Académique Documents
Professionnel Documents
Culture Documents
IC1 - Arrhythmia - 2012 EDITED
Transféré par
razorazDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
IC1 - Arrhythmia - 2012 EDITED
Transféré par
razorazDroits d'auteur :
Formats disponibles
Arrhythmias
Richard G Sheahan,
Consultant
Cardiologist/Electrophysiologist
Paroxysmal
Ectopic focus, sudden onset, abrupt cessation
Sustained
Duration of > 30 seconds
Requires intervention to terminate
Non-Sustained
At least 3 beats or < 30 seconds
Spontaneously terminates
Recurrent
Occurs periodically
Periods of no tachycardia are longer than periods
of tachycardia
Terms Describing Tachycardias
Tachyarrhythmias
Supraventricular Tachycardia
Atrial Flutter
Atrial Fibrillation
Ventricular Tachycardia
Ventricular Fibrillation
Sudden Cardiac Death
Premature Atrial & Ventricular
Complexes
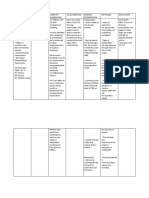
2% VF
Data source: Baily D. J Am Coll Cardiol. 1992;19(3):41A.
34%
Atrial
Fibrillation
18%
Unspecified
6%
PSVT
6%
PVCs
4%
Atrial
Flutter
9%
SSS
8%
Conduction
Disease
3% SCD
10% VT
Arrhythmia Symptoms
Palpitations Sudden Onset or Offset
Shortness of Breath
Chest pain
Syncope or Presyncope/Dizziness
Increasing Fatigue
Cough & Sputum
Impaired Quality of Life
Arrhythmia Signs
Pulse Rate
Blood Pressure
O2 Saturation
Perfusion, Pale Sweaty & Clammy
Heart Failure
Tachycardia Recognition
Rate > 100 bpm
Regular or Irregular
Narrow complex or Broad complex
P waves present or absent
Clinical Assessment
Past History
Arrhythmia
Supraventricular Tachycardia
Atrial Flutter
Atrial Fibrillation
Ventricular Tachycardia
Ventricular Fibrillation
Sudden Cardiac Death
Premature Atrial & Ventricular Complexes
Origin: AV Node
Mechanism: Reentry
Rate: 150 - 230 BPM, faster in teenagers
Characteristics: Normal QRS with absent P-waves;
most common SVT in adults
SVT
Supraventricular Tachycardia
IV Adenosine
Rate Control
Beta blockers, Calcium Channel Blockers
(Digoxin)
Rhythm Control
Normal Ventricule:
Propafenone, Flecainide, sotalol
Abnormal Ventricule
Amiodarone
Synchronized Cardioversion
Hemodynamically unstable
EP Study & RF Ablation
AVNRT( atrioventricular nodal re-entrant tachycardia)
Accounts for 80-90% of SVT
Abrupt onset and offset
The typical ventricular
rate is 140-300/min
P is usually buried within
the QRS complex
Best identified in V1
SVT-AVNRT
P
Just learn to recognise SVT, no need to know
AVRT or AVNRT specifically
AVRT( atrioventricular re-entrant tachycardia)
Reentrant circuit
consists of an
atrioventricular
nodal pathway and
accessory pathway
SVT-AVRT
Sinus Tachycardia
Pain
Anxiety
Fever
Anaemia
Dehydration
Hyperthyroidism
Sinus Tachycardia Treatment
Treat the cause
Acute management:
Treatment aimed at restoration of sinus
rhythm
1. Carotid sinus massage
2. IV adenosine
3. IV verapamil
Sinus Tachycardia Treatment
Long term management:
1. Drug therpy
- directed at AVN
- beta-blocker
- calcium channel blocker
- digoxin
- directed at AP
- Class IA/C agents
2. Radiofrequency ablation
3. Treat the underlying causes (if any)
Arrhythmia
Supraventricular Tachycardia (SVT)
Atrial Flutter
Atrial Fibrillation
Ventricular Tachycardia
Ventricular Fibrillation
Atrial Flutter
Atrial Flutter Treatment
Anticoagulation for High Risk Patients
Rate Control
Beta-blocker, Ca Channel Blocker, (?Digoxin)
Rhythm Control
Cardioversion
Antiarrhythmics
Radiofrequency Ablation
Arrhythmia
Supraventricular Tachycardia (SVT)
Atrial Flutter
Atrial Fibrillation
Ventricular Tachycardia
Ventricular Fibrillation
