Académique Documents
Professionnel Documents
Culture Documents
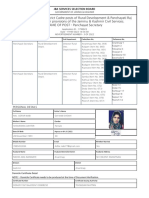
Tarun
Transféré par
Tarun MathurTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Tarun
Transféré par
Tarun MathurDroits d'auteur :
Formats disponibles
Dr.
Tarun Mathur
MITOCHONDRIAL DISORDERS
Mitochondria & Mt DNA
Mitochondrial disorders
Genetics
Pathophysiology
Approach to Diagnosis & Diagnostic criteria
TREATMENT
What is a Mitochondrion?
Cellular organelle of endosymbiotic origin residing in the cytosol of most
nucleated (eurkaryotic) cells.
Produces energy by oxidising organic acids and fats with oxygen by
oxidative phosphorylation and generates oxygen radicals (reactive oxygen
species ROS )as a toxic by-product
POWER HOUSE OF THE CELL
First observed > 100 years ago by Altmann, who named them `elementary
organisms'
MITOCHONDRIAL DNA
In 1963, Nass and Nass discovered mt DNA.
Complete sequences of mtDNA reported in 1981.
In 1988 first disease-causing mutations of mtDNA was found
16, 569-np double-stranded.
Closed, circular molecule
Located within the matrix.
37 Genes:
13 for OXPHOS Enzymes
22 for tRNA
2 for rRNA
1. Maternal inheritance
Most of the mtDNA come from the egg, to contrast, the sperm have
few mtDNA.
The characteristics of the mtDNA
Mitochondrial inheritance.
Sperm mitochondria are shed before
entry of the sperm nucleus. All
mitochondrial in the zygote are
contributed by the egg cell
2. High mutation rate
Bareness of
mtDNA
No mechanism
of repair
rate
nDNA1020 times
Somatic cell
mutation
Germ cell
Abnormal
mtDNA
Normal
mtDNA
Heteroplasmy both normal and abnormal mtDNA are contained in the
same cell or tissue.
Homoplasmy either normal or abnormal mtDNA is contained in the
same cell or tissue.
3. Heteroplasmy/homoplasmy
Concept of heteroplasmy
Both wild-type and mutant (gray) mitochondria are included in the hundreds
of mitochondria in a cell. These mitochondria segregate passively when the
cell divides. This can lead to variation in the proportion of affected
mitochondria in different tissues or different individuals in a family
4. Semiautomous organelle
Mitochondria has its own genetic material, and has the
capability of duplication, transcription and translation.
5. Effect of threshold
The energy supply is not impacted seriously when there is only
little mutant mitochondria in the cell or tissues. When there is
large amount of abnormal mitochondria, the energy supply will
be impacted seriously enough to cause the cell out of function.
Effect of threshold
Defects in DNA outside the chromosomesin cell structures
called mitochondriacan cause an array of disorders,
perhaps including many that debilitate the elderly
by Douglas C. Wallace
Mitochondrial DNA as a Forensics Tool
On September 3, 1996, in Chattanooga, Tenn., a 27-yearold man
was found guilty of murdering a four-year-old girl.
He was convicted largely on the strength of an analysis that
matched mitochondrial DNA from his saliva to that from hair
recovered on his victim.
His case was the first in which mitochondrial DNA evidence was
allowed into the courtroom.
Why Mitochondrial DNA Is Needed?
Imagine a major city with half its power plants
shut down. At best, such conditions would
produce a "brown out" with large sections of
the city working far below optimum efficiency
Applying this to human body:
Now imagine human body with one-half of its energy producing facilities
shut down.
The brain would be impaired, vision would be dim, muscles would twitch
spastically or would be too weak to allow body to walk or write, heart
would be weakened, and you would not be able to eat and digest your
food.
For large numbers of people, especially children, this is precisely the
situation in which they find themselves due to defects in the mitochondria.
Mitochondrial diseases compromise their lives and can be fatal.
Mitochondria produce energy by relaying electrons from food down the
respiratory chaina series of protein complexes (IIV) in the mitochondrial
inner membrane.
Thirteen proteins in the complexes are specified by genes in mitochondrial
DNA
Respiratory chain is composed of complexes located at the inner mitochondrial
membrane:
Complex I: NADH ubiquinone reductase
Complex II: succinate: ubiquinone oxidoreductase
Complex III: ubiquinol cytochrome c reductase
Complex IV: cytochrome C oxidase
Complex V: ATP synthase
Final goal: production of ATP
Respiratory chain proteins are synthesized from two different genomes: mtDNA
and nDNA
mtDNA encodes 13 respiratory chain polypeptides, 2 rRNAs and 22 tRNAs
nDNA encodes the majority of respiratory chain polypeptides
Primary mitochondrial diseases are the consequence of dysfunctions of both
mitochondrial and nuclear genes either separately or in combination.
Oxidative phosphorylation (OXPHOS) is defective.
Most common deficiencies affect complexes I and IV.
Classification of MIDs.
Molecular genetics of main mitochondrial disorders
mtDNA mutations
large-scale rearrangements
deletions Chronic progressive external ophtalmoplegia (CPEO), Kearns-Sayre
syndrome (KSS), Pearson syndrome (marrow-pancreas syndrome)
duplications
Point mutations in tRNAs or rRNAs
MELAS
MERRF
Mitochondrial cardiomyopathy and myopathy
Point mutations in protein coding genes
ATP6 mutations: NARP, Leigh syndrome
Complex I mutations: Leber hereditary optic atrophy (LHON)
Complex IV (COX) subunit mutations
Nuclear gene mutations
Autosomal dominant and autosomal recessive progressive external
ophtalmoplegia (AdPEO, ArPEO)
MNGIE: myogastrointestinal encephalopathy: mutations in thymidine
phosphorylase gene (22q13)
Wolfram syndrome (DID-MOAD): mutations in wolframin gene (4p16) associated
with large scale mtDNA deletions
Leigh syndrome caused by nuclear gene mutations affecting complexes I, II or IV
Infantile hypertrophic cardiomyopathy and encephalomyopathy: mutations in
SCO2 gene
Mutations in other mitochondrial protein genes
Hereditary spastic paraplegia linked to 16q24
Friedreich ataxia, mutations in the frataxin gene in 9q13
Mitochondrial diseases affecting nervous system and muscle
Pathophysiology of
Mitochondrial disorders
Early logic suggested that compromising mitochondrial ATP production
harms/kills cells causing symptoms.
In 1962 Rolf Luft and coworkers at the Karolinska Institute and University
of Stockholm reported that an impairment in mitochondrial energy
production caused a debilitating disorder.
