Académique Documents
Professionnel Documents
Culture Documents
Biopsychosocial Model
Transféré par
TonieGeneralDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Biopsychosocial Model
Transféré par
TonieGeneralDroits d'auteur :
Formats disponibles
BIOPSYCHOSOCIAL MODEL
IN MEDICAL PRACTICE
Dr. YASER ALHUTHAIL
Associate Professor & Consultant
Consultation Liaison Psychiatry
Biomedical Model:
The application of biological science to maintain health
and treating disease.
Engel (1977) proposed a major change in our
fundamental model of health care.
The new model continues the emphasis on biological
knowledge, but also encompasses the utilization of
psychosocial knowledge.
Biopsychosocial Model
Implications:
Unity of mind and body:
Psychosocial factors must be taken into account
when considering all disease states
Emphasis on examining and treating the whole
patient, not just his or her disease or disorder.
Most illness, whether physical or psychological, is
influenced and determined by biological,
psychological, and social factors
Biological, psychological, and social variables
influence the predisposition, onset, course, and
outcome of the illness
Physicians who are able to evaluate the relationship of
these variables to their patients illnesses will be able
to develop more effective therapeutic interventions
and to achieve better outcomes
Psychological and Behavioral Predisposition to Physical
Illness
Life style, smoking, alcohol, substance abuse, eating
habits, lack of exercise etc account for about 70% Of
all cases of illness and death in the states
Obesity
Personality factors: Type A !!
Onset of illness
The role of stress
Stress can be described as a circumstance that disturbs,
or is likely to disturb, the normal physiological or
psychological functioning of a person.
The adaptive capacity of the person
THE STRESS MODEL
A psychosomatic framework.
Two major facets of stress response.
Fight or Flight response is mediated by
hypothalamus, the sympathetic nervous system, and
the adrenal medulla.
If chronic, this response can have serious health
consequences.
The hypothalamus, pituitary gland, the adrenal cortex
mediate the second facet.
Neurotransmitter Responses to
Stress
Stressors activate noradrenergic systems in the
brain and cause release of catecholamines from
the autonomic nervous system.
Stressors also activate serotonergic systems in
the brain, as evidenced by increased serotonin
turnover.
Stress also increases dopaminergic
neurotransmission in mesoprefrontal pathways.
Endocrine Responses to Stress
CRF is secreted from the hypothalamus.
CRF acts at the anterior pituitary to trigger release of
ACTH.
ACTH acts at the adrenal cortex to stimulate the
synthesis and release of glucocorticoids.
Promote energy use, increase cardiovascular activity,
and inhibit functions such as growth, reproduction,
and immunity.
Immune Response to Stress
Inhibition of immune functioning by glucocorticoids.
Stress can also cause immune activation through a
variety of pathways including the release of humoral
immune factors (cytokines) such as interleukin-1 (IL-
1) and IL-6.
These cytokines can themselves cause further release of
CRF, which in theory serves to increase glucocorticoid
effects and thereby self-limit the immune activation.
High level of Cortisol results in suppression of
immunity which can cause susceptibility to
infections and possibly also in many types of
cancer.
Changes in the immune system in response to stress
are now very well established.
Course and Outcome of Illness
Direct vs. Indirect effect
Stressful life events
Social support
Their combination: 4 times increased mortality post
MI
Mental disorders: course, mortality, health care
utilization, LOS, ER visits, etc
Psychosocial Interventions
Numerous studies indicate that psychosocial
interventions positively affect health outcomes
Supportive, educational, or psychotherapeutic
interventions
Psychobiological Mechanisms
Too many HOWs ?!!
Theories !!..
Exact mechanisms!!..
Further research...