Atrial Fibrillation
MOST IMPORTANT RHYTHM AND COMMONEST
Feinberg WM, Blackshear JL, Laupacis A, et al. Arch Intern Med. 1995;155:469-473
Atrial Fibrillation
Feinberg WM, Blackshear JL, Laupacis A. Arch Intern Med. 1995;155:469-473
Atrial Fibrillation Demographics by
Age
Atrial Fibrillation Treatment 1
Stroke Prevention
Heparin, Warfarin or newer anticoagulants
ASA
Rate Control
Betablockers, Ca Channel blockers, (? Digoxin)
Rhythm Control
Normal Heart: Propafenone, Flecainide, Sotalol
CHF/LVH/CAD: Amiodarone
Atrial Fibrillation Treatment 2
CORE MATERIAL
Synchronized Cardioversion
< 48 hours Heparin + Cardioversion
> 48 hours Heparin + TOE +/-
Cardioversion
Or Warfarin INR 2.0 -3.0 for > 4 weeks
Pulmonary Vein Isolation Ablation
Atrial Fibrillation Treatment 3
Associated Conditions
Treat Hyperthyroidism before
cardioversion
Treat sepsis
Treat pulmonary embolism
Pacemaker for Bradycardia
CHADS
2
Score*
Congestive heart failure 1
History of hypertension 1
Age > 75 1
Diabetes 1
Stroke / TIA 2
Warfarin indicated when CHADS
2
score > 2
* The CHADS
2
scores were developed in a study published in The Journal of the
American Medical Association in 2001
Annual Stroke Risk
Recommendations for Anticoagulation
Atrial Flutter vs. Atrial Fibrillation
CORE
Atrial Flutter
Summary of Disease Characteristics
Underlying
Mechanism
Pattern
Atrial Rate
Ventricular Rate
Rhythm
Atrial Fibrillation
Multiple wavelet reentry
Multiple/single focus
firing
Wavy baseline
400 BPM
Varies w/conduction
Grossly Irregular
Reentry via macro
reentrant circuit
Saw tooth baseline
250 to 320 BPM
Varies w/conduction
Usually regular
Arrhythmia
Supraventricular Tachycardia (SVT)
Atrial Flutter
Atrial Fibrillation
Ventricular Tachycardia
Ventricular Fibrillation
Origin: Ventricles (Single Focus)
Mechanism: Reentry Initiated by abnormal
Automaticity or Triggered activity
Characteristics: Rapid, wide, and regular QRS
ECG Characteristics
Monomorphic VT
*
Animation
Origin: Ventricles (Wandering Single Focus)
Mechanism: Reentry with movement in the circuit
Initiated by Abnormal Automaticity or
Triggered activity
Characteristics: Wide and irregular QRS Complex that
changes in axis QTc Normal
Polymorphic VT
*
Animation
Origin: Ventricle
Mechanism: Reentry (movement in focus)
Rate: 200 250 BPM
Characteristics: Associated with Long QT interval;
QRS changes axis & morphology
with alternating positive/negative
complexes
Torsades de Pointes
Ventricular Tachycardia
CORE
Ventricular Tachycardia Treatment
Acute
Synchronized Cardioversion if unstable
+/- CPR
IV Amiodarone, Beta-blocker, Magnesium
Chronic
Correct Reversible Causes
ICD if no 1) Reversible Causes or 2) EF <
35%
Arrhythmia
Supraventricular Tachycardia (SVT)
Atrial Flutter
Atrial Fibrillation
Ventricular Tachycardia
Ventricular Fibrillation
Ventricular Fibrillation
CORE
Ventricular Fibrillation Treatment
Acute
Defibrillation
CPR & ACLS
IV Amiodarone, Beta-blocker, Magnesium
Chronic
Correct Reversible Causes
ICD if 1) no Reversible Causes 2) EF < 35%
Vous aimerez peut-être aussi
- Arrhythmia NewDocument73 pagesArrhythmia Newlohith saiPas encore d'évaluation
- 2 - PPT DR Erika Maharani SPJPDocument42 pages2 - PPT DR Erika Maharani SPJPAmry YusufPas encore d'évaluation
- Arrhythmia, Pericardial and Myocardial Diseases (Dr Praveen) 2Document44 pagesArrhythmia, Pericardial and Myocardial Diseases (Dr Praveen) 2hashini1997nisansalaPas encore d'évaluation
- Chapter - 036 Arrhythmias ClassDocument129 pagesChapter - 036 Arrhythmias ClassWisdomIsMiseryPas encore d'évaluation
