Académique Documents
Professionnel Documents
Culture Documents
Overview of Rheumatoid Arthritis: Naureen Mirza, MD May 10, 2010
Transféré par
csingleton2364Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Overview of Rheumatoid Arthritis: Naureen Mirza, MD May 10, 2010
Transféré par
csingleton2364Droits d'auteur :
Formats disponibles
Overview of Rheumatoid
Arthritis
Naureen Mirza, MD
May 10, 2010
Epidemiology
An annual incidence of approximately 0.2 per
1000 in males and 0.4 per 1000 in females
A prevalence of 0.5-1% is reported in diverse
populations worldwide
Twin studies show the disease to have a
heritability of 60%
Hormonal and reproductive factors contribute to
the female excess and parity
Obesity, smoking, coffee consumption, and prior
blood transfusion have also been identified as
potential risk factors
T
a
b
l
e
6
7
-
1
.
T
H
E
1
9
8
7
A
R
A
C
R
I
T
E
R
I
A
(
T
R
A
D
I
T
I
O
N
A
L
F
O
R
M
A
T
)
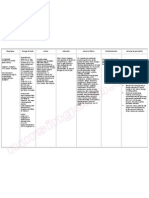
1. Morning stiffness
Morning stiffness in and around the joints, lasting at least 1
h before maximal improvement
2. Arthritis in three or
more joint areas
Soft tissue swelling or fluid (not bony overgrowth) observed
by a physician, present simultaneously for at least 6
weeks
3. Arthritis of hand
joints
Swelling of wrist, MCP or PIP joints for at least 6 weeks
4. Symmetric arthritis Simultaneous involvement of the same joint areas (defined
in 2) on both sides of the body (bilateral involvement of
PIP, MCP or MTP joints is acceptable without absolute
symmetry) for at least 6 weeks
5. Rheumatoid nodules Subcutaneous nodules over bony prominences, extensor
surfaces or in juxta-articular regions, observed by a
physician
6. Rheumatoid factor Detected by a method positive in fewer than 5% of normal
controls
7. Radiographic
changes
Typical of RA on posteroanterior hand and wrist
radiographs; it must include erosions or unequivocal
bony decalcification localized in or most marked
adjacent to the involved joints (OA changes alone do
not qualify)
New criteria for the diagnosis of RA
Joint involvement
1 med-lg joint
0
2-10 Med-Lg joints 1
1-3 small joints 2
4-10 small joints 3
>10 small joints 5
Serology
Neither RF or Anti ccp
0
At least one + with low titer 2
Atleast one with high titer 3
Duration of synovitis
<6 weeks
0
>6 weeks 1
Acute phase reactants
Neither CRP or ESR abnormal
0
Abnormal CRP or abnormal ESR 1
Score >=6 indicates
definite RA
History In RA
Chronological account of illness from the onset
Onset: acute or gradual, with details
Location of pain (local or referred): precise anatomy,
presence/absence of swelling
Pattern of joint involvement: axial, peripheral, symmetric
Type of pain: quality and character
Severity: pain threshold effects, interference with activities of daily
living, range of joint movement
Radiation of pain: local or deep referred type
Clinical course: duration, frequency, periodicity, persistence
Modifying factors: aggravating, relieving, medication effects
Associated symptoms: fatigue, other systemic symptoms
Duration of morning stiffness: non-restorative sleep pattern
Present status: regional review of joints, extra-articular features,
functional class, activities of daily living, psychologic state
C
L
I
N
I
C
A
L
E
V
A
L
U
A
T
I
O
N
O
F
R
H
E
U
M
A
T
O
I
D
A
R
T
H
R
I
T
I
S
-
E
X
A
M
I
N
A
T
I
O
N
Extra-articular features
