Académique Documents
Professionnel Documents
Culture Documents
Urine Formation: Joanna I. Alafag Adv. Animal Physiology Feb. 13, 2020
Transféré par
Tyron Cadiz LopezTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Urine Formation: Joanna I. Alafag Adv. Animal Physiology Feb. 13, 2020
Transféré par
Tyron Cadiz LopezDroits d'auteur :
Formats disponibles
Joanna I.
Alafag
Adv. Animal Physiology
Feb. 13, 2020
HUMAN URINARY SYSTEM
group of organs concerned with filtering out excess
fluid and other substances from the bloodstream
works with the other systems of the body to help
maintain homeostasis.
Parts of the Urinary Sytem
I. KIDNEYS
Functions of the Kidneys
1. Regulation of blood ionic composition.
2. Maintenance of blood osmolarity.
3. Regulation of blood volume.
4. Regulation of blood pressure.
5. Regulation of blood pH
6. Release of hormones
7. Regulation of blood glucose level
8. Excretion of wastes and foreign
substances
Functions of the Kidneys
External Anatomy of the
Kidney:
1. Size length: 4-5 in
width: 2-3 in
thickness: 1 in
mass: 145 -150 g
2. Renal hilus
- deep vertical fissure through which
the ureters, vessels and nerves leave
the kidney
3. Tissue layers
a. Renal capsule
- smooth, transparent, fibrous
membrane
- barrier against trauma and helps
maintain the shape of the kidney
b. Adipose capsule
- fatty tissue
- protects the kidney from trauma and
holds it firmly in place
c. Renal fascia
- thin, dense layer of irregular
connective tissue
-anchors the kidney
Internal Anatomy of the
Kidney
Blood and Nerve Supply of
the Kidneys
Renal vein
Segmental veins
Interlobar veins
Arcuate veins
Interlobar veins
Peritubular capillaries
and / or vasa recta
Efferent arterioles
Glomerular capillaries
Affferent arterioles
Interlobar arteries
Arcuate arteries
Interlobar arteries
Segmental arteries
Renal artery
NEPHRON
functional unit of the kidney
3 basic functions:
filters blood
returns useful substances to the
blood
removes wastes and other
substances
maintain homeostasis of blood
urine is produced
Parts of the Nephron
A. Renal corpuscle
-where plasma is filtered
1. Glomerulus
- a tangled, rounded mass of capillary
network
2. Glomerular (Bowmans) capsule
- double-walled epithelial cup that
surrounds the glomerulus
- 2 layers:
a. visceral layer
*podocytes - modified simple
squamous epithelial cells
b.parietal layer
- simple squamous epithelium and
forms outer wall of capsule
* capsular (Bowmans) space
- space between the 2 layers of the
glomerular capsule
B. Renal tubule
- where filtered fluid passes
Region Description
1. Proximal convoluted
tubule (PCT)
Simple cuboidal epithelial cells with
prominent brush borders of
microvilli
2. Loop of Henle (LOH)
Loop of Henle: descending
limb and thin ascending limb
Simple squamous epithelial cells
Loop of Henle: thick ascending
limb
Simple cuboidal to low columnar
epithelial cells
3. Most distal convoluted tubule
(DCT)
Simple cuboidal epithelial cells
4. Collecting duct (CD)
Final portion of DCT; collecting
duct (CD)
Simple cuboidal epithelium
consisting of principal cells and
intercalated cells in last part of
DCT and collecting duct
2 Types of Nephrons
1. Flow of Fluid through a
Juxtamedullary Nephron
Glomerular (Bowmans)
capsule
Proximal convoluted
tubule
Descending limb of the
loop of Henle
Thin ascending limb of the
loop of Henle
Thick ascending limb of
the loof of Henle
Distal convoluted tubule
(drains into collecting duct)
Glomerular (Bowmans)
capsule
Proximal convoluted
tubule
Descending limb of the
loop of Henle
Ascending limb of the
loop of Henle
Distal convoluted tubule
(drains into collecting
duct)
2. Flow of Fluid through a
Cortical Nephron
URINE FORMATION
I. GLOMERULAR FILTRATION
substances in blood are filtered at the
endothelial-capsular membrane and
the filtrate enters the PCT
Filtration fraction
- fraction of plasma in the afferent
arterioles of the kidneys that becomes:
Glomerular filtrate
- fluid that enters the capsular space
average daily glomerular
filtrate in adults:
99% of the glomerular filtrate returns to
the bloodstream via tubular
reabsorption
1-2L are excreted as urine
female 150L
male 180L
Filtration Membrane or
Endothelial Capsular Membrane
- sandwich like assembly of endothelial
cells of glomerular capillaries and
podocytes
- permits water and small solutes
- prevents most plasma proteins,
blood cells, and platelets
3 Components:
1. glomerular endothelial cells
- large fenestration (70-100nm)
-permits all solutes in blood plasma to
exit glomerular capillaries
-prevents filtration of blood cells and
platelets.
