Académique Documents
Professionnel Documents
Culture Documents
Script 1-21
Transféré par
KathrinaRodriguez0 évaluation0% ont trouvé ce document utile (0 vote)
27 vues40 pagesThis document discusses proper patient and clinician positioning and ergonomics. It provides guidelines for positioning patients in upright, semi-upright/semi-supine, supine, and Trendelenburg positions depending on their needs. It also discusses neutral positioning of the clinician's neck, back, torso, shoulders, arms, forearms, hands and in relation to the patient and equipment. The document emphasizes maintaining a 90 degree angle at the elbow and not compromising posture. It promotes indirect vision techniques and micro-stretching to prevent musculoskeletal disorders.
Description originale:
script
Titre original
SCRIPT 1-21
Copyright
© © All Rights Reserved
Formats disponibles
PPTX, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentThis document discusses proper patient and clinician positioning and ergonomics. It provides guidelines for positioning patients in upright, semi-upright/semi-supine, supine, and Trendelenburg positions depending on their needs. It also discusses neutral positioning of the clinician's neck, back, torso, shoulders, arms, forearms, hands and in relation to the patient and equipment. The document emphasizes maintaining a 90 degree angle at the elbow and not compromising posture. It promotes indirect vision techniques and micro-stretching to prevent musculoskeletal disorders.
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PPTX, PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
27 vues40 pagesScript 1-21
Transféré par
KathrinaRodriguezThis document discusses proper patient and clinician positioning and ergonomics. It provides guidelines for positioning patients in upright, semi-upright/semi-supine, supine, and Trendelenburg positions depending on their needs. It also discusses neutral positioning of the clinician's neck, back, torso, shoulders, arms, forearms, hands and in relation to the patient and equipment. The document emphasizes maintaining a 90 degree angle at the elbow and not compromising posture. It promotes indirect vision techniques and micro-stretching to prevent musculoskeletal disorders.
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PPTX, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 40
Back Care & Ergonomics
Patient Positioning, Clinician Positioning, Direct and Indirect
Vision, Posturedontics, Simple Stretching
Patient Positioning
Patient Positioning
Upright
initial and final
position;
at eye level when
conversing with
patient;
Semi-upright/
semi-supine
For patients w/
cardiovascular,
respiratory, or
vertigo problems
between the
upright and full
supine positions.
Supine
brain is on the
same level as the
heart.
for support of the
circulation;
used mostly for
treatment
procedures.
Trendelenburg
in the supine
position and
tipped back and
down 35 degrees
to 45 degrees
heart is higher
than the head.
emergency
position used
when the patient
is approaching
syncope
Patient Positioning
Supine Position in Detail
Body
Slightly higher than the tip of the nose
Maintains good blood flow to the head
Head
Top of head should be even with upper edge of headrest
Headrest
Should be aligned so the neck and head are aligned with the torso
Patient Positioning: Maxillary Arch
Positioning for the Maxillary Arch
BODY: feet should be even with or slightly higher
than the tip of his or her nose.
CHAIR BACK: nearly parallel to floor
HEAD: even with the upper edge of headrest
HEADREST: adjust to position the head in chin-up
position
Patient Positioning: Mandibular Arch
Positioning for the Mandibular Arch
BODY: feet should be even with or slightly higher than
the tip of his or her nose.
HEAD: even with the upper edge of headrest
CHAIR BACK: slightly raised above parallel position
(15-20 degrees)
HEADREST: slightly raise the headrest chin-down
position
Clinician Positioning
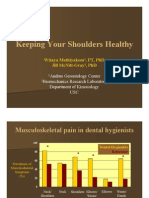
Musculoskeletal Disorders
Musculoskeletal
injuries resulting
from REPEATED
OVERUSE.