SUMMARY
Multidimensional Approach
Psychosocial influences are well established
Multifaceted impact
Proper communication
Education and support
Vous aimerez peut-être aussi
- Translate Kaplan Sadock Sinopsis Psikiatri Komprehensif Halaman 721 730 PDF FreeDocument76 pagesTranslate Kaplan Sadock Sinopsis Psikiatri Komprehensif Halaman 721 730 PDF FreeHadi GunaPas encore d'évaluation
- Practical Skills On PalpationDocument6 pagesPractical Skills On PalpationsudersonPas encore d'évaluation
- Pain LectureDocument13 pagesPain LectureDale BuckmanPas encore d'évaluation
- Biopsychosocial FactorsDocument6 pagesBiopsychosocial Factorslovelots1234100% (1)
- WHO Vaccine Manual PDFDocument112 pagesWHO Vaccine Manual PDFRagel CorpsPas encore d'évaluation
- Behavioural ScienceDocument10 pagesBehavioural SciencecindyPas encore d'évaluation
- MED 1.1.1 History Taking and Clinical Decision Making PDFDocument9 pagesMED 1.1.1 History Taking and Clinical Decision Making PDFelleinasPas encore d'évaluation
- Sensation and PerceptionDocument61 pagesSensation and Perceptionan100% (1)
- A Guide To Clinical Case Study and Its PresentationDocument13 pagesA Guide To Clinical Case Study and Its PresentationVince Troy AquinoPas encore d'évaluation
- Vocal Function Exercises For Presbylaryn PDFDocument9 pagesVocal Function Exercises For Presbylaryn PDFAngela Lleuful ToledoPas encore d'évaluation
- Engel's Biopsychosocial ModelDocument5 pagesEngel's Biopsychosocial ModelOmar RoaPas encore d'évaluation
- Antiemetic Medications: Agents, Current Research, and Future DirectionsDocument8 pagesAntiemetic Medications: Agents, Current Research, and Future DirectionsNusieba IbrahimPas encore d'évaluation
- 13 - Antiseizure AgentsDocument145 pages13 - Antiseizure AgentsALJHON OSORIOPas encore d'évaluation
- Diagnosis of Systemic Lupus ErythematosusDocument6 pagesDiagnosis of Systemic Lupus ErythematosusMuhammad Akhram ResmanaPas encore d'évaluation
- FC Derm (SA) Part II Past Papers - 2011 Mar 25-3-2014Document4 pagesFC Derm (SA) Part II Past Papers - 2011 Mar 25-3-2014matentenPas encore d'évaluation
- Pulmonary Rehab - ECarroll PDFDocument26 pagesPulmonary Rehab - ECarroll PDFSulabh ShresthaPas encore d'évaluation
- Depressive Disorders Bipolar Disorder SuicideDocument13 pagesDepressive Disorders Bipolar Disorder Suicidenaji santiagoPas encore d'évaluation
- Opiates TipsDocument39 pagesOpiates TipsroooPas encore d'évaluation
- Adjuvant AnalgesicsDocument44 pagesAdjuvant AnalgesicsZulfan EfendiPas encore d'évaluation
- Online Review Exam ISBBDocument44 pagesOnline Review Exam ISBBRockét PeredoPas encore d'évaluation
- Case 6 Revision - Cognitive Impairment: Central SulcusDocument7 pagesCase 6 Revision - Cognitive Impairment: Central SulcusCharlie WalkerPas encore d'évaluation
- HandBook of Pathology and PathoPhysiology of CardioVascularDocument321 pagesHandBook of Pathology and PathoPhysiology of CardioVascularNurwahidah Moh WahiPas encore d'évaluation
- Immunology Lecturs 27Document27 pagesImmunology Lecturs 27Rolls SaeedPas encore d'évaluation
- Answering Vignette For A GradeDocument11 pagesAnswering Vignette For A Gradevasisth50Pas encore d'évaluation
- Reading Test-02 Part - B - CDocument15 pagesReading Test-02 Part - B - Cbinu mathai100% (1)
- Trauma Counselling - Principles and Practice in South Africa Today by Alida Herbst, Gerda Reitsma (Eds.)Document325 pagesTrauma Counselling - Principles and Practice in South Africa Today by Alida Herbst, Gerda Reitsma (Eds.)safranscollectionPas encore d'évaluation
- Antiseizure Drugs: By: Aim D. QuttenehDocument9 pagesAntiseizure Drugs: By: Aim D. QuttenehrimPas encore d'évaluation
- Antenatal Care: Muhammad Wasil Khan and Ramsha MazharDocument55 pagesAntenatal Care: Muhammad Wasil Khan and Ramsha MazharmarviPas encore d'évaluation
- Understanding The Biopsychosocial ApproachDocument8 pagesUnderstanding The Biopsychosocial ApproachTennidoxPas encore d'évaluation
