxygen supply from being critically
low.
Red Cell Transfusion
(Pediatric)
Transfusions may be given more
stringently to children because:
Normal hemoglobin levels are lower in
healthy children than in adults
Children do not have the underlying
cardiorespiratory and vascular diseases
that develop with aging in adults.
Red Cell Transfusion
(Pediatric)
Children should be better able to
compensate for RBC loss.
In the peri-operative period, for example,
it is unnecessary for most children to
maintain hemoglobin levels of 80 g/L or
greater, a level frequently desired for
adults.
Guidelines for Pediatric Red Blood Cell
Transfusions
CHILDREN AND ADOLESCENTS
INFANTS WITHIN THE FIRST 4
MO OF LIFE
Acute loss of >25% at
circulating blood
volume
Hemoglobin of <8.0 g/dL
in the perioperative
period
Hemoglobin of <13.0
g/dL and severe
cardiopulmonary
disease
Hemoglobin of <8.0 g/dL
and symptomatic chronic
anemia
Hemoglobin of <8.0 g/dL
and marrow failure
Hemoglobin of <13.0
g/dL and severe
pulmonary disease
Hemoglobin of <10.0
g/dL and moderate
pulmonary disease
Hemoglobin of <13.0
g/dL and severe cardiac
disease
Hemoglobin of <10.0
g/dL and major surgery
Hemoglobin of <8.0 g/dL
and symptomatic anemia
THE DECISION TO TRANSFUSE
SHOULD NOT BE BASED ON THE
HAEMOGLOBIN LEVEL ALONE, BUT
ALSO ON A CAREFUL ASSESSMENT
OF THE PATIENTS CLINICAL
CONDITION.
PLATELET
CONCENTRATES
PLATELET CONCENTRATES
(prepared from whole blood donations
Description
Unit of issue
Single donor unit in a volume
of 5060 ml of plasma should
contain:
At least 55 x 10
9
platelets
<1.2 x 10
9
red cells
<0.12 x 10
9
leucocytes
May be supplied as either:
Single donor unit: platelets
prepared from one donation
Pooled unit: platelets prepared
from 4 to 6 donor units pooled
into one pack to contain an
adult dose of at least 240 x 10
9
platelets
PLATELET CONCENTRATES
(prepared from whole blood donations
Infection risk
Storage
Same as whole blood, but a
normal adult dose involves
between 4 and 6 donor
exposures
Bacterial contamination affects
about 1% of pooled units
Up to 72 hours at 20C to 24C
(with agitation)
Longer storage increases the
risk of bacterial proliferation
and septicaemia in the
recipient
PLATELET CONCENTRATES
(prepared from whole blood donations
Indications
Treatment of bleeding due
to:
Thrombocytopenia
Platelet function defects
Prevention of bleeding due
to thrombocytopenia, such
as in bone marrow failure
Thrombocytopenia is a risk factor for
hemorrhage, and platelet transfusion
reduces the incidence of bleeding.
The threshold for prophylactic platelet
transfusion is 10,000/L.
In patients without fever or infections, a
threshold of 5000/L may be sufficient to
prevent spontaneous hemorrhage.
For invasive procedures, 50,000/L
platelets is the usual target level.