Record presence of nodules, Raynaud's phenomenon,
digital infarcts, episcleritis, peripheral neuropathy, palmar
erythema, leg ulcers
Note tendon sheath involvement, or tendon nodules,
subluxation or rupture
Check for anemia, splenomegaly, leukopenia, pleuritis or
pericarditis, the sicca syndrome or renal involvement
Articular: measures of inflammatory activity
Check for tenderness, synovial effusion, grip strength
Articular: measures of destruction and deformity
Check for lax collaterals, subluxation, malalignment,
metatarsal prolapse, hammer toes and bone-on-bone
crepitus
Examination
Articular manifestations
Arthritis : Joint swelling, tenderness,
warmth, limitation of motion, pain in range
of motion,
Morning stiffness
Muscle atrophy
Chronic deformities
Ankylosis of the joint
Rheumatoid nodules
20% of RA patients with +tests for blood
rheumatoid factors and rarely in RF
most commonly on pressure areas
central fibrinoid necrosis with surrounding
fibroblasts
May occur in any organs as well
May regress with treatment , but has been
reported to increase with Methotrexate use
believed to occur as a result of small vessel
vasculitis with fibrinoid necrosis, which
forms the center of the nodule, and
surrounding fibroblastic proliferation
Histology of rheumatoid nodule
Rheumatoid nodule with granulomatous
transformation. There is prominent central fibrinoid
necrosis, with surrounding palisading histiocytes and an
outer layer of chronic fibrosing connective tissue with
inflammatory cells including lymphocytes and fibroblasts.
Hematologic abnormalities
Anemia
Thrombocytosis
Thrombocytopenia ( rare )
Eosinophilia(esp related to gold)
Lymphadenopathy ( concomitant Sjogrens syndrome may
increase the risk of Lymphoma)
Splenomegaly ( clinically in 5-10 % with active RA and upto
58% by radionuclide scanning)
Feltys syndrome
RA in combination with splenomegaly and leukopenia
long-standing, seropositive, nodular, deforming RA
33% do not have active synovitis
Lower extremity ulcers, hyperpigmentation, bacterial
infections, ANAs, Also may have thrombocytopenia,
hypocomplementemia,
an increased risk for the development of lymphomas
Neutropenia
Anemia
Thrombocytopenia
Splenomegaly
large granular
lymphocytes in these
patients represent in
vivo activated
cytotoxic T cells and
clonality is present.
Large granular lymphocytes
Pulmonary manifestations
Pulmonary nodules
Pleural effusions (50%)
Caplans syndrome
Diffuse interstitial
pulmonary fibrosis (28%)
Bronchiolitis obliterans
organizing pneumonia
(BOOP)
Obliterative bronchiolitis
Drug induced
Isolated pul. Arteritis (rare)
Pulmonary hypertension
(rare)
Airway obstruction (38%)
Caplans
syndrome
Cardiac disease in RA
Pericarditis (50%)
Premature cardiovascular disease (TNF- is produced by cardiac
myocytes and resident macrophages during cardiac stress and may help trigger and
perpetuate atherosclerosis)
Myocardial and endocardial disease (clinically insignificant)
Coronary arteritis
Valvular abnormalities
Rheumatoid nodule in the aortic valve cusp
Ocular Involvement
Most common : Keratoconjuctivitis sicca (10-35%)
Episcleritis : nodular or diffuse, appears acutely and
causes eye redness and pain
Scleritis is less common than episcleritis, but is more obviously correlated
with vasculitis, long-standing arthritis and active joint inflammation.