Eventually it became clear that the tissues and organs most readily
affected by cellular energy declines are the CNS, followed, in descending
order of sensitivity, by heart and skeletal muscle, the kidneys and
hormone-producing tissues.
EVERY CELL IN THE BODY contains hundreds of mitochondria, the power
plants of cells.
A single mitochondrion contains several loops of DNA, each of which
includes 37 genes(24+13) involved in energy generation.
Mutations in mitochondrial genes are inherited solely from mothers.
Consequently, if a fertilized egg carries a mutation in some fraction of its
mt DNA (a condition known as heteroplasmy), one daughter cell may
inherit a larger proportion of mitochondria bearing mutant DNAs, and the
other cell may inherit a larger percentage of mitochondria bearing normal
DNAs.
The laws of probability dictate that as the cells continue to reproduce, the
mitochondrial DNA populations in the emerging daughter cells will move
toward uniformity (homoplasmy), tending to consist of predominantly
normal or predominantly mutant molecules.
MtDNA-related disorders may manifest as a forme fruste lesions at an
early age and shift from one phenotype to another as they grow older.
For example, a patient with MELAS may present with only episodic
headache in childhood, but with strokelike episodes and neurological
deficits as they age and the pathogenic mutations accumulate in brain and
cerebral vasculature.
Some "Rules of Thumb" of when to think mitochondria:
1. A "common disease" (i.e. autism, cerebral palsy, lots of others) has
atypical features that set it apart from the pack.
2. Three or more organ systems are involved.
3. Recurrent setbacks or flares in a chronic disease occur.
Mitochondrial News, Spring 2000 Issue by Dr. Robert K. Navaiaux.
Any disease. Any organ. Any age. best general summary of the spectrum
of mitochondrial disease available (Christodoulou 1999).
Mitochondrial diseases are notorious masqueraders (Kerr 1998).
Symptoms are indistinguishable from those caused by common disorders.
Only the behavior of the mitochondrial disease over time sets it apart
from its more common cousins.
Even a single point mutation in mt DNA can produce many different
diseases.
eg. A3243G mutation first linked to MELAS
Some patients first suffered psychiatric disease and hearing loss
early onset dementia in their 30s
unexplained cardiomyopathy and mildly elevated lactate
An observant parents evidence may be disproved but should never be ignored
Lancet 1:688, 1951, Anonymous
Striking Features of the Diseases
Frequently inherited.
Occasionally arise spontaneously in an egg or early in embryonic
development.
The latter mutations, like inherited ones, can become widely
distributed in the body as the fetus develops, in which case they
may produce rather profound effects.
(contd.)
Mt DNA mutations can also form in tissues throughout life, in different
cells and even in different mitochondrial DNA molecules in a single cell.
These changes are called somatic mutations.
Accumulation of somatic mutations explains two features .
People born with mt DNA mutations often become ill only after a
delay of years or sometimes decades, and
Their conditions usually worsen over time.
Many inherited mutations affect mitochondrial function only subtly, allowing
tissues throughout the body to produce the energy they need, at least for a time.
Buildup of random, somatic mutations in a lifetime further depresses energy
production, until eventually a given tissues energy level falls too low to allow
normal operations to continue.
Then the tissue begins to perform improperly, and symptoms emerge.
As a rule, a severe mt DNA mutationone that suppresses energy production
causing life threatening disease early onwill turn out to be heteroplasmic; that
is, the mutant gene will be found to coexist in the patients tissues with the normal
version of the gene.
Various inherited mutations substitute a solitary base pair for another in a
protein-coding gene, thereby causing an incorrect amino acid to replace a
correct one in the encoded protein.
One such missense mutation offers a striking illustration of the principle
that a heteroplasmic mitochondrial DNA mutation can often express itself
in disparate ways in different people.
For a family in which 4 generations were available for study, the same
mutation caused several individuals to suffer mild retinal degeneration in
the peripheryof their visual field (retinitis pigmentosa), another person to
undergo severe retinal and CNS degeneration, and two ill-fated boys to
acquire a potentially lethal childhood disease known as Leighs syndrome.
Evidently the differences in symptomatology within this family stemmed
to a great extent from differences in the percentages of mutant
mitochondrial DNA molecules in the patients tissues.
Those with higher percentages had lower ATP production and more
extensive disease.
APPROACH TO THE DIAGNOSIS OF
MITOCHONDRIAL DISORDERS
The overall clinical spectrum of mitochondrial disorders is wide.
1
st
, is detailed family history suggesting maternal inheritance.
2
nd
, seemingly unrelated and confusing multisystem problems, both
clinical and subclinical, suggest mitochondrial disease, because
mitochondria are present in all tissues and organ systems.
3
rd
, rare abnormalities, often not seen with other diseases, can be of
mitochondrial origin. For instance, strokes in children or young adults,
especially associated with other neurological abnormalities, might indicate
MELAS.
4
th
, a combination of neuropathy and myopathy in one patient suggests
mitochondrial disease.
5
th
, history of flare up with intercurrent illnesses, trauma, or surgery.
WHEN TO SUSPECT MITOCHONDRIAL DISEASE
Red Flags:
Mitochondrial disease may present with any symptom in any organ at any
age, but some symptoms and signs truly are more suggestive of a
mitochondrial disorder than others.
These red-flag features warrant the initiation of a baseline diagnostic
evaluation for mitochondrial disease
Red-Flag Findings in Mitochondrial Disease
Neurologic
Cerebral stroke-like lesions in a nonvascular pattern
Basal ganglia disease
Encephalopathy: recurrent or with low/moderate dosing of valproate
Neurodegeneration
Epilepsia partialis continua
Myoclonus
Ataxia
MRI findings consistent with Leigh disease
Characteristic MRS peaks
Lactate peak at 1.3 ppm TE (time to echo) at 35 and 135
Succinate peak at 2.4 ppm
Ophthalmologic
Retinal degeneration with signs of night blindness, color-vision deficits,
Decreased visual acuity, or pigmentary retinopathy
Ophthalmoplegia/paresis
Fluctuating, dysconjugate eye movements
Ptosis
Sudden- or insidious-onset optic neuropathy/atrophy
Other
A newborn, infant, or young child with unexplained hypotonia, weakness,
failure to thrive, and a metabolic acidosis (particularly lactic acidosis)
Exercise intolerance that is not in proportion to weakness
Hypersensitivity to general anesthesia
Episodes of acute rhabdomyolysis
Proposed major diagnostic criteria for
mitochondrial disease diagnosis
Clinical:
Clinically complete mitochondrial encephalomyopathy or mitochondrial cytopathy
defined as fulfilling all three of the following conditions.
a) Unexplained combination of multisystemic symptoms ,essentially pathognomonic
for a respiratory chain (RC) disorder.
b) Symptoms must include at least three of the organ system presentations.
c) A progressive clinical course with episodes of exacerbations OR a family history
that is strongly indicative of mtDNA mutation.
d) Exclusion of other metabolic or non-metabolic disorders.