Guidelines for Pediatric Platelet Transfusions
CHILDREN AND ADOLESCENTS
INFANTS WITHIN THE FIRST 4
MO OF LIFE
PLTs < 50 10
9
/L and
bleeding
PLTs < 50 10
9
/L and an
invasive procedure
PLTs < 20 10
9
/L and
marrow failure with
hemorrhagic risk factors
PLTs < 10 10
9
/L and
marrow failure without
hemorrhagic risk factors
PLTs at any count, but with
PLT dysfunction plus
bleeding or an invasive
procedure
PLTs < 100 10
9
/L and
bleeding
PLTs < 50 10
9
/L and an
invasive procedure
PLTs < 20 10
9
/L and
clinically stable
PLTs < 100 10
9
/L and
clinically unstable
PLTs at any count, but
with PLT dysfunction plus
bleeding or an invasive
procedure
PLATELET CONCENTRATES
(prepared from whole blood donations
Contraindication
s
Not generally indicated for
prophylaxis of bleeding in surgical
patients, unless known to have
significant pre-operative platelet
deficiency
Not indicated in:
Idiopathic autoimmune
thrombocytopenic purpura (ITP)
Thrombotic thrombocytopenic purpura
(TTP)
Untreated disseminated intravascular
coagulation (DIC)
Thrombocytopenia associated with
septicaemia, until treatment has
commenced or in cases of
hypersplenism
PLATELET CONCENTRATES
(prepared from whole blood donations
Dosage 1 unit of platelet concentrate/10
kg body weight: in a 60 or 70
kg adult, 46 single donor
units containing at least 240 x
109 platelets should raise the
platelet count by 2040 x 109/L
Increment will be less if there
is:
Splenomegaly
Disseminated intravascular
coagulation
Septicaemia
TRANSFUSION OF PLATELET CONCENTRATES
Dose units: Platelet concentrate from 1 donor unit (450
ml) of whole blood contains about 60 x 109/L
Dosage Volume Platelet concentrate
Up to 15 kg 1 platelet conc. 3050 ml* 60 x 10
9
/L
1530 kg 2 platelet conc. 60100 ml 120 x 10
9
/L
>30 kg 4 platelet conc. 120400 ml 240 x 10
9
/L
* For small infants, the blood bank may remove part of
the plasma before transfusion
PLATELET CONCENTRATES
(prepared from whole blood donations
Administration
After pooling, platelet
concentrates should be infused as
soon as possible, generally within
4 hours, because of the risk of
bacterial proliferation
Must not be refrigerated before
infusion as this reduces platelet
function
Should be infused over a period of
about 30 minutes
Do not give platelet concentrates
prepared from RhD positive
donors to an RhD negative female
with childbearing potential
PLATELET CONCENTRATES
(prepared from whole blood donations
Complications Febrile non-haemolytic and
allergic urticarial reactions are
not uncommon, especially in
patients receiving multiple
transfusions
The goal of platelet therapy is to
control or stop the bleeding. The
clinical response is more important
than the platelet count.
PLATELET CONCENTRATES
FRESH FROZEN
PLASMA
FRESH FROZEN PLASMA
Description Pack containing the plasma
separated from one whole
blood donation within 6 hours
of collection and then rapidly
frozen to 25C or colder
Contains normal plasma levels
of stable clotting factors,
albumin and immunoglobulin
fibrinogen, Antithrombin,
Proteins C and S.
Factor VIII level at least 70% of
normal fresh plasma level
FRESH FROZEN PLASMA
Unit of issue
Infection risk
Usual volume of pack is
200300 ml
Smaller volume packs may be
available for children
If untreated, same as whole
blood
Very low risk if treated with
methylene blue/ultraviolet light
inactivation
FRESH FROZEN PLASMA
Storage At 25C or colder for up to 1
year
Before use, should be thawed
in the blood bank in water
which is between 30C to
37C.
Higher temperatures will
destroy clotting factors and
proteins
Once thawed, should be stored
in a refrigerator at +2C to
+6C
FRESH FROZEN PLASMA
Indications Replacement of multiple
coagulation factor deficiencies:
Liver disease
Warfarin (anticoagulant)
overdose
Depletion of coagulation factors
in patients receiving large
volume transfusions
Disseminated intravascular
coagulation (DIC)
Thrombotic thrombocytopenic
purpura (TTP)
Guidelines for Pediatric Plasma Transfusions
INFANTS, CHILDREN AND ADOLESCENTS
Severe clotting factor deficiency and
bleeding
Severe clotting factor deficiency and an
invasive procedure
Emergency reversal of warfarin
effects
Dilutional coagulopathy and bleeding
Anticoagulant protein (antithrombin III,
proteins C and S) replacement
Plasma exchange replacement fluid for
thrombotic thrombocytopenic purpura
FRESH FROZEN PLASMA
Precautions Acute allergic reactions are not
uncommon, especially with
rapid infusions
Severe life-threatening
anaphylactic reactions
occasionally occur
Hypovolaemia alone is not an
indication for use
FRESH FROZEN PLASMA
Dosage
Administration
Initial dose of 15 ml/kg
Must normally be ABO
compatible to avoid risk of
haemolysis in recipient
No compatibility testing
required
Infuse using a standard blood
administration set as soon as
possible after thawing
Labile coagulation factors
rapidly degrade; use within 6
hours of thawing
CRYOPRECIPITATE
CRYOPRECIPITATE
Description Prepared from fresh frozen
plasma by collecting the
precipitate formed during
controlled thawing at +4C and
resuspending it in 1020 ml
plasma
Contains about half of the
Factor VIII and fibrinogen in the
donated whole blood: e.g.