Untreated scleritis may progress to scleromalacia
Scleromalacia
Other uncommon manifestation of RA in the
eye
Uveitis
Episcleral nodulosis
Corneal filamentary keratitis
Peripheral ulcerative keratitis
Retinal detachments
Macular edema
Glucocorticoids, Gold and Chloroquine
Brown's syndrome, which is defined as diplopia upon
upward and inward gaze and is believed to be the result of
inflammation and thickening of the superior tendons, and
optic neuritis
Neurological manifestations
Nerve compressions
(Carpal tunnel, tarsal tunnel, atlantoaxial subluxation, subaxial
c-spine involvement, extradural nodules)
Stroke, seizure, hemorrhage, encephalopathy and
meningitis as a result of cerebral vasculitis, amyloidosis or
rheumatoid nodules, or both, in the dura and choroid plexus
of the brain
Most patients have long-standing RA with other extra-
articular disease
Renal Involvement
The kidneys are usually spared in RA, although a low-grade
membranous nephropathy, glomerulitis, vasculitis and secondary
reactive amyloidosis have all been described
Renal abnormalities frequently result from the agents used in
treating RA, notably gold, D-penicillamine, cyclosporin and NSAIDs,
and usually manifest as membranous nephropathy and acute
interstitial nephritis, often the result of a drug hypersensitivity
reaction
Amyloidosis
0.7-5.8% of patients with RA
Virtually every organ system may be involved in the secondary
amyloidosis that complicates RA, including the heart, kidney, liver,
spleen, intestines and skin.
Renal manifestations of amyloidosis are the most common ones
Poor prognosis : 4-year survival rates of about 58% are reported
Rheumatoid vasculitis
Systemic vasculitis uncommon, usually with longstanding,
poorly controlled disease
pANCA
More in patients with feltys
Skin: Nail fold infarcts . Leg ulcers, gangrene
Baker's popliteal cyst
Diagnosis
CBC
RF
Anti ccp
ESR
X rays of affected joints
Musculoskeletal ultrasound
MRI
Additional testing
PPD
Chest X ray
Hep B and C serologies
ANA
Joint aspiration
Synovial biopsy
Lyme serology
Treatment options
NSAIDs
Hydroxychloroquine
Steroids, systemic and intra articular
Methotrexate
Sulfasalazine
Leflunomide
More aggressive disease
TNF inhibitors
Abatacept (CTLA 4 IgG)
Rituximab (Anti CD 20)
Vous aimerez peut-être aussi
- DR - Farhad Salehzadeh Connective Tissue DiseaseDocument70 pagesDR - Farhad Salehzadeh Connective Tissue DiseaseLinux LinuxPas encore d'évaluation
- Final Rheumatoid ArthritisDocument27 pagesFinal Rheumatoid ArthritisAmmarPas encore d'évaluation
- Rheumatology SummaryDocument4 pagesRheumatology SummaryFarah FarahPas encore d'évaluation
- Clinical Manifestations and Diagnosis of Systemic Sclerosis (Document30 pagesClinical Manifestations and Diagnosis of Systemic Sclerosis (Leang KarichakPas encore d'évaluation
- باطنة تمريض rheumatologyDocument6 pagesباطنة تمريض rheumatologyAbdullmlik AlfurasPas encore d'évaluation
- Final Rheumatoid ArthritisDocument58 pagesFinal Rheumatoid ArthritisShivalingaiah GirishPas encore d'évaluation
- Synovial Fluid Analysis: Philip Chui Nathan King Miriam Nojan Ambulatory Presentation Steven Zhao OCTOBER 16, 2015Document31 pagesSynovial Fluid Analysis: Philip Chui Nathan King Miriam Nojan Ambulatory Presentation Steven Zhao OCTOBER 16, 2015Achmad Harun MuchsinPas encore d'évaluation