mesangial cells
- contractile cells that help regulate
glomerular filtration
relaxation: maximal surface area
high glomerular filtration
contraction: reduced surface area
low glomerular filtration
2. basal lamina
- acellular material between the
endothelium and the podocytes
- fibrils in a glycoprotein matrix
- prevents filtration of larger plasma
proteins
3. pedicels
- foot-like processes from each
podocyte
filtration slits
- spaces between pedicels
slit membrane
- permits the passage of molecules
having a diameter smaller than 6-7 nm
(water, glucose, urea, and ions)
Why is there larger volume of fluid
filtered in renal corpuscle than in
other capillaries?
1. glomerular capillaries are long and
extensive greater surface area
2. filtration membrane is thin and porous
3. glomerular capillary blood pressure is
high
Net Filtration Pressure (NFP)
- total pressure that promotes filtration
1. Glomerular blood hydrostatic
pressure (GBHP)
- promotes filtration
- forces water and solutes in blood
plasma
- about 55mm Hg
2. Capsular hydrostatic pressure
(CHP)
- opposes filtration
- pressure exerted against the filtration
membrane by fluid present capsular
space and renal tubule
- about 15mm Hg
3. Blood colloid osmotic pressure
(BCOP)
- opposes filtration
- due to proteins such as albumins,
globulins, and fibrinogen in blood
plasma
- about 30 mm Hg
NFP = GBHP CHP - BCOP
= 55 mmHg - 15mmHg - 30mm Hg
= 10mm Hg
pressure that causes a normal amount of
plasma to filter from glomerulus into
capsular space
Glomerular Filtration Rate
(GFR)
- amount of filtrate formed in all renal
corpuscles of both kidney each minute
- average adult GFR
female: 105 ml/min
male: 125 ml/min
Type of Regulation Major Stimulus Mechanism and Site of Action Effect on GFR
Renal Autoregulation
Myogenic mechanism
Increased stretching of smooth
muscle fibers in afferent arteriole
walls due to increased blood
pressure.
Stretched smooth muscles fibers
contract, thereby narrowing the
lumen of the afferent arterioles.
Decrease
Tubuloglomerular
feedback
Rapid delivery of Na
+
and Cl
-
to the
macula densa due to high systemic
blood pressure.
Increased release of a
vasoconstrictor by the
juxtaglomerular apparatus causes
constriction of afferent arterioles.
Decrease
Neural regulation Increase in level of activity of renal
sympathetic nerves releases
norepinephrine.
Constriction of afferent arterioles
through activation of
1
receptors
and increased rennin.
Decrease
Hormonal Regulation
Angiotensin II
Atrial natriuretic
peptide
(ANP)
Decreased blood volume or blood
pressure stimulates production of
angiotensin II.
Stretching of the heart stimulates
secretion of ANP.
Constriction of both afferent and
efferent arterioles.
Relaxation of mesangial cells in
glomerulus increase capillary
surface area available for filtration.