Factor VIII: 80100 iu/ pack;
Fibrinogen: 150300 mg/pack
CRYOPRECIPITATE
Infection risk
Storage
As for plasma, but a normal
adult dose involves at least 6
donor exposures
At 25C or colder for up to 1
year
CRYOPRECIPITATE
Indications As an alternative to Factor VIII
concentrate in the treatment of
inherited deficiencies of:
von Willebrand Factor (von
Willebrands disease)
Factor VIII (haemophilia A)
Factor XIII
As a source of fibrinogen in
acquired coagulopathies: e.g.
disseminated intravascular
coagulation (DIC)
CRYOPRECIPITATE
Administration If possible, use ABO-
compatible product
No compatibility testing
required
After thawing, infuse as soon
as possible through a standard
blood administration set
Must be infused within 6 hours
of thawing
CRYOPRECIPITATE-
DEPLETED PLASMA
CRYOPRECIPITATE-DEPLETED
PLASMA
Description Plasma from which
approximately half the
fibrinogen and Factor VIII has
been removed a
cryoprecipitate, butwhich
contains all the other plasma
constituents
Transfusion Reactions
Immediate effects
Hemolytic reactions
Febrile reactions
Allergic reaction
Hyperkalemia
Circulatory overload
Reactions due to
Contaminated bld
Delayed Effects
Hemolytic reaction
Alloimmunization
Infectious complications
Hemosiderosis
Transfusion Reactions
Manifestations of Adverse reaction
Fever with or without chills
most common symptom of Hemolytic
transfusion reaction
Chills with or with out fever
Pain at the transfusion site or in the chest,
abdomen or flanks
Blood pressure changes
Transfusion Reactions
Manifestations of Adverse reaction
Blood pressure changes
Acute
Hypertension
Hypotension
Circulatory shock in combination with fever,
severe chills and high-cardiac-output suggest --
Sepsis or HTR
Guidelines for the recognition acute
transfusion reactions
Signs
Localized Cutaneous
reactions
Urticaria
Rash
Symptoms
Pruritus (itching)
Possible Cause
Hypersensitivity (mild)
Category 1: MILD REACTIONS
Guidelines for the recognition of acute
transfusion reactions
Signs
Flushing
Urticaria
Rigors
Fever
Restlessness
tachycardia
Symptoms
Anxiety
Pruritus
Palpatations
Mild Dyspnea
Headache
Category 2: MODERATELY - SEVERE REACTIONS
Possible Cause
Hypersensitivity
(mod-severe)
Febrile NH
Ab to WBC
Ab to
proteins such
as IgA
Contamination
with pyrogens
and/or bacteria
Guidelines for the recognition of acute
transfusion reactions
Signs
Rigors
Fever
Restlessness
Tachycardia (rise
of >20% in heart
rate
Hypotension
(fall of >20% in
systolic BP)
Haemoglobuniria
(red urine)
Unexplained
bleeding (DIC)
Symptoms
Anxiety
Chest pain
Pain near infusion
site
Respiratory
distress/ shortness
of breath
Loin/ back pain
Dyspnea
Headache
Category 3: LIFE-THREATENING REACTIONS
Possible Cause
Acute intravascular
haemolysis
Bacterial
contamination and
septic shock
Fluid overload
Anaphylaxis
Transfusion
associated acute lung
injury
Hemolytic reactions
Non-immune mediated (physical destruction)
Overheating-use of improvised blood warmers
Forceful transfusion-pressure cuffs
Small bore needles(?)