- 04 Consultation ModelsDocument33 pages04 Consultation ModelsFemale calmPas encore d'évaluation
- Stopp StartDocument11 pagesStopp StartHUONGPas encore d'évaluation
- Compendium Medicine Pocket Radiology PreviewDocument13 pagesCompendium Medicine Pocket Radiology Previewmoeimansari7Pas encore d'évaluation
- The Biopsychosocial Model of Health and Illness: Dr. Shaheen E LakhanDocument2 pagesThe Biopsychosocial Model of Health and Illness: Dr. Shaheen E LakhancycohexanePas encore d'évaluation
- Treatment of Comorbid Conduct Turgay AlmagorDocument14 pagesTreatment of Comorbid Conduct Turgay AlmagormailmanatPas encore d'évaluation
- Lecture 10 - Micro Level Factors - Health and Social Care 2017 Student (Autosaved)Document22 pagesLecture 10 - Micro Level Factors - Health and Social Care 2017 Student (Autosaved)ChéSterrPas encore d'évaluation
- Kaneko (2015) Multidimensional Analysis On The Effect of VFE On Aged Vocal Fold AtrophyDocument7 pagesKaneko (2015) Multidimensional Analysis On The Effect of VFE On Aged Vocal Fold AtrophyRoberto Martinez SandovalPas encore d'évaluation
- De PrescribingDocument14 pagesDe PrescribingVazco Castilla LozanoPas encore d'évaluation
- Pain PowerpointDocument50 pagesPain PowerpointRicardo Pascual100% (1)
- Management of Medically Compromised PatientsDocument10 pagesManagement of Medically Compromised PatientsAlfika Dinar FitriPas encore d'évaluation
- Antimicrobials and Non-Healing WoundsDocument92 pagesAntimicrobials and Non-Healing WoundsNelu CastravetPas encore d'évaluation
- Frailty in Older Adults - Evidence For A Phenotype (Fried 2001)Document12 pagesFrailty in Older Adults - Evidence For A Phenotype (Fried 2001)Cristian100% (1)
- NHS England Drugs List v15 2020 2021 PDFDocument12 pagesNHS England Drugs List v15 2020 2021 PDFSandra NgPas encore d'évaluation
- Nciph ERIC10Document5 pagesNciph ERIC10bejarhasanPas encore d'évaluation
- Educating The Chinese Individual: Life in A Rural Boarding SchoolDocument44 pagesEducating The Chinese Individual: Life in A Rural Boarding SchoolUniversity of Washington PressPas encore d'évaluation
- Biopsychosocial Model of Health and DiseaseDocument7 pagesBiopsychosocial Model of Health and DiseaseMary Romaine Dela PasionPas encore d'évaluation
- Formulating The Clinical QuestionDocument25 pagesFormulating The Clinical QuestionlexyuPas encore d'évaluation
- Report On THE CONCEPT OF THERAPEUTIC EMPLOTMENT' 1Document33 pagesReport On THE CONCEPT OF THERAPEUTIC EMPLOTMENT' 1Jeorge M. Dela Cruz100% (1)
- Adult Emergency PDFDocument2 pagesAdult Emergency PDFVon HippoPas encore d'évaluation
- Acute Respiratory Failure 1Document7 pagesAcute Respiratory Failure 1Trish 0019Pas encore d'évaluation
- SC10 Thomas LisaDocument113 pagesSC10 Thomas LisaAldo Hip Naranjo100% (1)
- Altered Mental StatusDocument151 pagesAltered Mental StatusbrentupdegraffPas encore d'évaluation
- Acute Pain: Mechanisms, Management, and Treatment OptionsDocument61 pagesAcute Pain: Mechanisms, Management, and Treatment OptionsAnnisa RamadhanyPas encore d'évaluation
- Histology Self Quiz Intro and EpitheliumDocument3 pagesHistology Self Quiz Intro and EpitheliumJoonHong An100% (1)
- Facial Nerve Palsy: Dr. Saud AlromaihDocument74 pagesFacial Nerve Palsy: Dr. Saud AlromaihChandra ManapaPas encore d'évaluation
- Neurological ExaminationDocument71 pagesNeurological ExaminationSiti Nursuhada binti Mohd AminPas encore d'évaluation
- Critical Appraisal: Noor Pramono NoerpramanaDocument102 pagesCritical Appraisal: Noor Pramono Noerpramanasharma tobingPas encore d'évaluation
- Psych Questions 1Document34 pagesPsych Questions 1MADHUMITHA VEMULA100% (1)
- New Techniques in Physical TherapyDocument61 pagesNew Techniques in Physical TherapyMohamed Magdy El MeligiePas encore d'évaluation
- Traumatic Stress - Effects On The Brain PDFDocument17 pagesTraumatic Stress - Effects On The Brain PDFDaniel Londoño GuzmánPas encore d'évaluation