Decrease
Increase
Regulation of Glomerular Filtration Rate (GFR)
Renal Corpuscle
Glomerular filtration rate:
105-125 ml/min of fluid that is isotonic to
blood
Filtered substances: water and all solutes
present in blood (except proteins) including
ions, glucose, amino acids, creatinine, uric
acid
Substance Total Amount in
Plasma
Filtered (Enters
glomerular capsule
per day)
Reabsorbed
(Returned to blood
per day)
Urine (excreted per
day)
Water 3 L 180 L 178-179 L 1-2 L
Proteins 200g 2 g 1.9 g 0.1 g
Na
+
ions 9.7 g 579 g 575 g 4 g
Cl
-
ions 10.7 g 640 g 633.7 g 6.3 g
HCO
3
-
ions 4.6 g 275 g 275 g 0.03 g
Glucose 2.7 g 162 g 162 g 0
Urea 0.9 g 54 g 27 g 27 g
K
+
ions 0.5 g 29.6 g 29.6 g 2 g
Uric acid 0.15 g 8.5 g 7.7 g 0.8 g
Creatinine 0.03 1.6g 0 1.6 g
Substances in plasma and amounts filtered,
reabsorbed and excreted in urine
II. SELECTIVE TUBULAR
REABSORPTION
- selective process that reclaims
materials from tubular fluid and returns
them to the bloodstream
- epithelial cells all along the renal
tubule and duct carry out reabsorption
- PCT cells make the largest
contribution
Reabsorption Routes:
1. Paracellular Reabsorption
- water and solutes move between
tubule cells
- up to 50 % of the reabsorption of
certain ions and the water that
osmotically accompanies them
2. Transcellular Reabsorption
- substance passes through the apical
membrane of a tubule cell, cytosol,
basolateral membrane and into
interstitial fluid
Transport Mechanisms:
1. Primary active Transport
- energy derived from hydrolysis of ATP
is used to pump a substance across a
membrane
- used by the Na
+
pumps
2. Secondary Active Transport
- the energy stored in an ions
electrochemical gradient drives
substance across a membrane
- symporters: membrane proteins that
move 2 or more substances in the
same direction
- antiporters: membrane proteins that
move 2 or more substances in the
opposite direction
- transport maximum (T
m
): maximum
amount of substance that can be
reabsorbed per unit time
3. Osmosis
a. obligatory water reabsorption:
- water reabsorbed together with
solutes in tubular fluid
- occurs in the PCT and descending
limb of Henle due to their permeability
to water
- 90% of reabsorption of water filtered
by the kidneys occurs together with
Na
+
, Cl
-
and glucose
b. facultative water reabsorption
- occurs mainly in collecting ducts and
is regulated by antidiuretic hormone
- 10% of reabsorption of water
III. TUBULAR SECRETION
- removes a substance from the blood
by transferring materials from the
blood and tubule cells into tubular fluid
2 outcomes of tubular secretion:
Secretion of H
+
helps control blood pH
Secretion of other substances helps
eliminate them from the body
Proximal Convoluted Tubule
Reabsorption (into blood) of filtered:
Water 65% (osmosis)
Na
+
65% (Na pumps,
symporters, antiporters)
K
+
65% (diffusion)
Glucose 100 % (symporters, facilitated
diffusion)
Amino acids 100% (symporters, facilitated
diffusion)
Cl
-
50 % (diffusion)
HCO
3
-
80-90% (facilitated diffusion)
Urea 50% (diffusion)
Ca
2+
, Mg
2+
variable (diffusion)
Secretion (into urine) of:
H
+
variable (antiporters)
NH
4
+
variable, increase in acidosis
(antiporters)
Urea variable (diffusion)
Creatinine small amount
At end of PCT, tubular fluid is still isotonic to
blood (300 mOsm/L)
Loop of Henle