Using same line for hypotonic solutions or drugs
Bacterial growth in blood units
Hemolytic reactions
Non-immune mediated (physical
destruction)
Treatment
Depends upon the severity of reaction
Severe reaction, hypotension, shock and renal
dysfunction -- Intensive management
Hemoglobinuria or Hemoglobinemia --
Supportive therapy
Hemolytic reactions
Immune mediated
Patient Ab reacting with donor Ag
Wrong blood given
Due to rxn with ABO, Rh, Lewis, Kelly
Severity depends upon the amount
transfused
(as small as 10-15ml)
Hemolytic reactions
Immune mediated
The most dramatic and challenging
adverse event of blood transfusion.
There is rapid destruction of blood cells.
Most commonly occurs
Whole blood
Packed red cell
Hemolytic reactions
Immune mediated
Can also occur in
Fresh frozen plasma
Platelet concentrate
Other plasma derived
Hemolytic reactions
Immune mediated
Acute Hemolytic Transfusion Reaction
Immediately after or with in 24 hours of a
transfusion
Incidence: 1 in 12000 to
1 in 35000 transfusion
Mortality: 1 in 100000 to
1 in 600000 transfusion
Hemolytic reactions
Immune mediated
Delayed Hemolytic Transfusion Reaction
Recognized 3 to 10 days after transfusion
Hemolytic reactions
Immune Mediated
Signs and Symptoms of Acute Immune Mediated
Fever
Chills and rigors
Anxiety
Feeling of dread
Facial flushing
Oliguria
Dyspnea
Diarrhea
Hypotension
Hemoglobinuria
Pallor
Icterus
Hemolytic reactions
Immune Mediated
Signs and Symptoms of Acute Immune Mediated
Back pain
Flank pain
Nausea
Vomiting
Chest pain
Abdominal pain
Anuria
Pain on the
transfusion site
Diffuse bleeding
Jaundice
Hemolytic reactions
Immune Mediated
Signs and Symptoms of Chronic Immune
Mediated
Fever
Chills and rigors
Pallor
Diffuse bleeding
Jaundice
Oliguria
Anuria
Hemolytic reactions
Stop Transfusion
Severity depends on amount (as small
as 30ml)
Maintain adequate systemic arterial
blood
Pressure and tissue perfusion by
hydration
Normal saline solution
Prevent renal failure (100ml/hr urine
output/use of diuretics)
Hemolytic reactions
Vaso-active agents (dopamine)
DIC cryoprecipitate, platelet
Investigate
Blood typing
Coombs test
If positive identify antibody responsible
Urine hemoglobin
Culture of the remaining blood
Febrile Non-Hemolytic
Reaction
Due to anti-leukocyte Antibody against
White cell and platelet of donor
Mild reaction
rule out Hemolytic Transfusion
reaction
bacterial contamination
Febrile Non-Hemolytic
Reaction
43% - 75% of all transfusion reaction
0.5% - 1.4% on non-leukocyte
reduced red blood cell
15% recurrence rate
Febrile Non-Hemolytic
Reaction
Fever
Chills with no reason
Temperature increase of >1C associated
with transfusion and without any other
explanation
Febrile Non-Hemolytic
Reaction
Treatment
Antipyretics/steroids
Antihistamines not indicated -- not involve
histamine release
if frequent -- washed Rbc
Allergic Transfusion Reaction
A rare complication of transfusion of
blood components or plasma
derivatives
Can occur in (most common):
Plasma rich blood component like
Platelet concentrate
FFP/Cryoprecipitate
Can also occur:
Packed red cells
Allergic Transfusion Reaction
The risk is increased by rapid infusion,
typically when fresh frozen plasma is
used as an exchange fluid in therapeutic
plasma exchange.
Cytokines in the plasma may be one
cause of bronchoconstriction and
vasoconstriction in occasional recipients.