Histology:
(a) > 2% ragged-red fibers in skeletal muscle
Enzymology:
(a) 2% COX-negative fibers if < 50 years of age
(b) 5% COX-negative fibers if > 50 years of age
(c) < 20% activity of any RC complex in a tissue
(d) < 30% activity of any RC complex activity in a cell line
(e) < 30% activity of the same RC complex activity in more than two tissues
(enzyme activities represent percentage of normal control mean relative to an
appropiate reference enzyme such as citrate synthase or RC complex II)
Minor diagnostic criteria
Clinical:
a) Symptoms compatible with a RC defect
Histology:
a) 1% - 2% ragged-red fibers if aged 30 50 years
b) Any ragged-red fibers if < 30 years of age
c) > 2% subsarcolemmal mitochondrial accumulations in a patient < 16 years of age
d) Widespread electron microscopic abnormalities in any tissue
Enzymology:
a) Antibody based demonstration of a defect in RC complex expression
b) 20% - 30% activity of any RC complex in a tissue
c) 30% - 40% activity of any RC complex in a cell line
d) 30% - 40% activity of the same RC complex activity in more than two tissues
Functional:
a) Fibroblast ATP synthesis rates 2 3 SD below mean
b) Fibroblasts unable to grow on media with glucose replaced by galactose
Molecular:
a) Identification of nuclear or mtDNA mutation of probable pathogenicity
Metabolic:
a) One or more metabolic indicators of impaired RC function
*Diagnostic criteria proposed by Bernier et al (2002)
Stepwise procedure for the diagnostic work-up of mitochondriopathies
Laboratory Findings
The mitochondrial metabolic test battery includes :
Blood creatine kinase (CK): normal or mildly elevated in mitochondrial
myopathies.
Lactate and pyruvate:
increase in lactate and lactate: pyruvate ratio (normal ratio: < 20:1).
normal values do not exclude mitochondrial disease.
Generally normal or only mildly elevated blood lactate levels
Plasma carnitine: often decreased in mtDNA-related disorders, with relative
increase in acylcarnitine levels.
Blood and urine amino acids
Urine organic acids, and
Cerebrospinal fluid (CSF) lactate and pyruvate (if the CNS is involved):
Measurement of lactate levels in CSF or brain (by proton magnetic resonance
spectroscopy [MRS]) may be helpful.
Ratio of phosphocreatine (PCr) to inorganic phosphate (Pi)
with mitochondrial dysfunction, PCr/Pi ratios are lower than normal at
rest, decrease excessively during exercise, and return to baseline values
more slowly than normal controls.
not suitable for infants and young children because it requires a high
degree of cooperation.
Neuro-ophthalmology
4 most common neuro-ophthalmological abnormalities seen in
mitochondrial disorders are
Leber's hereditary optic neuropathy (LHON),
Progressive external ophthalmoplegia (PEO),
Pigmentary retinopathy, and
Retrochiasmal vision loss
The most common pigmentary retinopathy appearance in mtDNA-related
diseases is that of salt-and-pepper retinopathy that typically becomes
more prominent with advancing age.
Neuroradiology
Brain MRI, facilitated detection .
Brain atrophy common in children with Mt disease.
Basal ganglia calcification common in KSS and MELAS, and diffuse signal
abnormalities of the white matter are characteristic of KSS and MNGIE.
The diagnosis of MELAS relies on radiographic observation of strokelike.
strokelike because they do not conform to the anatomical territories
predominantly involve cortical gray matter.
initial or predominant lesions characteristically in the posterior cerebral
hemisphere.
LS characteristically shows bilateral hyperintense signals on T2-weighted
and fluid-attenuated inversion recovery (FLAIR) MRIs in the putamen,
globus pallidus, and thalamus.
Girl with MELAS at ages 8 & 13 years.
A),T2-weighted coronal image during an acute strokelike episode shows parasagittal bilateral
hyperintense lesions (arrows) at the age of 8 years.
B),T2-weighted coronal image 2 months later shows that lesions have almost entirely resolved.
Cerebellar atrophy is evident.
C),T2-weighted axial image 5 years later, during a prolonged seizure, shows a new hyperintense
lesion in the left parietooccipital region (arrow).
1&12-year-old girl with Leigh syndrome. A), T1-weighted axial image shows
swollen,hypointense putamina with areas of hyperintensity within the lesions
.B), T2weighted axial image shows hyperintensity and swelling in the putamina.
13-year, girl with Kearns-Sayre syndrome.,T1-
weighted (A) and proton densityweighted (B)
axial images show hyperintensity of the caudate
nuclei, globus pallidi, and medioposterior
thalami.
C, T2-weighted coronal image displays white
matter hyperintensity extending to the
subcortical U fibers and involving the cerebellar
white matter. High-signal lesions are seen
within the posterior medulla oblongata (arrow).
D, T2-weighted axial image shows
hyperintensity of the posterior columns of the
medulla oblongata (arrow) and cerebellar white
matter
Proton MR Spectroscopy in the Diagnostic Evaluation of Suspected Mt Disease
Detection of CNS lactate by MR spectroscopy is useful in diagnosis.
MR spectroscopy does not depict elevated lactate in all cases.
Abnormal CNS concentrations of lactate may be undetected by MR spectroscopy
because of differences in the type of mitochondrial disorder, timing, severity, or
location of the affected tissues and the site of interrogation.
Images from the case of a 31-year-old man with MELAS syndrome, which was documented by a
point mutation in the Mt tRNA (Leu).
T2 MRIshows a large focal hyperintensity in the left parietal region, predominantly affecting the
gray matter. This area corresponds to elevated choline (Cho), decreased N-acetylaspartate
(NAA), and markedly elevated lactate (Lac) on the multisection spectroscopic imaging metabolic
maps.
In addition, multisection spectroscopic images show globally elevated lactate, which is greatest in
the left parietal strokelike lesion, next highest in the remaining gray matter (G.M.) and CSF, and
lowest in the white matter.
Muscle Biopsy
Many histopathological abnormalities are non-specific .
Hallmark feature is the ragged-red fibers.
Modified Gomori trichrome stains subsarcolemmal and intermyofibrillar
mito-chondria as bright red masses against the background of the blue
myofibrils.