Reabsorption (into blood) of:
Water 15% (osmosis in descending
limb)
Na
+
20-30%(symporters in ascending
limb)
K
+
20-30%(symporters in ascending
limb)
Cl
-
35% symporters in ascending
limb)
HCO
3
-
10-20% (facilitated diffusion)
Urea 50% (diffusion)
Ca
2+
, Mg
2+
variable (diffusion)
Secretion (into urine) of:
Urea variable (recycling from CD)
At end of LOH, tubular fluid is hypotonic (100-
150 mOsm/L)
Distal Convoluted Tubule
Reabsorption (into blood) of filtered
Water 10-15% (osmosis)
Na
+
5% (symporters)
Cl
-
5% (symporters)
Ca
2+
variable (stimulated by
parathyroid)
Principal Cells in Late Distal Tubule
and Collecting Duct
Reabsorption (into blood) of filtered
Water 5-9% (insertion of water channels
stimulated by ADH)
Na
+
1-4% (Na pumps)
Cl
-
5% (symporters)
Urea variable (recycling to loop of
Henle)
Secretion (into urine) of:
K
+
variable amount to adjust for
dietary intake (leakage
channels)
Tubular fluid leaving the collecting duct is
diluted when ADH level is low and
concentrated when ADH level is high
Intercalated Cells in Distal Tubule
and Collecting Duct
Reabsorption (into blood) of filtered
HCO
3
-
variable amount, depends on
(new) H
+
secretion (antiporters)
Urea variable (recycling to LOH)
Secretion (into urine) of:
H
+
variable amount to maintain
acid-base homeostasis (H
+
pumps)
Hormone Major Stimuli that Trigger
Release
Mechanism and Site of
Action
Effects
Angiotensin II Low blood volume or low
blood pressure stimulates
renin-induced production of
angiotensin II.
Stimulates activity of Na
+
/
H
+
antiporters in proximal
tubule cells
Increases reabsorption of
Na
+
, other solutes, and
water, which increases
blood volume
Aldosterone Increased angiotensin II
level and increased level of
plasma K
+
promote release
of aldosterone by adrenal
cortex.
Enhances activity and
synthesis of sodium pumps
in basolateral membrane
and Na
+
channels in apical
membrane of principal cells
in collecting duct.
Increases secretion K
+
and
reabsorption of Na
+
, Cl
-
,
and water, which increases
blood volume.
Antidiuretic hormone (ADH)
or vasopressin
Increased osmolarity of
extracellular fluid or
increased angiotensin II
level promote release of
ADH from the posterior
pituitary gland.
Stimulates insertion of
water-channel proteins-
aquaporin-2, into the apical
membranes of principal
cells.
Increases facultative
reabsorption of water,
which decreases
osmolarity of body fluids.
Atrial natriuretic peptide
(ANP)
Stretching of atria of heart
stimulates secretion of
ANP.
Suppresses reabsorption of
Na
+
and water in proximal
tubule and collecting duct;
also inhibits secretion of
aldosetrone and ADH.
Increases excretion of Na
+
in urine (natriuresis);
increases urine output
(diuresis) and thus
decreases blood volume.
Hormonal Regulation of Selective Tubular
Reabsorption and Tubular Secretion
II. URETERS
transport urine from the renal pelvis of kidney
to the urinary bladder
25-30 cm long; thick-walled, narrow tubes that
vary in diameter from 1 mm -10 mm
peristaltic contractions of the muscular walls of
the ureters, hydrostatic pressure and gravity
push urine toward the urinary bladder
3 Coats:
a. Mucosa
- deepest coat
transitional epithelium
- stretches to accommodate variable amount of fluid
mucus
- prevents cells from coming in contact with urine