Allergic Transfusion Reaction
Allergic transfusion reaction
Due to binding of soluble substance in
donor plasma with IgE antibodies
release of histamine
Allergic Transfusion Reaction
Uncomplicated allergic transfusion
reaction
45% of all transfusion Reaction
Anaphylactoid reaction
1%-3% of transfusion
Anaphylaxis
0.002%-0.005% per transfused product
Allergic Transfusion Reaction
Allergic transfusion reaction
Urticaria (diffuse or local)
Discontinue temporarily but need not be
stopped
Stopped if with other systemic
manifestation such as hypotension, GI
manifestation
Anti histamines
Allergic Transfusion Reaction
Anaphylactoid
reaction
Mild form of:
Fever
Chills
Nausea
Vomiting
Diarrhea
And/or
Urticaria
Anaphylaxis
Severe form (life
threatening
Fever
Chills
Nausea
Vomiting
Diarrhea
And/or Urticaria
Allergic Transfusion Reaction
Anaphylaxis (life threatening)
May include several systems
Respiratory (cough, wheezing, chest
tightness)
GI (vomiting, diarrheas, nausea)
Circulatory (arrhythmias)
Ig A deficiency
Allergic Transfusion Reaction
Treatment
Stop transfusion
Depends upon severity
Hypotension fluids, epinephrine
Bronchospasm B
2
agonist, Theophyline
Post transfusion purpura
Thrombocytopenia 5 to 21 days
Patient makes an alloantibody in
response to platelet antigens in the
transfused blood that for a period of
time (7-48days) causes destruction of
autologous antigen-negative platelets.
Sign/Symptoms: Thrombocytopenia that
is frequently profound, purpura, or
bleeding
Post transfusion purpura
Treatment
Platelet transfusion is of very little value
- should be reserved for patients with
active bleeding.
Therapeutic plasma exchange may be
beneficial.
Transfusion related Acute Lung
Injury
Rare
Mortality: 10%
Abrupt onset of non cardiogenic
pulmonary edema
Rapid failure of pulmonary function
usually presents within 1 to 4 hours of
starting transfusion, with diffuse opacity
on the chest X-ray.
Transfusion related Acute Lung
Injury
Presence of antibodies in the donor
plasma reactive to recipient leukocyte
antigens
Production of inflammatory mediators
during storage of cellular blood
components
Transfusion related Acute Lung
Injury
Symptoms
Respiratory distress
Fever
Chills
Increased respiratory rate
Cough
Tachycardia
Transfusion related Acute Lung
Injury
Most resolve within 72 hours
Treatment
Support (O2, ventilation)
Severe cases may require assisted
ventilation with high FIO2.
Circulatory overload
Fluid overload can result in heart failure and
pulmonary edema.
May occur when:
Too much fluid is transfused
The transfusion is too rapid
Renal function is impaired.
Fluid overload is particularly likely to
happen in patients with:
Chronic severe anaemia
Underlying cardiovascular disease.
Circulatory overload
May complicate up to 1 in 100
transfusion
Symptoms
Dyspnea
Orthopnea
Cough
Tachycardia
Hypertension
Infectious
Bacterial /Viral
Can occur in:
Packed red cells
Plasma rich blood component (most
common)
Platelet concentrate
FFP/Cryoprecipitate
Bacterial Infections
Packed red cells
2.6 per 100000 transfusions
Symptoms
Temperature
higher than 38.5
Rigors
Hypotension
Nausea
Vomiting
Dyspnea
Diarrhea
Shock
Oliguria
DIC
Bacterial Infections
Platelet concentrate (common)
8-80 per 100000 units transfused
(random)
Symptoms
Symptoms may begin during or shortly
after transfusion or begin up to 2 weeks
after transfusion:
Fever, Chills, Hypotension
Viral Infections
Hepatitis
Hepatitis A
Rare
1:1million
Hepatitis B
1:63000
Hepatitis C
Hepatitis D