Hands, wrists
elbows, neck,
shoulders
Risk factors for MSDs (TENTATIVE)
MSDs
Fixed
working
position
Excessive
use of
small
muscles
Tight Grips
Repetitive
movements
Positioning
challenges
Confined
working
space
Equipment
limitation
Common Musculoskeletal Disorders for
Healthcare Providers
Thoracic
Outlet
Syndrome
Rotator Cuff
Tendinitis
Pronator
Syndrome
Extensor
Wad Strain
Carpal
Tunnel
Syndrome
Ulnar Nerve
Entrapment
Tenosynovitis Tendinitis
Common Musculoskeletal Disorders for
Healthcare Providers
Carpal Tunnel Syndrome
Wrist and hand disorder caused by
compression of median nerve within carpal
tunnel of the wrist.
SYMPTOMS: Numbness, pain, and tingling
in the thumb, index, and middle fingers
Prevention of MSDs
Ergonomics
Postural
and
positional
factors
PREVENTION
of MSDs
Ergonomics
Do
Maintain a neutral, balanced body
position then change patients chair and
dental equipment to complete
periodontal instrumentation.
Use neutral spine position to maintain
the natural curve of the spine
Donts
Dont change body position or
equipment in an uncomfortable or
painful manner just to get the job done.
Dont have a mindset that its acceptable
to assume an uncomfortable position
just for 15 minutes.
Neutral Positioning
Neutral Neck
Position
Neutral Back
Position
Neutral Torso
Position
Neutral
Shoulder
Position
Neutral Positioning
Neutral Upper
Arm Position
Neutral Forearm
Position
Neutral Hand
Position
Clinician and Equipment Position
Neutral Position in Relation to
Patient
Adjust the height of the clinician chair to
establish 90 degrees hip angle
Lower patient chair until tip of patients nose is
below the clinicians waist level.
Elbow angle: 90 degrees when fingers are
touching patients teeth
COMMON ERROR: patient is too high in
relation to the clinician
AVOID placing legs under the back of the
patients chair.
EASY TECHNIQUE
Sit alongside the patient while placing arms
on the sides and crossed at waist.
Patients mouth below the elbow
point.
Clinician and Equipment Position
Position for Mandibular Teeth
Dental Light place directly and as far above
patients head.
Bracket Table position as low as possible to
easily view the instruments
Patient Chair position so that elbow angle is 90
degrees when fingers rest on mandibular teeth.
Position for Maxillary Teeth
Dental Light position above patients chest. And
as far away from patients face. Tilt light so light
beams shine into patients mouth at an angle.
Patient Chair lower entire chair until elbow angle
is 90 degrees when fingers rest on maxillary teeth
Clinician and Equipment Positioning
Sequence for
Positioning
ME: Assume clock
position for the
treatment area
MY PATIENT:
Establish patient
chair and head
position
MY EQUIPMENT:
Adjust the unit
light. Pause and
self-check the
clinician, patient
and the equipment
position
MY
NONDOMINANT
HAND
MY DOMINANT
HAND:
Clock Positions for Right-handed clinician
8 oclock
9 oclock
10 oclock
12 oclock
Clock Positions for Left-handed Clinician
4 oclock
3 oclock
2 to 1 oclock
12 oclock
Positioning Summary for Left-Handed
Clinician
Positioning Summary for Right-Handed
Clinician
Exercise
1. See and check each
photo for clinician,
patient and
equipment position.
2. For incorrect
positioning element,
describe how the
problem could be
corrected.
Photo 1
Photo 2
Photo 3
Direct and Indirect Vision
Indirect Vision
Observation of reflected image in order to
visualize the lingual of mandibular posteriors,
distal of maxillary posteriors, etc. (Fehrenbach,
2009)
Definition
Reduced risk for MSDs due to minimization of
the clinician's musculoskeletal discomfort since
it allows for the maintenance of neutral position
Advantage
Simple Stretching and
Posturedontics
Simple Stretching
Increasing blood flow to muscles
Increasing production of joint synovial
fluid
maintains normal range of motion
creates a relaxation response
identifies tight muscles prone to injury
addresses the negative effects
of static, awkward postures by:
Chairside Stretching
Elbow at 90 degrees and
shoulder height. Gently
pull arm across front of
body with opposite arm.
Look over shoulder being
stretched. Hold two to four
breath cycles.
Legs in tripod position,
bend to your left side,
resting left elbow on left
knee. Stretch right arm
overhead and look at the
ceiling. Hold for two to four
breath cycles.