b. Muscularis
- intermediate coat
-functions for peristalsis
c. Adventitia
- superficial coat;
- anchors the ureters in place
III. URINARY BLADDER
- a hollow , distensible muscular organ
- receives urine ureters and stores urine
until it is excreted through urethra
- average capacity is 700-800ml
3 Coats of Urinary Bladder
a. Mucosa
- mucous membrane
b. Muscularis / Detrusor muscle
- consists of 3 layers of smooth muscle fibers
internal urethral sphincter (involuntary):
external urethral sphincter (voluntary
c. Adventitia
areolar connective tissue
Micturition Reflex
discharge of urine from the urinary bladder
when the volume of urine exceeds 200-400 ml,
pressure within the urinary bladder increases and
stretch receptors in its wall transmit nerve impulses
into the spinal cord
occurs via parasympathetic impulses
contractions of the detrusor muscle and
relaxation of the internal urethral sphincter muscle
IV. URETHRA
- a duct leading from the internal
urethral orifice in the floor of the
urinary bladder to the exterior of the
body that conveys urine in females
and urine and semen in males
Female Urethra
Male Urethra
Vous aimerez peut-être aussi
- Ammonia Tech Manual 2002Document28 pagesAmmonia Tech Manual 2002Talha Bin Zubair0% (1)
- (K) Gastroenteritis and Fluid VolumeDocument1 page(K) Gastroenteritis and Fluid Volumeapi-3769252Pas encore d'évaluation
- Hemodynamics Practice QuestionsDocument2 pagesHemodynamics Practice QuestionsMax HocksteinPas encore d'évaluation
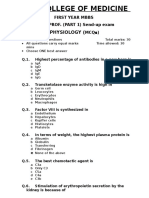
- 1st Year Sendup MCQsDocument8 pages1st Year Sendup MCQsTARIQPas encore d'évaluation
- Anatomy & Physiology QB - Human SystemsDocument1 pageAnatomy & Physiology QB - Human SystemsmanasPas encore d'évaluation
- Questions AnatDocument13 pagesQuestions AnatAfaq RazaPas encore d'évaluation
- Gastrointestinal Anatomy and Physiology: The EssentialsD'EverandGastrointestinal Anatomy and Physiology: The EssentialsJohn F. ReinusPas encore d'évaluation
- Lesson Plan ICFDocument5 pagesLesson Plan ICFTyron Cadiz LopezPas encore d'évaluation
- Kinematics Problem SetDocument1 pageKinematics Problem SetMohammad JubranPas encore d'évaluation
- STC Ratings PDFDocument3 pagesSTC Ratings PDFDiseño SonidoPas encore d'évaluation
- AUBF 02 - (Urine) Chemical PropertiesDocument11 pagesAUBF 02 - (Urine) Chemical PropertiesJustine Alexandrea RamirezPas encore d'évaluation
- Yu - Git - Emb 2Document56 pagesYu - Git - Emb 2gtaha80Pas encore d'évaluation
- Regulation of GIT by gastrointestinal hormonesDocument13 pagesRegulation of GIT by gastrointestinal hormonesRaja Rashid IqbalPas encore d'évaluation
- Prof. Ghabisha Saif Posterior Abdominal Wall AnatomyDocument36 pagesProf. Ghabisha Saif Posterior Abdominal Wall AnatomyAzizPas encore d'évaluation
- Quiz - Development of Human Cardiovascular SystemDocument7 pagesQuiz - Development of Human Cardiovascular Systemlucky mbaselaPas encore d'évaluation
- DPP 2 Oesophagus and StomachDocument4 pagesDPP 2 Oesophagus and StomachDr-Atin Kumar SrivastavaPas encore d'évaluation
- Ganong Physiology 21eDocument1 pageGanong Physiology 21eprasun_v0% (1)
- Endocrine System: Parathyroid, Thyroid, Pancreas, and Adrenal GlandsDocument22 pagesEndocrine System: Parathyroid, Thyroid, Pancreas, and Adrenal GlandsJinnah GandhiPas encore d'évaluation