- Ra Sle MSDocument60 pagesRa Sle MSDionisius KevinPas encore d'évaluation
- Approach Patient With ArthritisDocument45 pagesApproach Patient With ArthritisAli TawbePas encore d'évaluation
- Rheumatoid ArthritisDocument37 pagesRheumatoid ArthritisPetit NacarioPas encore d'évaluation
- Rheumatoid ArthritisDocument6 pagesRheumatoid ArthritisJayson Cruz100% (2)
- Approach To Arthritis PDFDocument54 pagesApproach To Arthritis PDFanahitshoPas encore d'évaluation
- Rheumatology Year 4Document90 pagesRheumatology Year 4Abdalla SamatarPas encore d'évaluation
- Rheumatology: - Syrian - Notes - CK - 2 - Step - Usmle - Pieces/8806 - Bits - CK - 2 - Step - Student - HTMLDocument5 pagesRheumatology: - Syrian - Notes - CK - 2 - Step - Usmle - Pieces/8806 - Bits - CK - 2 - Step - Student - HTMLLoyla RosePas encore d'évaluation
- Avascular Necrosis of Femoral HeadDocument50 pagesAvascular Necrosis of Femoral HeadStar CruisePas encore d'évaluation
- Guideline of GoutDocument28 pagesGuideline of GoutAhmad Fathira Fitra100% (1)
- SBRC RheumatologyDocument26 pagesSBRC RheumatologyErin HillPas encore d'évaluation
- Rheumatoid Athritis (Ra)Document24 pagesRheumatoid Athritis (Ra)Malueth Angui100% (1)
- Rheumatic DiseasesDocument42 pagesRheumatic DiseasesToko RaMy LinePas encore d'évaluation
- AR - Clínica y LaboratorioDocument8 pagesAR - Clínica y LaboratoriomonseibanezbarraganPas encore d'évaluation
- CTD1Document1 pageCTD1David HosamPas encore d'évaluation
- ARTHRITIS-by Ayesigwa GeraldDocument38 pagesARTHRITIS-by Ayesigwa GeraldAyesigwa Gerald96Pas encore d'évaluation
- Rheumatoid ArthritisDocument29 pagesRheumatoid ArthritisTamim IshtiaquePas encore d'évaluation
- ArthritisDocument56 pagesArthritisyulitamustikasariPas encore d'évaluation
- Chap 321: GideonjcaballesDocument73 pagesChap 321: GideonjcaballesMichelle TheresePas encore d'évaluation
- Systemic Lupus ErythematosusDocument3 pagesSystemic Lupus ErythematosusAlya Putri KhairaniPas encore d'évaluation
- Rheumatoid ArthritisDocument32 pagesRheumatoid ArthritisAyyappan JayavelPas encore d'évaluation
- Muskuloskeletal 2Document80 pagesMuskuloskeletal 2feby faradillaPas encore d'évaluation
- Faculty of MedicineDocument28 pagesFaculty of MedicineRana AtefPas encore d'évaluation
- Rheumatoid ArthritisDocument143 pagesRheumatoid ArthritisMuhammad HaneefPas encore d'évaluation
- Rheumatology For AMK: Abhinav Singh PMSDocument43 pagesRheumatology For AMK: Abhinav Singh PMSTerrence ChanPas encore d'évaluation
- Pag 001 190 GeorgescuDocument19 pagesPag 001 190 GeorgescuBooker DewittPas encore d'évaluation
- SLE-combined 2 ArshadDocument71 pagesSLE-combined 2 ArshadarshadsyahaliPas encore d'évaluation
- Arthritides 5th Year-UNZA LectureDocument76 pagesArthritides 5th Year-UNZA LectureMohammed AadeelPas encore d'évaluation
- Acutely Swollen JointDocument7 pagesAcutely Swollen JointHossein VakiliPas encore d'évaluation
- Scleroderma, Sjogren's SyndromeDocument31 pagesScleroderma, Sjogren's SyndromeSalomeSibashviliPas encore d'évaluation
- Systemic Lupus Erythematosus - An Overview: - Dr. Parvez KhanDocument68 pagesSystemic Lupus Erythematosus - An Overview: - Dr. Parvez KhanMohammad Sadiq AzamPas encore d'évaluation