- ARITMIADocument47 pagesARITMIASarah JR Nur AzizahPas encore d'évaluation
- Primary Care Arrhythmia FinalDocument36 pagesPrimary Care Arrhythmia FinalIsmai Eko SaputraPas encore d'évaluation
- ADVANCED ECG INTERPRETATIONDocument90 pagesADVANCED ECG INTERPRETATIONnursewinstonPas encore d'évaluation
- CARDIOVASCULAR EMERGENCIES GUIDEDocument47 pagesCARDIOVASCULAR EMERGENCIES GUIDEmedstudy123Pas encore d'évaluation
- Pathophysiology of ArrhythmiasDocument15 pagesPathophysiology of ArrhythmiasJonathan MontecilloPas encore d'évaluation
- 5 ArrhythmiaDocument44 pages5 ArrhythmiaDanny DesuPas encore d'évaluation
- Introduction Lecture On Arrhythmias: Putra AntaraDocument34 pagesIntroduction Lecture On Arrhythmias: Putra AntaraDesak PratiwiPas encore d'évaluation
- Supraventricular Arrhythmias: Dr. Arun Srinivas Chief Cardiologist Vikram Hospital, MysoreDocument81 pagesSupraventricular Arrhythmias: Dr. Arun Srinivas Chief Cardiologist Vikram Hospital, Mysorerobinjohn06Pas encore d'évaluation
- Peri Operative Arryhthmias: Dr. Juzny Alkatiri, SPPD, SPJPDocument102 pagesPeri Operative Arryhthmias: Dr. Juzny Alkatiri, SPPD, SPJPAstari Pratiwi NuhrintamaPas encore d'évaluation
- Managing Palpitations and Detecting ArrhythmiasDocument43 pagesManaging Palpitations and Detecting ArrhythmiasChris Jardine LiPas encore d'évaluation
- Heartbeat Disorders: by Aisha Sara Tasnim Physician: Dr. SsebulibaDocument31 pagesHeartbeat Disorders: by Aisha Sara Tasnim Physician: Dr. SsebulibaNinaPas encore d'évaluation
- Ventricular Arrhythmias EP Overview MedtronicDocument44 pagesVentricular Arrhythmias EP Overview Medtronicinu_upPas encore d'évaluation
- Drugs used to treat cardiac arrhythmiasDocument74 pagesDrugs used to treat cardiac arrhythmiasGunel Sadiqova100% (1)
- ECG AbnormalDocument60 pagesECG Abnormalvidishmalaviya300Pas encore d'évaluation
- Arrhythmias: Sing Khien Tiong Gpst1Document34 pagesArrhythmias: Sing Khien Tiong Gpst1preethi preethaPas encore d'évaluation
- Cardiac Emergencies Cne DelhiDocument109 pagesCardiac Emergencies Cne DelhiManisha Thakur100% (1)
- Aritmia LetalDocument49 pagesAritmia LetalfebriyakPas encore d'évaluation
- 12 CS Supraventricular TachycardiaDocument64 pages12 CS Supraventricular TachycardiaFatima MaazPas encore d'évaluation
- ARRHYTHMIASDocument56 pagesARRHYTHMIASMasunga DwasiPas encore d'évaluation
- Supraventricular Tachycardia NotesDocument59 pagesSupraventricular Tachycardia NotesShadi TabbarahPas encore d'évaluation
- Cardiac DisordersDocument15 pagesCardiac Disordersgold_enriquez100% (3)
- Presentation of Cardiac Arrhythmias (BSC Course) - Matt Wright - 2007123 - 0254Document64 pagesPresentation of Cardiac Arrhythmias (BSC Course) - Matt Wright - 2007123 - 0254preethi preethaPas encore d'évaluation
- Supraventricular Tachycardia Causes, Symptoms and TreatmentDocument39 pagesSupraventricular Tachycardia Causes, Symptoms and TreatmentReinsy NoviPas encore d'évaluation
- SVT PresentationDocument39 pagesSVT PresentationReinsy NoviPas encore d'évaluation
- Management of Perioperative ArrhythmiasDocument51 pagesManagement of Perioperative ArrhythmiasAbhishek LonikarPas encore d'évaluation
- Management of Cardiac Arrhythmias in Advanced Cardiac Life Support (ACLSDocument34 pagesManagement of Cardiac Arrhythmias in Advanced Cardiac Life Support (ACLSrhezzaagxxPas encore d'évaluation
- Arrhythmia A ADocument42 pagesArrhythmia A AMohd Faizal KasnanPas encore d'évaluation