Succinate dehydrogenase , (fibres stain intensely blue) is more sensitive
than the MGT in detecting mitochondrial proliferation.
NADH-tetrazolium reductase (NADH-TR) stains mitochondria-rich fibers
more intensely, but less specific than SDH for mitochondria.
(1) Red-ragged fibers MGT
(2) Increased oxidative enzyme activity SDH.
(3) Increased oxidative enzyme activity NADH TR
Red aggregates as seen in mitochondrial myopathies stained with trichrome
RRFs can occur in
inclusion body myositis
normal aging.
toxic myopathy of zidovudine
Stain very helpful in evaluating patients with mitochondrial disorders is
cytochrome oxidase (COX) activity.
RRFs are commonly COX-negative.
COX-SDH histochemical stain ,stain blue against a background of normal
brown fibers that have both COX and SDH.
Absence of either RRFs or COX-negative fibers does not rule out
mitochondrial disease.
Immunohistochemistry and Immunoblots
Immunohistochemical studies using anti-bodies specifically against mtDNA- or
nDNA-encoded proteins can define whether the disorder is related to the
mitochondrial or nuclear genome.
Electronmicroscopy
Subsarcolemmal and intermyofibrillar proliferation of mitochondria and the
presence of abnormal mitochondria in muscle fibers.
Blue Native Polyacrylamide Gel Electrophoresis
Powerful tool for the analysis of the OXPHOS complexes.
DNA-Based Diagnosis
A large number of mtDNA and nDNA mutations are now known to cause mitochondrial
disorders and their number, especially nDNA gene mutations, continues to rise in recent years
MAJOR MITOCHONDRIAL CLINICAL
SYNDROMES
Mitochondrial Encephalomyopathy, Lactic Acidosis, and Strokelike Episodes
(MELAS)
In 1975 a syndrome consisting of lactic acidosis and mitochondrial myopathy
was described in two separate reports.
The acronym MELAS was proposed in 1984.
One of MC maternally inherited mitochondrial disorders, caused by
decreased ability of cells to produce sufficient ATP.
Incidence is unknown.
Most frequent A-to-G point mutation at the 3243 position in the mt DNA.
Onset generally in childhood or early adult life.
Broad range of clinical manifestations , highly variable course.
Diagnosis of exclusion.
The classic neurologic characteristics include encephalopathy, seizures, and stroke-like
episodes.
Multisystem effects including cardiac conduction defects, diabetes mellitus, short
stature, myopathy, and gastrointestinal disturbances.
The unique radiological feature is that the stroke involves the cerebral cortex, sparing
the white matter, mostly in the parietal and occipital regions.
Criteria for Diagnosing MELAS Syndrome
Number of Criteria Signs and Symptoms
6 core features (present
in 90% of cases)
Age of symptom onset < 40 yrs
Encephalopathy,frequently manifesting as seizures,
dementia, or both
Exercise intolerance
Lactic acidosis
Ragged-red fibers on biopsy
Stroke-like episodes (before age 40 yrs)
3 additional features,
with at least 2 required
to confirm diagnosis
Normal early development
Recurrent headache
Recurrent vomiting
Myoclonic Epilepsy with Ragged-Red Fiber Myopathy
Usually beginning in childhood, but onset may occur in adulthood.
The classic features of MERRF include:
Myoclonus most characteristic symptom
Epileptic seizures
Ataxia
Ragged-red fibers
Additional symptoms may include: hearing loss, lactic acidosis , short stature,
exercise intolerance ,dementia, cardiac defects, eye abnormalities, and speech
impairment.
Few cases are sporadic but most are maternally inherited due to a mutation
within the mitochondria, A8344G, accounting for over 80% of the cases
Mitochondrial Neurogastrointestinal Encephalomyopathy
Autosomal recessive disease with secondary alterations of mtDNA.
Combination of ptosis, PEO, severe gastrointestinal dysmotility leading to
cachexia, Peripheral neuropathy, leukoencephalopathy on brain MRI , and
evidence of mitochondrial dysfunction (e.g., lactic acidosis or RRF in muscle
biopsy)
Onset is usually in the late teens and most patients die before age 40.
mutations in the gene encoding thymidine phosphorylase.
Subacute Necrotizing Encephalomyelopathy (Leigh's Syndrome)
First reported in 1951 by Denis Leigh , a British neuropathologist.
Onset in >50% is in 1
ST
year of life, mostly before 6
TH
month . Late-onset also
reported.
Characterized by psychomotor regression, muscular hypotonia, brainstem signs
(especially strabismus, nystagmus and swallowing difficulties), ataxia, pyramidal signs,
respiratory insufficiency, lactate acidemia and acute deterioration following common
infections.
Dysfunction of the RC enzymes due to defects in genes for the PDC, cytochrome-c
oxidase, ATP synthase subunit 6, or subunits of mitochondrial complex I is responsible
in majority .
X-linked recessive, autosomal recessive, and mitochondrial.
The most characteristic neuro-radiological findings are bilateral, symmetric
focal hyperintensities in the basal ganglia, thalamus, substantia nigra, and
brainstem nuclei .
In the basal ganglia, the putamen is particularly involved.
Progressive External Ophthalmoplegia and Kearns-Sayre Syndrome
KSS is defined by the triad of PEO, onset before age 20, and at least one of the following:
short stature, pigmentary retinopathy, cerebellar ataxia, heart block, and elevated CSF
protein (>100 mg/dL).
Neuropathy, Ataxia, Retinitis Pigmentosa Syndrome
relatively rare disorder due to point mutation at np-8993
Characterised by combination of SM neuropathy,cerebellar ataxia & night blindness.
Usually young adults
Clinical presentation includes combination of following symptoms:
Early salt & pepper retinopathy Hearing loss
Retinitis pigmentosa seizures
Sluggish pupils, nystagmus Ataxia
blindness Sensory neuropathy
Proximal musle weakness Developmental delay
CST Atrophy
dementia
TREATMENT APPROACHES:
Treatment of mitochondrial disease is mainly symptomatic, empiric, and palliative
Seizures
Management of seizures typically involves the use of common anticonvulsants
including phenobarbital, phenytoin, carbamazepine, gabapentin, lamotrigine,
benzodiazepines, and zonisamide.
Valproate has been identified as a potentially dangerous medication because of its
hepatotoxic side effect.
known to inhibit cytochrome oxidase (COX) as well as cause mitochondrial
ultrastructural changes.
Coenzyme Q10
lipophilic mobile electron carrier ,located in the inner mitochondrial
membrane.