- Share Inflammatory ArthritisDocument122 pagesShare Inflammatory ArthritisDrAnkur BorahPas encore d'évaluation
- Systemic Lupus Erythematosus SLE: DefinitionDocument19 pagesSystemic Lupus Erythematosus SLE: DefinitionShimmering MoonPas encore d'évaluation
- Lupus Nephritis1Document45 pagesLupus Nephritis1Lingga GumelarPas encore d'évaluation
- Systemic Sclerosis (SSCL)Document4 pagesSystemic Sclerosis (SSCL)AtoPas encore d'évaluation
- Nephrotic SyndromeDocument67 pagesNephrotic SyndromeSharaf EskafiPas encore d'évaluation
- Systemic VasculitidesDocument124 pagesSystemic VasculitidesshahikamunaferPas encore d'évaluation
- Systemic Lupus Erythematosus: More Frequently in Women Than Men 3 Times More in African-AmericanDocument8 pagesSystemic Lupus Erythematosus: More Frequently in Women Than Men 3 Times More in African-AmericanReizeeeePas encore d'évaluation
- Musculoskeletal: Autoimmune Inflammatory Metabolic Infectious DisordersDocument51 pagesMusculoskeletal: Autoimmune Inflammatory Metabolic Infectious DisordersSaya MenangPas encore d'évaluation
- Raynaud'S Phenomenon: Dr. Ajay Panwar Japi (May 2010)Document23 pagesRaynaud'S Phenomenon: Dr. Ajay Panwar Japi (May 2010)Ajay PanwarPas encore d'évaluation
- Rheumatoid Arthritis Module IDocument14 pagesRheumatoid Arthritis Module ISamhitha Ayurvedic ChennaiPas encore d'évaluation
- DOMMR Rheumatoid ArthritisDocument62 pagesDOMMR Rheumatoid Arthritisneeraj_bansal_3Pas encore d'évaluation
- Juvenile DermatomyositisDocument22 pagesJuvenile DermatomyositisEmily EresumaPas encore d'évaluation
- Final Rheumatoid Arthritis - PPT 2Document51 pagesFinal Rheumatoid Arthritis - PPT 2Tino kashiriPas encore d'évaluation
- Rheumatology Notes For ReadingDocument8 pagesRheumatology Notes For ReadingMohamed Rikarz Ahamed RikarzPas encore d'évaluation
- Portofolio SHDocument22 pagesPortofolio SHDini Jatiya AnggrainiPas encore d'évaluation
- Polyarteritis NodosaDocument36 pagesPolyarteritis NodosaAbigalePas encore d'évaluation
- Approach To ARTHRITISDocument46 pagesApproach To ARTHRITISkalfPas encore d'évaluation
- Young - 2007Document21 pagesYoung - 2007TurboPas encore d'évaluation
- Sickle Cell and HemophiliaDocument38 pagesSickle Cell and HemophiliacorneliusPas encore d'évaluation
- DR Is - Systemic Lupus ErythematosusDocument27 pagesDR Is - Systemic Lupus ErythematosusRizky SudarmaPas encore d'évaluation
- Bioorganic & Medicinal Chemistry LettersDocument6 pagesBioorganic & Medicinal Chemistry Letterscsingleton2364Pas encore d'évaluation
- Core Structure of gp41 From The HIV Envelope Glycoprotein: 1997 by Cell PressDocument11 pagesCore Structure of gp41 From The HIV Envelope Glycoprotein: 1997 by Cell Presscsingleton2364Pas encore d'évaluation
- Stony Brook University Parking Map: F E D C B ADocument2 pagesStony Brook University Parking Map: F E D C B Acsingleton2364Pas encore d'évaluation
- BRS - Pharmacology 4th Ed PDFDocument382 pagesBRS - Pharmacology 4th Ed PDFcsingleton2364100% (4)
- Doctors in Trailing Step 1Document473 pagesDoctors in Trailing Step 1Aneesha Chopra100% (2)
- Cracked Tooth PresentationDocument36 pagesCracked Tooth Presentationmirfanulhaq100% (1)