- Cardiac Rhythm and Related Disorders: Marshell Tendean, MD Department of Internal Medicine UKRIDA JakartaDocument39 pagesCardiac Rhythm and Related Disorders: Marshell Tendean, MD Department of Internal Medicine UKRIDA JakartaFatimah Hartina FaradillahPas encore d'évaluation
- Ecg Pathology 02Document95 pagesEcg Pathology 02Andi MP Manurung100% (1)
- ACLS Appendix 3Document32 pagesACLS Appendix 3tostc100% (1)
- ArrhythmiasDocument47 pagesArrhythmiasJaismi AntonyPas encore d'évaluation
- SVT PresentationDocument39 pagesSVT PresentationReinsy NoviPas encore d'évaluation
- Supraventricular Tachycardia: Teresa Menendez Hood, MD FACCDocument39 pagesSupraventricular Tachycardia: Teresa Menendez Hood, MD FACCReinsy NoviPas encore d'évaluation
- LA Cardiac Arythmia - 0Document61 pagesLA Cardiac Arythmia - 0Karthik SPas encore d'évaluation
- Kuliah EKG Blok Kegawatdaruratan September 2018Document122 pagesKuliah EKG Blok Kegawatdaruratan September 2018khanzaisdiharanaPas encore d'évaluation
- Workshop Pit IV THN 2017Document57 pagesWorkshop Pit IV THN 2017anettepardedePas encore d'évaluation
- Approach To PalpitationsDocument74 pagesApproach To PalpitationsDarawan MirzaPas encore d'évaluation
- Ventricular Arrhythmia - Hatem AlsrourDocument31 pagesVentricular Arrhythmia - Hatem Alsrourhatem alsrour100% (3)
- Cardiac Arrythmias in The ED Menbeu Edited From AnaDocument106 pagesCardiac Arrythmias in The ED Menbeu Edited From AnaTemesgen Geleta100% (1)
- ELECTROCARDIOGRAMDocument63 pagesELECTROCARDIOGRAMMbah GapinbissiPas encore d'évaluation
- Cardiac Arrhythmias: A. Supraventricular TachyarrhythmiaDocument10 pagesCardiac Arrhythmias: A. Supraventricular TachyarrhythmiaSarah RepinPas encore d'évaluation
- 28,29 Management of Cardiac ArrhythmiasDocument41 pages28,29 Management of Cardiac ArrhythmiasSL Dr ChEMiSPas encore d'évaluation
- ECG Case Studies Moosa1.Document54 pagesECG Case Studies Moosa1.m.ikhsan.adi.nugrahaPas encore d'évaluation
- Presentation of Cardiac ArrhythmiasDocument64 pagesPresentation of Cardiac ArrhythmiasMohd Anisul KarimPas encore d'évaluation
- Arrythmia Chapter - 005 Patho 2017Document49 pagesArrythmia Chapter - 005 Patho 2017diwabi3331Pas encore d'évaluation
- N12 Cardiac DysrhythmiasDocument68 pagesN12 Cardiac Dysrhythmiaskathbondoc03Pas encore d'évaluation
- Ecg Interpretation New TemplateDocument88 pagesEcg Interpretation New TemplateJonathan NgPas encore d'évaluation
- Cardiac Rhythm and Related Disorders: - Marshell Tendean, MD - Department of Internal Medicine UKRIDA JakartaDocument50 pagesCardiac Rhythm and Related Disorders: - Marshell Tendean, MD - Department of Internal Medicine UKRIDA JakartavaiyenPas encore d'évaluation
- ECG Guide: Anatomy, Physiology, Interpretation and AbnormalitiesDocument102 pagesECG Guide: Anatomy, Physiology, Interpretation and AbnormalitiesMustafa A. DawoodPas encore d'évaluation
- DR Jess Feltcher - Palpitations in General Practicce - 0Document49 pagesDR Jess Feltcher - Palpitations in General Practicce - 0aim1997Pas encore d'évaluation
- Cardiac Arrhythmias in ChildrenDocument50 pagesCardiac Arrhythmias in ChildrenNorhafizah AhmadPas encore d'évaluation
- 3881 - Prosedur Pendaftaran Internship Per November 2016Document57 pages3881 - Prosedur Pendaftaran Internship Per November 2016Munawir_Syam91Pas encore d'évaluation
- Dysrhythmia Recognition Pocket Reference Card PDFDocument14 pagesDysrhythmia Recognition Pocket Reference Card PDFjenn1722100% (2)
- Internal Medicine NotesDocument26 pagesInternal Medicine NotesPierce ArthurPas encore d'évaluation