- Tutorial Lymphatic SystemDocument3 pagesTutorial Lymphatic SystemHazwan100% (1)
- Physiology Final Exams JULY 8, 2020Document17 pagesPhysiology Final Exams JULY 8, 2020Ndor BariboloPas encore d'évaluation
- MCQs On GITDocument3 pagesMCQs On GITsamuel waiswaPas encore d'évaluation
- Endo 3 Notes PDFDocument9 pagesEndo 3 Notes PDFDilPas encore d'évaluation
- Physiology Final Exam - Glory 2017 PDFDocument14 pagesPhysiology Final Exam - Glory 2017 PDFMohammad BarakatPas encore d'évaluation
- Physiology QuestionsDocument14 pagesPhysiology QuestionsLamis Alhaj KaddamPas encore d'évaluation
- GIT & Urinary SystemDocument50 pagesGIT & Urinary SystemRenishya ManiarasuPas encore d'évaluation
- MCI Screening Test 2005Document46 pagesMCI Screening Test 2005Iboyaima SinghPas encore d'évaluation
- MD Physiology CuricullamDocument8 pagesMD Physiology CuricullamPhysiology by Dr RaghuveerPas encore d'évaluation
- Lecture 7 ThermoregulationDocument30 pagesLecture 7 ThermoregulationLouella Artates100% (1)
- Glands of The Digestive SystemDocument16 pagesGlands of The Digestive SystemMatija PajićPas encore d'évaluation
- Practical PhysiologyDocument11 pagesPractical Physiologyapi-3728690Pas encore d'évaluation
- Kidney Function MCQDocument8 pagesKidney Function MCQحسين فاضل حسين طالبPas encore d'évaluation
- TextDocument14 pagesTextOdigo OfujePas encore d'évaluation
- MCQSDocument25 pagesMCQSkays30002403Pas encore d'évaluation
- Physiology questions topic wiseDocument18 pagesPhysiology questions topic wisekoutharapu lasyapriyankaPas encore d'évaluation
- Coordination System Encircle The Best Answer of The Following QuestionsDocument13 pagesCoordination System Encircle The Best Answer of The Following Questionsnon elfPas encore d'évaluation
- 054 Physiology MCQ ACEM Primary RenalDocument1 page054 Physiology MCQ ACEM Primary RenalYasif AbbasPas encore d'évaluation
- Physiology MOCK MCQ Exam September 2012Document33 pagesPhysiology MOCK MCQ Exam September 2012mee youPas encore d'évaluation
- 1 Introduction To The Gastrointestinal SystemDocument7 pages1 Introduction To The Gastrointestinal SystemLinh Phan100% (1)
- 1 4899983447608524847Document113 pages1 4899983447608524847berlianroma100% (1)
- Lab Report Assistant Endocrine SystemDocument7 pagesLab Report Assistant Endocrine SystemJohn Louis AguilaPas encore d'évaluation
- Physiology McqsDocument5 pagesPhysiology McqsFaisal AwanPas encore d'évaluation
- Git Notes in ShortDocument13 pagesGit Notes in ShortNeville212Pas encore d'évaluation
- ABG Exercises 3Document19 pagesABG Exercises 3REMAN ALINGASAPas encore d'évaluation
- Histology of The Digestive SystemDocument27 pagesHistology of The Digestive SystemHarnarayan Jeev Singh Bajaj100% (1)
- Questions Metabolic AcidosisDocument6 pagesQuestions Metabolic Acidosisyayooo2004Pas encore d'évaluation
- BloodDocument38 pagesBloodchukwukerechimezirimPas encore d'évaluation
- MCQs & QUs On Fsirst Year First ComDocument74 pagesMCQs & QUs On Fsirst Year First Commaisara10Pas encore d'évaluation
- BIOLOGY AND HEALTH SCIENCES EXERCISESDocument10 pagesBIOLOGY AND HEALTH SCIENCES EXERCISESAKAYEZU Body santivePas encore d'évaluation
- Mbbs Question BankDocument38 pagesMbbs Question BankHappy MukherjeePas encore d'évaluation