- DR Mohd Suhaimi Tajudin Overview TriageDocument39 pagesDR Mohd Suhaimi Tajudin Overview Triageshinichi kudoPas encore d'évaluation
- Analysis of The Socket Bone Wall Dimensions in The Upper Maxilla in Relation To Immediate Implant PlacementDocument6 pagesAnalysis of The Socket Bone Wall Dimensions in The Upper Maxilla in Relation To Immediate Implant PlacementLeonardo PolitoPas encore d'évaluation
- IDDT Clinical GuidelinesDocument2 pagesIDDT Clinical Guidelinesramel5217780Pas encore d'évaluation
- Fulminant Hepatic FailureDocument9 pagesFulminant Hepatic FailurerazerxxxPas encore d'évaluation
- Downtown Orlando Campus MapDocument2 pagesDowntown Orlando Campus MapJDPas encore d'évaluation
- Drug Study 2Document5 pagesDrug Study 2Bani Ann Dela CruzPas encore d'évaluation
- Medical Emergency Teams/Rapid Response Teams: Purpose and BenefitsDocument2 pagesMedical Emergency Teams/Rapid Response Teams: Purpose and BenefitsPsc CilegonPas encore d'évaluation
- Ayele TilahunDocument81 pagesAyele TilahunJanet Magno De OliveiraPas encore d'évaluation
- Coombs TestDocument5 pagesCoombs TestMima Fatimah LuthfiePas encore d'évaluation
- Inno-Lia HCV ScoreDocument14 pagesInno-Lia HCV ScoreMaria CorreiaPas encore d'évaluation
- The Auburn Plainsman 12-3-1998Document32 pagesThe Auburn Plainsman 12-3-1998The Auburn PlainsmanPas encore d'évaluation
- Janumet PM eDocument62 pagesJanumet PM eRaffi DerderianPas encore d'évaluation
- Chapter 19Document16 pagesChapter 19missy23pap100% (1)
- The Coagulation ConsultDocument284 pagesThe Coagulation ConsultArtur X AlcaPas encore d'évaluation
- Oral Manifestations of Connective Tissue Disease (CTDDocument34 pagesOral Manifestations of Connective Tissue Disease (CTDFatin Nabihah Jamil67% (3)
- Children-Mental Health-Facts-NamiDocument1 pageChildren-Mental Health-Facts-Namiapi-298799918Pas encore d'évaluation
- Introduction Sports MassageDocument6 pagesIntroduction Sports MassageHari SetiawanPas encore d'évaluation
- IFIC Basic Concepts of Infection ControlDocument196 pagesIFIC Basic Concepts of Infection ControlYULI22280% (5)
- Baxter International IncDocument133 pagesBaxter International IncTuePas encore d'évaluation
- Neuro Obs - ResidentDocument2 pagesNeuro Obs - ResidentAKNTAI002100% (6)
- Hypertrophic Pyloric StenosisDocument28 pagesHypertrophic Pyloric StenosisAhmad Abu Kush100% (2)
- Patient AssesmentDocument18 pagesPatient AssesmentMarian Ioan-LucianPas encore d'évaluation
- Clonidine HydrochlorideDocument1 pageClonidine HydrochlorideLovelyn Joy Abubo CortezPas encore d'évaluation
- A Short Excerpt From Richard Selzer's "Mortal Lessons"Document3 pagesA Short Excerpt From Richard Selzer's "Mortal Lessons"Ben_Cap_61867% (3)
- Medical CenterDocument38 pagesMedical CenterKhea Micole MayPas encore d'évaluation
- Pediatric PneumoniaDocument12 pagesPediatric PneumoniaKrystal Migo Denolo ContrerasPas encore d'évaluation
- Comprehension Book Grade 12Document66 pagesComprehension Book Grade 12milkovicius0% (3)
- Medical Transcription - Operative ReportDocument2 pagesMedical Transcription - Operative Reportmyahuynh25100% (1)
- Woodcutters TechniqueDocument3 pagesWoodcutters TechniqueToo SmallPas encore d'évaluation