- CPG Management of Atrial Fibrillation PDFDocument119 pagesCPG Management of Atrial Fibrillation PDFZee YongPas encore d'évaluation
- PseudodementiaDocument10 pagesPseudodementiarazorazPas encore d'évaluation
- Acs 20 ReviewDocument7 pagesAcs 20 ReviewrazorazPas encore d'évaluation
- R C S I D R A F T M e D I C A L G R A D U A T e P R o F I L eDocument8 pagesR C S I D R A F T M e D I C A L G R A D U A T e P R o F I L erazorazPas encore d'évaluation
- True But TrueDocument20 pagesTrue But TruerazorazPas encore d'évaluation
- GKM Final Year Book ClearanceDocument6 pagesGKM Final Year Book Clearancerandom.mail.scsm7112Pas encore d'évaluation
- Laser Treatment For Varicose VeinsDocument5 pagesLaser Treatment For Varicose VeinsrazorazPas encore d'évaluation
- Literature Review of Bariatric Surgery For The Treatment of Morbid ObesityDocument1 pageLiterature Review of Bariatric Surgery For The Treatment of Morbid ObesityrazorazPas encore d'évaluation
- Registration FormDocument2 pagesRegistration FormrazorazPas encore d'évaluation
- NEJM Protocol Sample 1Document86 pagesNEJM Protocol Sample 1razorazPas encore d'évaluation
- PG Respiratory Summit Registration Form 2013Document2 pagesPG Respiratory Summit Registration Form 2013razorazPas encore d'évaluation
- Cataract LectureDocument7 pagesCataract LecturerazorazPas encore d'évaluation
- Dangerous Diplopia - PansinusitisDocument4 pagesDangerous Diplopia - PansinusitisrazorazPas encore d'évaluation
- RCPI Management of Early Pregnancy MiscarriageDocument24 pagesRCPI Management of Early Pregnancy MiscarriagerazorazPas encore d'évaluation
- How To Write A Great Research Paper by Simon Peyton JonesDocument46 pagesHow To Write A Great Research Paper by Simon Peyton JonesrazorazPas encore d'évaluation
- CVR02 - EcgDocument3 pagesCVR02 - EcgrazorazPas encore d'évaluation
- Gut 2013 - 23 - 25th August 2013, PenangDocument12 pagesGut 2013 - 23 - 25th August 2013, PenangPierce ChowPas encore d'évaluation
- In Austere Financial Times, Which Procedures Should Be Rationed and Who Should Decide?Document13 pagesIn Austere Financial Times, Which Procedures Should Be Rationed and Who Should Decide?razorazPas encore d'évaluation
- Cataract LectureDocument7 pagesCataract LecturerazorazPas encore d'évaluation
- Surgical Safety ChecklistDocument8 pagesSurgical Safety ChecklistrazorazPas encore d'évaluation
- PneumoniaDocument37 pagesPneumoniarazorazPas encore d'évaluation
- The Medical Short Case Preview 2011Document20 pagesThe Medical Short Case Preview 2011Lim Thien Thien100% (2)
- ETHICON Encyclopedia of Knots (Noduri Chirurgicale PDFDocument49 pagesETHICON Encyclopedia of Knots (Noduri Chirurgicale PDFoctav88Pas encore d'évaluation
- NSAIDsDocument2 pagesNSAIDsrazoraz100% (1)
- Secrets Alto Sax MelodyDocument3 pagesSecrets Alto Sax MelodyrazorazPas encore d'évaluation
- GCE Biology Unit 6 TSM Final (Unit 6 Guide and Examples From Edexcel)Document76 pagesGCE Biology Unit 6 TSM Final (Unit 6 Guide and Examples From Edexcel)razoraz90% (10)
- Practice Quiz (50 Questions) - You Scored 2 Out of 50. Your Performance Has BeenDocument35 pagesPractice Quiz (50 Questions) - You Scored 2 Out of 50. Your Performance Has BeenMelodia Turqueza GandezaPas encore d'évaluation
- Autopsy Lecture 7 Embalm, Artif, NegatDocument51 pagesAutopsy Lecture 7 Embalm, Artif, NegatAbdul WahabPas encore d'évaluation
- Pptchapter12 130806074658 Phpapp01Document54 pagesPptchapter12 130806074658 Phpapp01Aaron WallacePas encore d'évaluation