- Disorders of Calcium and Phosphate MetabolismDocument20 pagesDisorders of Calcium and Phosphate MetabolismThirupathi Jakkani100% (1)
- PELVISDocument68 pagesPELVISDevsya DodiaPas encore d'évaluation
- Medical QuestionsDocument13 pagesMedical QuestionsHannah Lei100% (1)
- Digestion and Absorption MCQsDocument3 pagesDigestion and Absorption MCQsSeekerPas encore d'évaluation
- Urinary RenalDocument44 pagesUrinary RenalgorekaPas encore d'évaluation
- Digestive SystemDocument69 pagesDigestive SystemMostafa MontaserPas encore d'évaluation
- MCQ Physio QuestionDocument37 pagesMCQ Physio QuestionKavitha Suresh KumarPas encore d'évaluation
- Chapter 70-GuytonDocument9 pagesChapter 70-Guytonswoljaswol1Pas encore d'évaluation
- 07.lymphatic Sysytem 18Document24 pages07.lymphatic Sysytem 18driraja9999Pas encore d'évaluation
- Important Seqs of Biochemistry For 1st Year Mbbs StudentsDocument7 pagesImportant Seqs of Biochemistry For 1st Year Mbbs Studentsdr saadia anjum0% (1)
- Development of the Digestive System from Foregut to HindgutDocument90 pagesDevelopment of the Digestive System from Foregut to Hindgutyusrah mukhtarPas encore d'évaluation
- Lymphatic Drainage of Abdomen: Learning ObjectivesDocument5 pagesLymphatic Drainage of Abdomen: Learning ObjectivesUloko ChristopherPas encore d'évaluation
- BcqsDocument38 pagesBcqsAdnan MaroofPas encore d'évaluation
- 2 K 23 Mbbs CurriculumDocument300 pages2 K 23 Mbbs CurriculumAbdullah Nayyar100% (1)
- CA BlankDocument4 pagesCA BlankTyron Cadiz LopezPas encore d'évaluation
- SF2 InstructionDocument2 pagesSF2 InstructionTyron Cadiz LopezPas encore d'évaluation
- Name Number Correct Number Incorrect Percentage Tyron C. Lopez 2 2 50Document1 pageName Number Correct Number Incorrect Percentage Tyron C. Lopez 2 2 50Tyron Cadiz LopezPas encore d'évaluation
- ISIP AT KILOS-LOOBDocument7 pagesISIP AT KILOS-LOOBTyron Cadiz LopezPas encore d'évaluation
- CodeDocument1 pageCodeTyron Cadiz LopezPas encore d'évaluation
- SF2 InstructionDocument2 pagesSF2 InstructionTyron Cadiz LopezPas encore d'évaluation
- 15 Team SingleDocument2 pages15 Team SingleTyron Cadiz LopezPas encore d'évaluation
- Test Permit 2018Document9 pagesTest Permit 2018Tyron Cadiz LopezPas encore d'évaluation
- TOS ICF 3rdDocument1 pageTOS ICF 3rdTyron Cadiz LopezPas encore d'évaluation
- SF 2 New UpdatedDocument15 pagesSF 2 New UpdatedTyron Cadiz LopezPas encore d'évaluation
- ICF 4thDocument3 pagesICF 4thTyron Cadiz LopezPas encore d'évaluation
- LP June 15-19Document8 pagesLP June 15-19MichBarundiaOñaPas encore d'évaluation
- FORM 137-A: Grade 7 WISDOMDocument9 pagesFORM 137-A: Grade 7 WISDOMTyron Cadiz LopezPas encore d'évaluation
- FORM 137-A: Grade 7 WISDOMDocument9 pagesFORM 137-A: Grade 7 WISDOMTyron Cadiz LopezPas encore d'évaluation
- Seminar On Energy Efficiency & Conservation Program 102616Document3 pagesSeminar On Energy Efficiency & Conservation Program 102616Tyron Cadiz LopezPas encore d'évaluation
- BRIGADA Appendix E. BE Form 04Document1 pageBRIGADA Appendix E. BE Form 04Tyron Cadiz LopezPas encore d'évaluation
- DO s2015 44 0 PDFDocument134 pagesDO s2015 44 0 PDFRamonPas encore d'évaluation
- BecDocument25 pagesBecTyron Cadiz Lopez100% (1)
- Values Competence P1Document1 pageValues Competence P1Tyron Cadiz LopezPas encore d'évaluation