Most widely used therapeutic agent in patients with mitochondrial disease
Oral CoQ
10
200600 mg/day for 1 year, recommended in adult patients with
mitochondrial disease. Pediatric dosage,215 mg/kg/day orally.
Mechanisms including
reversal of CoQ
10
deficiencies
enhancing activity of the respiratory chain in patients with inadequate
complex III activity.
increases the production of ATP.
antioxidant scavenging dangerous reactive oxygen species.
Potential effects of CoQ
10
in mitochondrial disorders
reduction of serum lactate and pyruvate levels,
improvement in cardiac conduction defects, and
improved eye movements.
reduced muscle weakness,
improved tolerance and oxygen utilization during exercise,
reduced peripheral nerve damage, and
improved neurologic function.
Mixed results, no sustained clinical benefits have been noted.
However, considered first-line therapy for patients with MELAS syndrome and
should be started after clinical diagnosis.
Drug interaction with warfarin & statins.
L-arginine
L-Arginine is a semiessential amino acid & a vasodilator .
one of the MC drugs included in treatment regimens for MELAS syndrome.
Adult and pediatric doses of L-arginine are equivalent.
In acute stroke, IV L-arginine hydrochloride 500 mg/kg is given within 30
minutes of onset& repeated every 6 hours until the desired effect has
been achieved and may be continued for 13 days.
Maintenance dose- 150300 mg/kg/day in 23 divided doses.
Electron Transport Chain Cofactors: B Vitamins
first-line agents in the treatment of MELAS syndrome.
Thiamine (vitamin B
1
)
Essential in carbohydrate metabolism.
active form, TPP , coenzyme increasing acetyl coenzyme A, for proper
functioning of the respiratory chain.
oral dose 50300 mg/day with no adverse events
improves myopathy as well as normalises creatine kinase, blood lactate, and
pyruvate levels.
Riboflavin (vitamin B
2
)
improvement in neurologic symptoms and exercise capacity with riboflavin
alone or in combination .
Dosage,50400 mg/day with no reported adverse reactions
Nicotinamide (vitamin B
3
)
Main metabolite NAD
+
.
Oral doses of may 50500 mg/day be used.
Creatine
Amino acid produced in liver from arginine and glycine, combines with
phosphate in the mitochondria forming phosphocreatine.
Creatine supplementation increases phosphocreatine in tissues, providing
increased energy stores.
Inhibit collagen-induced thrombocyte aggregation playing a role in preventing
stroke-like episodes.
20 g/day orally in 2 divided doses for 2 weeks followed by 210 g/day in
divided doses.
Levocarnitine
Common therapeutic modalitiy used in the treatment of MELAS syndrome.
1001000 mg orally 23 times/day.
Antioxidants
Ascorbic acid (vitamin C),
-tocopherol (vitamin E), and
Thiocitic acid (-lipoic acid) have been studied in patients with mitochondrial
disorders.
Idebenone
Synthetic analog of CoQ
10
, an electron carrier in the mitochondrial respiratory chain
stimulating ATP formation.
Antioxidant capabilities.
Approved in Japan for the treatment of MELAS syndrome but is not available in the
United States.
90270 mg/day orally have been used in adults.
Sodium dichloroacetate
improve lactic acidosis by decreasing pyruvate availability for conversion into
lactate.
improved energy production due to an increase in the supply of substrates used by
complex I.
2550 mg/kg/day orally administered in 2 divided doses.
Unfortunately, despite lowering of serum and/or CSF levels of lactate, DCA
treatment does not universally lead to overall clinical improvement
Cytochrome c
Cofactor in the mitochondrial respiratory chain
Cytochrome c is not commercially available and is rarely used to treat MELAS
syndrome.
No adverse effects have been reported
Corticosteroids
including dexamethasone 1216 mg/day, prednisone 24 mg/kg/day, and
methylprednisolone 1 g/day have been used in the treatment of MELAS syndrome.
Three therapeutic strategies look promising:
(i) allogeneic hematopoietic stem cell transplantation in MNGIE (mitochondrial
neurogastrointestinal encephalomyopathy);
(ii) bezafibrate, an activator of PGC-1alpha, has proven effective in animal models
of mitochondrial myopathy; and
(iii) Pronucleus transfer into a normal oocyte is effective in eliminating maternal
transmission of mtDNA, thus preventing the appearance of mtDNA-related
disorders.
Reports that cytochrome c oxidase deficiency can be reversed by the
supplementation of copper in cultured cells with a mutation in SCO2, a copper
chaperone, suggest that copper supplementation may be useful in some patients.
For the mtDNA-related disorders, the most promising approach is to reduce the
ratio of mutated to wild-type genomes (gene shifting), by pharmacologic,
physiological,or even surgical approaches.
Think mitochondria WHEN :
1. A "common disease" (i.e. autism, cerebral palsy, lots of others) has
atypical features that set it apart from the pack.
2. Three or more organ systems are involved.
3. Recurrent setbacks or flares in a chronic disease occur.
REFERENCES
Bradley: Neurology in Clinical Practice, 5th ed.
Adams & Victors Principles of Neurology, 9th Edition
Review article ,NEJM;Mechanisms of diseaseMitochondrial Respiratory-Chain
Diseases By Salvatore DiMauro, M.D., and Eric A. Schon, Ph.D.
Mitochondrial Disease: A Practical Approach for Primary Care PhysiciansRichard
H. Haas, MB, BChir, MRCP, Sumit Parikh, MD, Marni J. Falk, MD, Russell P. Saneto,
DO, PhD, Nicole I. Wolf, MD Niklas Darin, MD,Bruce H. Cohen, MD
Diagnosis of mitochondrial diseases: Clinical and histological study of sixty
patients with ragged red fibers Sundaram Challa, Meena A. Kanikannan, Murthy
M. K. Jagarlapudi, Venkateswar R. Bhoompally,Mohandas Surath
Mitochondrial medicine recent advances C. GRAFF, D. A. CLAYTON & N.-G.
LARSSON
MCQ,S
1)All are true about Mitochondrial DNA Except
1. 16, 569-np single stranded.