- Responsi Stemi Dr. Tuko SP - JP FixDocument56 pagesResponsi Stemi Dr. Tuko SP - JP FixcintaPas encore d'évaluation
- Tissues Organs and Systems-9 7 15Document2 pagesTissues Organs and Systems-9 7 15api-294498352100% (1)
- Emotions and Body ChemicalsDocument24 pagesEmotions and Body ChemicalsJanani Anbalagan100% (3)
- Mbbs PBL BibleDocument76 pagesMbbs PBL Biblejoshy2211960% (1)
- Health g11 WK 1 Module 1Document9 pagesHealth g11 WK 1 Module 1Angel BoquecosaPas encore d'évaluation
- Body Fluids BloodDocument31 pagesBody Fluids BloodHardy Allen L. VillarosaPas encore d'évaluation
- Secretin Activated Brown Fat Mediates Prandial Thermogeneis To Induce Satiation (Study Aim)Document12 pagesSecretin Activated Brown Fat Mediates Prandial Thermogeneis To Induce Satiation (Study Aim)Geetika PremanPas encore d'évaluation
- Raga Todi Bringing Down Blood PressureDocument8 pagesRaga Todi Bringing Down Blood Pressureami1967Pas encore d'évaluation
- Respiration, - Characteristics N Factors Affecting RespirationDocument2 pagesRespiration, - Characteristics N Factors Affecting RespirationShalabh JoharyPas encore d'évaluation
- Coronary Circulation: by Sridip HaldarDocument19 pagesCoronary Circulation: by Sridip HaldarPercy JacksonPas encore d'évaluation
- Model Answer of Formative Written OSCADocument6 pagesModel Answer of Formative Written OSCAAhmed SamahaPas encore d'évaluation
- Bishop (2011) RSA Part 1Document23 pagesBishop (2011) RSA Part 1Nicolás BastarricaPas encore d'évaluation
- Anesthesiology and Intensive Care Medicine Answers For ExamDocument94 pagesAnesthesiology and Intensive Care Medicine Answers For Exammichal ben meronPas encore d'évaluation
- GCSE Edexcel Biology B1 Y9 Final Exam 13 - 14 PDFDocument10 pagesGCSE Edexcel Biology B1 Y9 Final Exam 13 - 14 PDFPaul BurgessPas encore d'évaluation
- Worksheet-No-1-Overview-of-Anatomy-and-Physiology-1Document5 pagesWorksheet-No-1-Overview-of-Anatomy-and-Physiology-1Lyca VillordonPas encore d'évaluation
- Science: Quarter 3 - Module 3: The Nervous System and Feedback MechanismsDocument34 pagesScience: Quarter 3 - Module 3: The Nervous System and Feedback MechanismsViktor InocPas encore d'évaluation
- Quiz 5: Tests & QuizzesDocument4 pagesQuiz 5: Tests & QuizzesmadelinePas encore d'évaluation
- 10 Things Great Sleepers DoDocument24 pages10 Things Great Sleepers DoCesar AraucoPas encore d'évaluation
- NCP 3rd YearDocument6 pagesNCP 3rd YearTotoro AblogPas encore d'évaluation
- Blood Pressure Levels For Boys by Age and Height Percentile: BP (Percentile) Systolic BP (MMHG) Diastolic BP (MMHG)Document4 pagesBlood Pressure Levels For Boys by Age and Height Percentile: BP (Percentile) Systolic BP (MMHG) Diastolic BP (MMHG)melese woldehawariatPas encore d'évaluation
- Complete Physical Exam GuideDocument12 pagesComplete Physical Exam GuideMarianPas encore d'évaluation
- Dutra de Souza 2023Document11 pagesDutra de Souza 2023Paulo Emilio Marchete RohorPas encore d'évaluation
- Week 4 - Ms1 Course Task - Cu 4 - RoveroDocument2 pagesWeek 4 - Ms1 Course Task - Cu 4 - RoveroJohnmarkLorenzanaRoveroPas encore d'évaluation
- Hand Out 3 Respiratory System Overview PDFDocument12 pagesHand Out 3 Respiratory System Overview PDFGrape JuicePas encore d'évaluation
- Cardiology BookDocument401 pagesCardiology BookOana100% (5)
- Management of Hypertensive EmergencyDocument17 pagesManagement of Hypertensive EmergencyGiovanna AlguPas encore d'évaluation
- 5 Step EKG InterpretationDocument1 page5 Step EKG InterpretationSibel ErtuğrulPas encore d'évaluation