Viral Infections
Human Herpes Infection
CMV
EBV
Vous aimerez peut-être aussi
- Textbook of Pediatric Hematology and Hemato-OncologyDocument541 pagesTextbook of Pediatric Hematology and Hemato-OncologyAngeline Adrianne83% (6)
- Blood Administration and Transfusion Reactions QuizDocument5 pagesBlood Administration and Transfusion Reactions Quizremooheshmat100% (1)
- BOMBAY Blood GroupDocument14 pagesBOMBAY Blood Groupmail2jackal0% (1)
- Iso 10993Document25 pagesIso 10993Diego Sebastian Rojas GodoyPas encore d'évaluation
- Case Study 5 HemophiliaDocument35 pagesCase Study 5 HemophiliaLorenz Anthonale Pulido100% (1)
- Blood Tranfusion11Document60 pagesBlood Tranfusion11Marites Angeles Bautista100% (2)
- Blood Groups, Blood Components, Blood Transfusion PresentationDocument50 pagesBlood Groups, Blood Components, Blood Transfusion PresentationAashish Gautam100% (1)
- Blood Transfusion and Transfusion ReactionDocument104 pagesBlood Transfusion and Transfusion Reactionrodelagapito-1100% (1)
- Blood TransfusionDocument28 pagesBlood TransfusionPORTRAIT OF A NURSEPas encore d'évaluation
- Blood Transfusion SeminarDocument20 pagesBlood Transfusion SeminarJeezreel100% (1)
- Transfusion of Blood & Blood Components1Document45 pagesTransfusion of Blood & Blood Components1Chamika Huruggamuwa100% (1)
- Anticoagulants and Other PreservativesDocument26 pagesAnticoagulants and Other Preservativessdas317Pas encore d'évaluation
- Donor Screening and Component PreparationDocument91 pagesDonor Screening and Component PreparationDominic BernardoPas encore d'évaluation
- Blood Transfusion 2Document11 pagesBlood Transfusion 2Anusha VerghesePas encore d'évaluation
- Blood Components PDFDocument67 pagesBlood Components PDFAhamed Minver100% (1)
- University of Santo Tomas Immunohematology and Transfusion MedicineDocument7 pagesUniversity of Santo Tomas Immunohematology and Transfusion MedicineWynlor Abarca100% (1)
- TransfusionguidelinesDocument98 pagesTransfusionguidelinesprisma1100% (1)
- Hospital TransfusionDocument64 pagesHospital TransfusionAlbano HallPas encore d'évaluation
- Hema I Chapter 11 - RBC IndicesDocument15 pagesHema I Chapter 11 - RBC IndicesKumneger DeresePas encore d'évaluation
- SOP Blood Administration EngDocument4 pagesSOP Blood Administration EngEmhemed Amer Tabib100% (2)
- Types of Specimen Collection ContainersDocument7 pagesTypes of Specimen Collection ContainersLucas Dei AmengorPas encore d'évaluation
- Adverse Reaction Blood BankDocument10 pagesAdverse Reaction Blood BankyourfamilydoctorPas encore d'évaluation
- Blood Grouping and Crosss MatchingDocument39 pagesBlood Grouping and Crosss MatchingDr. Pawan KumarPas encore d'évaluation
- Blood TransfusionDocument52 pagesBlood TransfusionAnonymous GC8uMx367% (3)
- Blood Transfusion Reaction 3032018Document33 pagesBlood Transfusion Reaction 3032018Kelly YeowPas encore d'évaluation
- Lec 9-10 Blood Groups & TransfusionDocument51 pagesLec 9-10 Blood Groups & TransfusionEmily Peterson100% (1)
- Blood Transfusion GuidelineDocument402 pagesBlood Transfusion GuidelineAdam Razi0% (1)
- Blood Bank and Blood TransfusionDocument11 pagesBlood Bank and Blood TransfusionMostafa Adel Ahmd100% (1)
- Blood Transfusion ClassDocument61 pagesBlood Transfusion ClassshikhaPas encore d'évaluation
- Analysis of UrineDocument5 pagesAnalysis of UrineHaridha ChandranPas encore d'évaluation
- Collection of Blood From DonorsDocument7 pagesCollection of Blood From DonorsBernardoHernandezPas encore d'évaluation