2. closed, circular molecule
3. located within the mitochondrial matrix
4. encodes for 13 polypeptides of the RC
2)Characteristic features of Mt DNA are
1. Maternal Inheritance
2. Bottle neck effect
3. High Mutation Rate
4. All the Above
3) large-scale rearrangements in MtDNA seen in ALL Except
1. Chronic progressive external ophtalmoplegia (CPEO)
2. Kearns-Sayre syndrome (KSS)
3. MELAS
4. Pearson syndrome
4) LAB Findings in Mitochondrial Disorders are all except
1. increase in lactate and lactate: pyruvate ratio
2. Decreased Plasma carnitine
3. Normal /mildly elevated Blood CK
4. PCr/Pi ratios are higher than normal
5)Ragged red fibres are seen in
1. Mitochondrial myopathy
2. Inclusion body myositis
3. Normal ageing
4. All the above
6)Stains Used for RAGGED RED Fibres are
1. Modified Gomori trichrome
2. Succinate dehydrogenase
3. NADH-tetrazolium reductase (NADH-TR)
4. All the Above
7) Core features of MELAS are ALL Except
1. Age of symptom onset < 40 yrs
2. Encephalopathy
3. Lactic acidosis
4. Normal early Development
8) Most widely used therapeutic agent In Mitochondrial disorders is
1. Coenzyme Q10
2. L-arginine
3. Creatine
4. Levocarnitine
9) Classic features of MERRF include:
1. Myoclonus most characteristic symptom
2. Epileptic seizures
3. Ataxia
4. All the above.
10) ALL are true about Leigh,s Syndrome Except
1. Onset in 1
ST
year of life
2. Psychomotor regression
3. Mitochondrial Inheritance only.
4.In the BG, Putamen is particularly involved.
Vous aimerez peut-être aussi
- Multiple Sclerosis: Practical Comprehensive EssentialsD'EverandMultiple Sclerosis: Practical Comprehensive EssentialsPas encore d'évaluation
- Mitochondrial GeneticsDocument7 pagesMitochondrial GeneticsÖmer KhanPas encore d'évaluation
- Assignment: Department: UimltDocument10 pagesAssignment: Department: UimltEm NomanPas encore d'évaluation
- The Spectrum of Mitochondrial Disease Ep-3-10Document8 pagesThe Spectrum of Mitochondrial Disease Ep-3-10F4AR100% (1)
- Mitochondrial Inheritance (Maternal Inheritance)Document36 pagesMitochondrial Inheritance (Maternal Inheritance)Babak NamiPas encore d'évaluation
- MitochondriaDocument128 pagesMitochondriahou1212!Pas encore d'évaluation
- Mitochondrial DiseaseDocument12 pagesMitochondrial DiseaseWSETPas encore d'évaluation
- Mitochondrial Cytopathies: Ens Teaching ReviewDocument11 pagesMitochondrial Cytopathies: Ens Teaching ReviewGréta BotyánszkiPas encore d'évaluation
- Mitochondrial Disorders Overview - GeneReviews® - NCBI Bookshelf HTTPSWWW - Ncbi.nlm - nih.govbooksNBK1224Document24 pagesMitochondrial Disorders Overview - GeneReviews® - NCBI Bookshelf HTTPSWWW - Ncbi.nlm - nih.govbooksNBK1224denisaPas encore d'évaluation
- Session 3 - Mitochondrial DisordersDocument17 pagesSession 3 - Mitochondrial DisordersjoPas encore d'évaluation
- Mitochondrial Encephalomyopathies (MEM)Document66 pagesMitochondrial Encephalomyopathies (MEM)Fatma KaledPas encore d'évaluation
- Genetics 50Document2 pagesGenetics 50Ma. Joy JocosolPas encore d'évaluation
- Mitochondrial Cytopathies in Children and AdultsDocument28 pagesMitochondrial Cytopathies in Children and AdultsNathaly LapoPas encore d'évaluation
- Mitochondrial Disorders OverviewDocument21 pagesMitochondrial Disorders OverviewIt's MePas encore d'évaluation
- The Genetics and Pathology of Mitochondrial DiseaseDocument15 pagesThe Genetics and Pathology of Mitochondrial DiseaseIt's MePas encore d'évaluation
- Mitochondrial DnaDocument10 pagesMitochondrial DnaGerardo GonzalezPas encore d'évaluation
- MB2 - Mitochondrial DNADocument30 pagesMB2 - Mitochondrial DNAfaezeh zare karizakPas encore d'évaluation
- Mitochondrial GeneticsDocument2 pagesMitochondrial Geneticsmelinda garpidaPas encore d'évaluation
- Mitochondrial Disorders in Neurons 2008Document35 pagesMitochondrial Disorders in Neurons 2008Harshit PandePas encore d'évaluation
- Genetics Lab - MITOCHONDRIAL INHERITANCEDocument4 pagesGenetics Lab - MITOCHONDRIAL INHERITANCEVilllllPas encore d'évaluation
- Document 1Document20 pagesDocument 1masdfgPas encore d'évaluation
- Diagnosis and Treatment of Mitochondrial MyopathiesDocument14 pagesDiagnosis and Treatment of Mitochondrial MyopathiesUname EpithetoPas encore d'évaluation
- Mitochondrial DNA Mutations in Human DiseaseDocument9 pagesMitochondrial DNA Mutations in Human DiseaseLuna SmithPas encore d'évaluation
- MitochondriaForm, Function, Anddisease 1705678469777Document11 pagesMitochondriaForm, Function, Anddisease 1705678469777kalitutawa465Pas encore d'évaluation
- How Aging Affects Mitochondria in Brain Cells PDFDocument12 pagesHow Aging Affects Mitochondria in Brain Cells PDFRocco LamponePas encore d'évaluation
- 1 Molecular GeneticsDocument10 pages1 Molecular GeneticsAbdullah Sawalha100% (1)
- Genetic and Genomic Basis of DiseaseDocument34 pagesGenetic and Genomic Basis of DiseasesammyjaberPas encore d'évaluation
- Mitochondrial DDocument17 pagesMitochondrial DIt's MePas encore d'évaluation
- Gky 456Document28 pagesGky 456Mauro Porcel de PeraltaPas encore d'évaluation
- Outline & Study Questions: Mitochondrial DiseasesDocument4 pagesOutline & Study Questions: Mitochondrial Diseasesapi-297823098Pas encore d'évaluation
- Mitochondrial DNA and DiseaseDocument12 pagesMitochondrial DNA and Diseasepijush ghoshPas encore d'évaluation
- Presentation of Proteomics and GenomicsDocument37 pagesPresentation of Proteomics and GenomicsJunaid MughalPas encore d'évaluation