- The Biopsychosocial Model ... 2017Document10 pagesThe Biopsychosocial Model ... 2017Camila AlmeidaPas encore d'évaluation
- Amyotrophic Lateral SclerosisDocument24 pagesAmyotrophic Lateral SclerosisJeanessa Delantar QuilisadioPas encore d'évaluation
- Health Questionnaire CandidateDocument5 pagesHealth Questionnaire CandidateSaudia Arabia JobsPas encore d'évaluation
- Immunology in the Twentieth Century: From Basic Science to Clinical ApplicationD'EverandImmunology in the Twentieth Century: From Basic Science to Clinical ApplicationPas encore d'évaluation
- Faecal Incontinence in Adults - ReviewDocument12 pagesFaecal Incontinence in Adults - Reviewi can always make u smile :DPas encore d'évaluation
- Centrally-Acting Muscle RelaxantsDocument11 pagesCentrally-Acting Muscle RelaxantsMerBoughPas encore d'évaluation
- Hypernatremia PediatricsDocument7 pagesHypernatremia PediatricsJOHANNESKIFENDIPas encore d'évaluation
- IMA Monthly Report Form JulyDocument4 pagesIMA Monthly Report Form JulyInternetStudioPas encore d'évaluation
- 1-Diabetes Package - PO2693771771-269Document6 pages1-Diabetes Package - PO2693771771-269KishorePas encore d'évaluation
- Consent To Surgery/Anaesthesia: Ilocos Sur Provincial Hospital-Gabriela SilangDocument1 pageConsent To Surgery/Anaesthesia: Ilocos Sur Provincial Hospital-Gabriela SilangRyrey Abraham PacamanaPas encore d'évaluation
- I. Nursing Process A. Assessment 1. Personal Data A. Demographic DataDocument6 pagesI. Nursing Process A. Assessment 1. Personal Data A. Demographic DataNicole Anne TungolPas encore d'évaluation
- Droplet InfectionsDocument11 pagesDroplet InfectionsdevPas encore d'évaluation
- Graves Disease in ChildrenDocument7 pagesGraves Disease in ChildrengarethPas encore d'évaluation
- Health and Family Welfare (C) Department: PreambleDocument14 pagesHealth and Family Welfare (C) Department: PreambleAjish BenjaminPas encore d'évaluation
- 32 PDFDocument22 pages32 PDFniallvvPas encore d'évaluation
- Hon 2005Document5 pagesHon 2005lenirizkiPas encore d'évaluation
- Twin Block 3Document2 pagesTwin Block 3GisselaMaldonadoPas encore d'évaluation
- Patent Ductus ArteriosusDocument31 pagesPatent Ductus ArteriosussuderiPas encore d'évaluation
- Komunikasi Asuhan Pasien - KARS - 2019Document93 pagesKomunikasi Asuhan Pasien - KARS - 2019Yudi Tubagja SiregarPas encore d'évaluation
- Heroine Source: by Waqas, Email 21waqas@stu - Edu.cnDocument14 pagesHeroine Source: by Waqas, Email 21waqas@stu - Edu.cnwaqasPas encore d'évaluation
- Seminar - Discussion 1Document3 pagesSeminar - Discussion 1api-373572658Pas encore d'évaluation
- Rajasekhar2021 Article TheUsefulnessOfGenelynEmbalminDocument4 pagesRajasekhar2021 Article TheUsefulnessOfGenelynEmbalminyordin deontaPas encore d'évaluation
- Closing The Cancer Divide: A Blueprint For ActionDocument45 pagesClosing The Cancer Divide: A Blueprint For ActionPresentaciones_FKPas encore d'évaluation
- Nonoperative Management of Femoroacetabular ImpingementDocument8 pagesNonoperative Management of Femoroacetabular ImpingementRodrigo SantosPas encore d'évaluation
- Neonatal HypotoniaDocument7 pagesNeonatal HypotoniaShirley KoehPas encore d'évaluation
- Adverse Drug ReactionDocument15 pagesAdverse Drug ReactionPuji Arifianti RamadhanyPas encore d'évaluation
- Revitears Study 2Document16 pagesRevitears Study 2office.hospimedPas encore d'évaluation
- Modul Bahasa Inggris Kep-D3 Sem 4Document32 pagesModul Bahasa Inggris Kep-D3 Sem 4Mufarroha98Pas encore d'évaluation
- MCN 1Document5 pagesMCN 1Aijem RyanPas encore d'évaluation
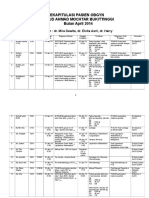
- Rekapitulasi Pasien Obgyn Apr 2014 2Document20 pagesRekapitulasi Pasien Obgyn Apr 2014 2Ressy Dara AmeliaPas encore d'évaluation
- Ectopic Pregnancy (m104)Document13 pagesEctopic Pregnancy (m104)Alphine DalgoPas encore d'évaluation