- Icf - CBC - 1st To 3rd Yr PDFDocument64 pagesIcf - CBC - 1st To 3rd Yr PDFRhea Tupan PradoPas encore d'évaluation
- RESISTANCEDocument9 pagesRESISTANCERohit SahuPas encore d'évaluation
- 19174the Rise of Industrial Big Data WP Gft834Document6 pages19174the Rise of Industrial Big Data WP Gft834em01803257Pas encore d'évaluation
- User ManualDocument14 pagesUser ManualKhaled BellegdyPas encore d'évaluation
- Analytical Chemistry Lecture Exercise 2 Mole-Mole Mass-Mass: Sorsogon State CollegeDocument2 pagesAnalytical Chemistry Lecture Exercise 2 Mole-Mole Mass-Mass: Sorsogon State CollegeJhon dave SurbanoPas encore d'évaluation
- Advanced Technologies of CDQ Plant Advanced Technologies of CDQ PlantDocument12 pagesAdvanced Technologies of CDQ Plant Advanced Technologies of CDQ Plant조기현Pas encore d'évaluation
- Unchained MelodeeDocument93 pagesUnchained MelodeeRafael Cornholio RodriguezPas encore d'évaluation
- M700-70 Series Programming Manual (M-Type) - IB1500072-F (ENG)Document601 pagesM700-70 Series Programming Manual (M-Type) - IB1500072-F (ENG)Mert SertPas encore d'évaluation
- Student Pilot GuideDocument13 pagesStudent Pilot GuideAŞKIN FIRATPas encore d'évaluation
- Conflict and Factional Disputes - Siegel & BealsDocument12 pagesConflict and Factional Disputes - Siegel & BealsDanielPas encore d'évaluation
- Fundamentals of SwimmingDocument7 pagesFundamentals of SwimmingSheila Mae Lira100% (1)
- ArtsDocument5 pagesArtsRhovi Christine AbandoPas encore d'évaluation
- Tenofovir Disoproxil Fumarate: Riefing - Nfrared BsorptionDocument4 pagesTenofovir Disoproxil Fumarate: Riefing - Nfrared BsorptionMostofa RubalPas encore d'évaluation
- Experimental Design and Optimization MethodsDocument38 pagesExperimental Design and Optimization MethodssudalaiyandiPas encore d'évaluation
- Business Plan of Easy Meal ServiceDocument41 pagesBusiness Plan of Easy Meal ServiceCeddie UnggayPas encore d'évaluation
- Meditations on Ancient Astrology Principles from Brihat Parashari HorāDocument87 pagesMeditations on Ancient Astrology Principles from Brihat Parashari HorāPrasanna KumarPas encore d'évaluation
- The Focus Shooting Method CourseDocument48 pagesThe Focus Shooting Method CourseKobiXDPas encore d'évaluation
- RLCraft v2.9 ChangelogDocument28 pagesRLCraft v2.9 ChangelogSơn TrươngPas encore d'évaluation
- Copeland CompressorDocument135 pagesCopeland CompressorsugirinPas encore d'évaluation
- The Ultimate Life GuideDocument12 pagesThe Ultimate Life GuideNLPCoachingPas encore d'évaluation
- Research PaperDocument13 pagesResearch PaperHamid ElmyPas encore d'évaluation
- English Task Resumido 2Document12 pagesEnglish Task Resumido 2Luis ArmandoPas encore d'évaluation
- Poisoning: Selenium in LivestockDocument4 pagesPoisoning: Selenium in Livestockdianarbk otuPas encore d'évaluation
- BR A Consumables Catalog ElecDocument31 pagesBR A Consumables Catalog Elecdweil1552Pas encore d'évaluation
- March 17, 2016 Strathmore TimesDocument24 pagesMarch 17, 2016 Strathmore TimesStrathmore TimesPas encore d'évaluation
- Toaz - Info Chemtech Reviewer PRDocument1 pageToaz - Info Chemtech Reviewer PRchristy janioPas encore d'évaluation
- Schneider Power Supply PhaseoDocument26 pagesSchneider Power Supply PhaseoScott EnnisPas encore d'évaluation
- Chefs at HomeDocument4 pagesChefs at Homezbdv2kyzv7Pas encore d'évaluation