- Mitochondrial Diseases Caused by mtDNA Mutations - A Mini-ReviewDocument10 pagesMitochondrial Diseases Caused by mtDNA Mutations - A Mini-ReviewIt's MePas encore d'évaluation
- Cytogenetics Course PackDocument29 pagesCytogenetics Course Packanonymous squashPas encore d'évaluation
- Mitochondrial DisorderDocument55 pagesMitochondrial DisorderRaja DarmawanPas encore d'évaluation
- Seminar: Anthony H V SchapiraDocument10 pagesSeminar: Anthony H V Schapiramompou88Pas encore d'évaluation
- Genes MitocondriaDocument25 pagesGenes MitocondriaAbril SantiagoPas encore d'évaluation
- Mol Syst1Document3 pagesMol Syst1nheidiPas encore d'évaluation
- Review DNA MitokondriaDocument2 pagesReview DNA MitokondriaMir RimPas encore d'évaluation
- Mitochondrial ReplacementDocument33 pagesMitochondrial ReplacementAlija DzekoPas encore d'évaluation
- Mitochondrial Myopathies - Clinical Features and Diagnosis - UpToDateDocument37 pagesMitochondrial Myopathies - Clinical Features and Diagnosis - UpToDateNana ShkodinaPas encore d'évaluation
- Mitochondrial DisordersDocument16 pagesMitochondrial DisorderswlmhfpPas encore d'évaluation
- Short Study Poject: Mitochondria - Its' Structure, History and FunctionDocument5 pagesShort Study Poject: Mitochondria - Its' Structure, History and FunctionSarvPas encore d'évaluation
- Lectura Adn MitocondrialDocument13 pagesLectura Adn MitocondrialIvan Berrios VillegasPas encore d'évaluation
- Another Surprise From The Mitochondrial GenomeDocument2 pagesAnother Surprise From The Mitochondrial GenomeUSMP FN ARCHIVOSPas encore d'évaluation
- Lecture 9-GS1 1112-Mitochondria & ChloroplastDocument37 pagesLecture 9-GS1 1112-Mitochondria & ChloroplastHa LuongPas encore d'évaluation
- Mitochondrial DisorderDocument3 pagesMitochondrial DisorderRoxie May Theresse AbagatnanPas encore d'évaluation
- Mitochondria & Ageing: Extracted From The Presentation by Lee Know, NDDocument4 pagesMitochondria & Ageing: Extracted From The Presentation by Lee Know, NDDavid100% (1)
- Science Half Yearly NotesDocument14 pagesScience Half Yearly NotesanonPas encore d'évaluation
- MitocondriopatiasDocument5 pagesMitocondriopatiasomarelmoncePas encore d'évaluation
- MME Aula 2 Bruno Jesus 2023Document58 pagesMME Aula 2 Bruno Jesus 2023Brendo AlvarengaPas encore d'évaluation
- Molecular Medicine & Genetics: YuwonoDocument22 pagesMolecular Medicine & Genetics: YuwonoAhsan AuliyaPas encore d'évaluation
- Introduction To Moleculer Genetic, DNA GENOME, CELL CYCLE, APOPTOSISDocument26 pagesIntroduction To Moleculer Genetic, DNA GENOME, CELL CYCLE, APOPTOSISAji Prasetyo UtomoPas encore d'évaluation
- Mechanisms of Mitochondrial Diseases: Emil Ylikallio & Anu SuomalainenDocument19 pagesMechanisms of Mitochondrial Diseases: Emil Ylikallio & Anu SuomalainenGréta BotyánszkiPas encore d'évaluation
- Ly Mitochondrial DiseaseDocument9 pagesLy Mitochondrial DiseaseLe Phuong LyPas encore d'évaluation
- EC13 Cell Ageing DNA TextDocument8 pagesEC13 Cell Ageing DNA TextSilvito94Pas encore d'évaluation
- 5 GeneticsDocument80 pages5 Geneticspetemaravich333Pas encore d'évaluation
- Practical Approaches To A Mito Diagnosis: Richard H. Haas M.B., B.Chir., M.R.C.PDocument57 pagesPractical Approaches To A Mito Diagnosis: Richard H. Haas M.B., B.Chir., M.R.C.PlhnguPas encore d'évaluation
- Homeopathic Miasms and HeredityDocument23 pagesHomeopathic Miasms and Heredityambertje12100% (1)
- Genetika Molekuler NeoplasmaDocument23 pagesGenetika Molekuler NeoplasmaAndikaChandraPas encore d'évaluation
- Ajr 139 4 824Document1 pageAjr 139 4 824Tarun MathurPas encore d'évaluation
- Campbell Et Al. (EXTEND Trial)Document9 pagesCampbell Et Al. (EXTEND Trial)gemmalynn sarapuddinPas encore d'évaluation
- 2017 Visiting PhysicianDocument16 pages2017 Visiting PhysicianTarun MathurPas encore d'évaluation
- Campbell Et Al. (EXTEND Trial)Document9 pagesCampbell Et Al. (EXTEND Trial)gemmalynn sarapuddinPas encore d'évaluation
- ENVOY DA Guding Catheter Brochure DSUS COD 0314 0017Document4 pagesENVOY DA Guding Catheter Brochure DSUS COD 0314 0017Tarun MathurPas encore d'évaluation
- Carotid Artery Stenting: Review of Technique and Update of Recent LiteratureDocument9 pagesCarotid Artery Stenting: Review of Technique and Update of Recent LiteratureTarun MathurPas encore d'évaluation
- AtulabhcvDocument13 pagesAtulabhcvTarun MathurPas encore d'évaluation
- Envoy Family Brochure Pages Dsuscod12140219Document16 pagesEnvoy Family Brochure Pages Dsuscod12140219Tarun Mathur100% (1)
- Ajr 139 4 824Document1 pageAjr 139 4 824Tarun MathurPas encore d'évaluation
- Crit Care Nurse 2011 Traumatic Brain Injury Advanced Multimodal Neuromonitoring From Theory To Clinical PracticeDocument13 pagesCrit Care Nurse 2011 Traumatic Brain Injury Advanced Multimodal Neuromonitoring From Theory To Clinical PracticeTarun MathurPas encore d'évaluation
- New Tertiary PackagesDocument23 pagesNew Tertiary PackagesTarun MathurPas encore d'évaluation
- BMC NeurologyDocument8 pagesBMC NeurologyTarun MathurPas encore d'évaluation
- 2010 Fellowship ProgramsDocument25 pages2010 Fellowship ProgramsTarun MathurPas encore d'évaluation
- 734 FullDocument7 pages734 FullTarun MathurPas encore d'évaluation
- 44 52Document9 pages44 52Tarun MathurPas encore d'évaluation