- Abo Blood GroupingDocument95 pagesAbo Blood GroupingSolomon Fallah Foa SandyPas encore d'évaluation
- WHO Handbook of Blood TranfusionDocument344 pagesWHO Handbook of Blood TranfusionWan Zafirah100% (1)
- Blood Bank QuizDocument13 pagesBlood Bank Quizdimalawang.af100% (1)
- Blood Transfusion FinalDocument8 pagesBlood Transfusion FinalejkohPas encore d'évaluation
- Infection Control Standards in Blood TransfusionDocument44 pagesInfection Control Standards in Blood Transfusionyang_torn100% (2)
- Blood TransfusionDocument28 pagesBlood TransfusionChristina DientePas encore d'évaluation
- ABO Blood Group System NotesDocument45 pagesABO Blood Group System NotesAnne Carmel Verano100% (1)
- Pocket Guide On Red Cells 2012Document8 pagesPocket Guide On Red Cells 2012Dave OrlandoPas encore d'évaluation
- FDA Blood Bank & Blood TranfusionDocument44 pagesFDA Blood Bank & Blood TranfusionDrSyedRashidAliPas encore d'évaluation
- Unit 5 Blood TransfusionDocument10 pagesUnit 5 Blood TransfusionMarianne Gonzales-HerreraPas encore d'évaluation
- Tanzania - CBC Lecture-2-17-14Document61 pagesTanzania - CBC Lecture-2-17-14Jonathan Jas100% (1)
- Red Blood Cell CountDocument5 pagesRed Blood Cell CountOmaPas encore d'évaluation
- PlateletpheresisDocument6 pagesPlateletpheresisEmhemed Amer TabibPas encore d'évaluation
- Blood ComponentsDocument44 pagesBlood ComponentsKrisha VittoPas encore d'évaluation
- Blood TransfusionDocument55 pagesBlood Transfusionanand7504100% (2)
- Blood TransfusionDocument18 pagesBlood TransfusionJeeduu frostPas encore d'évaluation
- B Blab 6 Crossmatch SP 05Document14 pagesB Blab 6 Crossmatch SP 05Rutchelle Joyce PugoyPas encore d'évaluation
- Laboratory Test InterpretationDocument73 pagesLaboratory Test Interpretationjosieangel11Pas encore d'évaluation
- Blood and Blood ProductsDocument24 pagesBlood and Blood Productscnecardio100% (3)
- Blood Transfusion ENGLISHDocument40 pagesBlood Transfusion ENGLISHHajrahPalembangan100% (2)
- Chapter 8 Blood DonationDocument55 pagesChapter 8 Blood DonationCHALIE MEQUPas encore d'évaluation
- Blood Bank EbookDocument14 pagesBlood Bank EbookNomer Formeloza BarlisPas encore d'évaluation
- Sop HematocritDocument1 pageSop HematocritStephanie Bautista Alcantara100% (1)
- Blood Grouping and Cross MatchingDocument2 pagesBlood Grouping and Cross MatchinganupreetPas encore d'évaluation
- Crossmatching and Issuing Blood Components PDFDocument20 pagesCrossmatching and Issuing Blood Components PDFdianaPas encore d'évaluation
- Blood Collection TubesDocument1 pageBlood Collection TubesMohammad Atiq100% (1)
- Red Blood Cell Indices: DR KatekDocument10 pagesRed Blood Cell Indices: DR KatekNathan Lupiya100% (1)
- Theory UrinalysisDocument23 pagesTheory UrinalysisAnggi Dyah AristiPas encore d'évaluation
- Blood Groups & Blood BankingDocument36 pagesBlood Groups & Blood BankingGodfrey Pizaroh Mujuzi100% (2)
- Blood Transfusion Reactions: Dr. Madhuvan GuptaDocument42 pagesBlood Transfusion Reactions: Dr. Madhuvan GuptaDr. Madhuvan GuptaPas encore d'évaluation
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsD'EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsPas encore d'évaluation
- Vector ControlDocument19 pagesVector ControlrodelagapitoPas encore d'évaluation
- Medical Parasitology: "TheDocument35 pagesMedical Parasitology: "Therodelagapito100% (1)
- The Photographic PrinciplesDocument32 pagesThe Photographic PrinciplesrodelagapitoPas encore d'évaluation