- A Novel Microcatheter-Delivered, Highly-Flexible and Fully-Retrievable Stent, Specifically Designed For Intracranial UseDocument3 pagesA Novel Microcatheter-Delivered, Highly-Flexible and Fully-Retrievable Stent, Specifically Designed For Intracranial UseTarun MathurPas encore d'évaluation
- 2010 Fellowship ProgramsDocument25 pages2010 Fellowship ProgramsTarun MathurPas encore d'évaluation
- Ajnr A2798 Full PDFDocument7 pagesAjnr A2798 Full PDFTarun MathurPas encore d'évaluation
- EFNS Guideline 2010 Inflammatory Demyelinating PolyradiculoneuropathyDocument8 pagesEFNS Guideline 2010 Inflammatory Demyelinating PolyradiculoneuropathyDeni Andre AtmadinataPas encore d'évaluation
- Radiologic Diagnosis of Cerebral Venous Thrombosis: Pictorial ReviewDocument12 pagesRadiologic Diagnosis of Cerebral Venous Thrombosis: Pictorial ReviewTarun MathurPas encore d'évaluation
- Tentative Prgramme of Direct Rectt RPSC 2012Document2 pagesTentative Prgramme of Direct Rectt RPSC 2012IndiaresultPas encore d'évaluation
- Consent EnglishDocument1 pageConsent EnglishTarun MathurPas encore d'évaluation
- Treatment of Ocular Myasthenia Gravis: Scott R. Haines, MD Matthew J. Thurtell, MBBSDocument10 pagesTreatment of Ocular Myasthenia Gravis: Scott R. Haines, MD Matthew J. Thurtell, MBBSTarun MathurPas encore d'évaluation
- Windows Printer Test PageDocument1 pageWindows Printer Test PageTarun MathurPas encore d'évaluation
- 2animatedinteractivecerebellumconnectionsshareweb 110802184735 Phpapp02Document27 pages2animatedinteractivecerebellumconnectionsshareweb 110802184735 Phpapp02Tarun MathurPas encore d'évaluation
- The Cerebellum: Clinical ExaminationDocument70 pagesThe Cerebellum: Clinical ExaminationTarun MathurPas encore d'évaluation
- CerebellumDocument16 pagesCerebellumTarun MathurPas encore d'évaluation
- m100 Resume Portfolio AssignmentDocument1 pagem100 Resume Portfolio Assignmentapi-283396653Pas encore d'évaluation
- Current MBA GradesDocument2 pagesCurrent MBA GradesDiptarghya KunduPas encore d'évaluation
- 11v.jigisha Chaptear2Document53 pages11v.jigisha Chaptear2Anirban PalPas encore d'évaluation
- Exercise Reported SpeechDocument3 pagesExercise Reported Speechapi-241242931Pas encore d'évaluation
- Chuyen de GerundifninitiveDocument7 pagesChuyen de GerundifninitiveThao TrinhPas encore d'évaluation
- Midterm Exam (Regulatory Framework and Legal Issues in Business Law) 2021 - Prof. Gerald SuarezDocument4 pagesMidterm Exam (Regulatory Framework and Legal Issues in Business Law) 2021 - Prof. Gerald SuarezAlexandrea Bella Guillermo67% (3)
- Comprehensive Compressed Air Assessments: The 5-Step ProcessDocument8 pagesComprehensive Compressed Air Assessments: The 5-Step ProcessANDRESPas encore d'évaluation
- Chryso CI 550Document2 pagesChryso CI 550Flavio Jose MuhalePas encore d'évaluation
- 18 Ex Parte Applic Shorten Time Consolidate 11/01/21Document13 pages18 Ex Parte Applic Shorten Time Consolidate 11/01/21José DuartePas encore d'évaluation
- Christian Education of Zendeling-Based at The Kalimantan Evangelical Church (GKE)Document16 pagesChristian Education of Zendeling-Based at The Kalimantan Evangelical Church (GKE)Editor IjrssPas encore d'évaluation
- Pressure Sound MeasurementDocument47 pagesPressure Sound MeasurementSaleem HaddadPas encore d'évaluation
- Schemes and Tropes HandoutDocument6 pagesSchemes and Tropes HandoutJohn LukezicPas encore d'évaluation
- Blind Chinese SoldiersDocument2 pagesBlind Chinese SoldiersSampolPas encore d'évaluation
- Prayer For Stages On The PathDocument6 pagesPrayer For Stages On The PathEijō JoshuaPas encore d'évaluation
- Digital Signal Processing AssignmentDocument5 pagesDigital Signal Processing AssignmentM Faizan FarooqPas encore d'évaluation
- Analysis of The SPM QuestionsDocument5 pagesAnalysis of The SPM QuestionsHaslina ZakariaPas encore d'évaluation
- How To Manage Asthma: A GuideDocument44 pagesHow To Manage Asthma: A GuideSrinivas YerriboinaPas encore d'évaluation
- CabillanDocument12 pagesCabillanviviviolettePas encore d'évaluation
- JKSSB Panchayat Secretary Adfar NabiDocument3 pagesJKSSB Panchayat Secretary Adfar NabiSHEIKHXUNIPas encore d'évaluation
- Proofs in Indian Mathematics: M.D.SrinivasDocument40 pagesProofs in Indian Mathematics: M.D.SrinivasShashankPas encore d'évaluation
- Text Mapping: Reading For General InterestDocument17 pagesText Mapping: Reading For General InterestIndah Rizki RamadhaniPas encore d'évaluation
- Effect of Boron Content On Hot Ductility and Hot Cracking TIG 316L SSDocument10 pagesEffect of Boron Content On Hot Ductility and Hot Cracking TIG 316L SSafnene1Pas encore d'évaluation
- MahayanaDocument26 pagesMahayanaAleza Menorca100% (1)
- DB2 UsefullcommandDocument8 pagesDB2 Usefullcommandganeshreddy_dspxPas encore d'évaluation
- Shalini NaagarDocument2 pagesShalini NaagarAazam AdtechiesPas encore d'évaluation
- Sample DCCM, DLHTM and DCLRDocument38 pagesSample DCCM, DLHTM and DCLREagle100% (5)
- Foreign Policy During Mahathir EraDocument7 pagesForeign Policy During Mahathir EraMuhamad Efendy Jamhar0% (1)
- Developing Mental Health-Care Quality Indicators: Toward A Common FrameworkDocument6 pagesDeveloping Mental Health-Care Quality Indicators: Toward A Common FrameworkCarl FisherPas encore d'évaluation
- Communist Party of India - WikipediaDocument104 pagesCommunist Party of India - WikipediaRameshwar ChandravanshiPas encore d'évaluation
- Reading #2: Participatory Action ResearchDocument45 pagesReading #2: Participatory Action Researchapi-3723169100% (2)