- Introduction To Human Resource ManagementDocument44 pagesIntroduction To Human Resource ManagementrodelagapitoPas encore d'évaluation
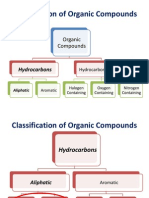
- Introduction To Organic ChemistryDocument48 pagesIntroduction To Organic Chemistryrodelagapito100% (2)
- Principles of EpiDocument29 pagesPrinciples of Epirodelagapito100% (1)
- KolmogorovDocument11 pagesKolmogorovrodelagapitoPas encore d'évaluation
- SkinDocument38 pagesSkinrodelagapito100% (1)
- Principles of Epidemiology & Epidemiologic MethodsDocument8 pagesPrinciples of Epidemiology & Epidemiologic MethodsrodelagapitoPas encore d'évaluation
- Blood ComponentsDocument4 pagesBlood ComponentsVishweshPatel100% (1)
- Anatomy and Physiology Ch18 LectureDocument89 pagesAnatomy and Physiology Ch18 LectureJessica CamillaPas encore d'évaluation
- First Year Complete Physiology MCQ Bank by Team DR Of2027-28Document284 pagesFirst Year Complete Physiology MCQ Bank by Team DR Of2027-28ammejan10100% (1)
- Practical Hematology Manual #1Document48 pagesPractical Hematology Manual #1Michelle P100% (2)
- Hemostasis PDFDocument70 pagesHemostasis PDFOka Iramda SaputraPas encore d'évaluation
- Lab 5 Estimation of Serum GlucoseDocument34 pagesLab 5 Estimation of Serum Glucoseahmed100% (2)
- ISBB CompilationDocument6 pagesISBB CompilationElla SalesPas encore d'évaluation
- Thrombocytopenia Brief DiscussionDocument11 pagesThrombocytopenia Brief Discussionriel100% (3)
- Blood RecreationDocument387 pagesBlood RecreationAlexandr TrotskyPas encore d'évaluation
- Pathology Exam 2Document5 pagesPathology Exam 2moneyy24Pas encore d'évaluation
- Vidas Troponin High Sensitive Ref#415386Document1 pageVidas Troponin High Sensitive Ref#415386Mike GesmundoPas encore d'évaluation
- Plavix (Clopidogrel)Document1 pagePlavix (Clopidogrel)E50% (2)
- Essentials of Anatomy and PhysiologyDocument68 pagesEssentials of Anatomy and PhysiologyhamidiPas encore d'évaluation
- HashbrownDocument22 pagesHashbrownLeomill MendiolaPas encore d'évaluation
- Dr. Agtuca - BT, CT, PT & PTTDocument31 pagesDr. Agtuca - BT, CT, PT & PTTJino BugnaPas encore d'évaluation
- Microsoft Word - The BloodDocument16 pagesMicrosoft Word - The BloodMelanie Fleckner0% (3)
- Toxic Responses of The BloodDocument10 pagesToxic Responses of The BloodM. Joyce100% (2)
- Pathology NotesDocument29 pagesPathology NotesMK100% (1)
- Platelet BiologyDocument14 pagesPlatelet Biologylakshminivas PingaliPas encore d'évaluation
- Arthrex PersonalizedCellTherapyDocument27 pagesArthrex PersonalizedCellTherapyMofit penjačka stijenaPas encore d'évaluation
- Platelet-Rich Plasma For Skin RejuvenationDocument17 pagesPlatelet-Rich Plasma For Skin Rejuvenationleenatalia93Pas encore d'évaluation
- Chapter 19 Blood 2304Document26 pagesChapter 19 Blood 2304Nishchaya SinghPas encore d'évaluation
- Manual Coleta Greiner Bio-OneDocument37 pagesManual Coleta Greiner Bio-OneHelton Resende SilvaPas encore d'évaluation
- Ticagrelor - Changing Paradigm in ACS ManagementDocument42 pagesTicagrelor - Changing Paradigm in ACS ManagementBudi WirawanPas encore d'évaluation
- Organisation Study of Terumo Penpol PVT LTD, ThiruvananthapuramDocument60 pagesOrganisation Study of Terumo Penpol PVT LTD, ThiruvananthapuramishanPas encore d'évaluation
- Animal Venoms in MedicineDocument9 pagesAnimal Venoms in MedicinelimperbiscuitPas encore d'évaluation
- Systemic Response To Injury, Surgical NutritionDocument8 pagesSystemic Response To Injury, Surgical NutritionCarl Earvin L. FavoritoPas encore d'évaluation