Clasp fingers together
behind occiput and slowly
extend the upper back.
Look toward ceiling and
press the elbows outward
to stretch the chest.
Stretching During Microbreaks
Anchor right hand
behind your back
or chair. Slowly
bring left ear
toward left armpit.
Hold two to four
breath cycles.
How to Stretch Safely
Position your body at
the starting position.
Take a deep breath
Slowly exhale as you
gradually intensify the
stretch up to a point of
mild tension or
discomfort
Hold the stretch for two
to four breathing cycles
(10 to 20 seconds)
Release the stretch
slowly come back to
neutral position. Repeat
the stretch, if time
allows.
Try on both sides and
determine which one is
the tightest.
Perform the directional
stretch primarily toward
the tightest side
throughout the workday,
Place stretching charts
that are visible from the
chairside.
Never stretch in a
painful range.
Posturedontics
Healthy spine
requires flexibility.
To achieve a healthy
spine we should
encourage
movement in all
directions.
Overusing one area
limits movement and
affects other areas
affecting blood flow
and oxygenation.
Posturedontics
Posturedontics
Daily
Functional
Exercises
A preventive strategy
for all dental personnel.
Designed to create
functional movement
patterns
Focus on muscles with
occupational demands
Encourage full range of
movements for joints
Support the natural
curves of the spine
Can be done during
clinical hours; chairside
between patients; at
home
Posturedontics
Posturedontics
Posturedontics
Posturedontics
Posturedontics
Review
Clinical Case
Scenario: A dental hygienist is on the first day of his new
position at a large dental clinic. Before taking this new
position, he was the only dental hygienist for over 10
years at the same small dental practice after graduating
top of his class at age 20. He notices that he is unable to
put his feet on the floor when he sits on the stool
provided for him. He also has trouble instrumenting the
lower arch; it just seems there is not enough overhead
light, especially on the lingual of the anteriors. He also
wants to get closer to his patients; he has forgotten what
the effective distance to a patient's mouth is. At the end
of the day he notices that his back hurts. He is worried
about what this means to his future in his profession.
1. What factors does the dental
hygienist need to consider in order
to discover why he is having a
backache?
2. What could he have done to help
with overhead lighting during
instrumentation of the mandibular
arch, especially the lingual of the
anteriors?
3. What is the distance he should have
maintained to his patient's mouths?
What can he do if this distance
seems too far away?
4. If this situation continues for many
years without any changes to his
way of practice, what could the
outcome be for him?
References
Dental Economics. (n.d.). Retrieved July 29, 2014,
from It's a S-t-r-e-t-c-h:
http://www.dentaleconomics.com/articles/print/volum
e-98/issue-5/columns/preventing-pain-in-
dentistry/it39s-a-s-t-r-e-t-c-h.html
Esther, M. W., & Charlotte, R. (2008). Clinical Practice
of Dental Hygiene. Lippincott Williams & Wilkins.
Fehrenbach, M. J., & Weiner, J. (2009). Saunders
Review of Dental Hygiene. Saunders Book
Company.
Vous aimerez peut-être aussi
- ARRANGING For Marchong or Concert BandDocument13 pagesARRANGING For Marchong or Concert BandCheGus AtilanoPas encore d'évaluation
- Patient PositioningDocument35 pagesPatient PositioningMona DoriaPas encore d'évaluation
- Mulligan Therapy: What Is It and How Does It WorkDocument33 pagesMulligan Therapy: What Is It and How Does It WorkAgus SantosoPas encore d'évaluation
- Hydrotest Test FormatDocument27 pagesHydrotest Test FormatRähûl Prätäp SïnghPas encore d'évaluation
- Revised Exam PEDocument3 pagesRevised Exam PEJohn Denver De la Cruz0% (1)
- Washington Manual Survival Guide OtolaryngologyDocument140 pagesWashington Manual Survival Guide OtolaryngologyVeronica GaticaPas encore d'évaluation
- 9 Hip MobilizationDocument12 pages9 Hip MobilizationGautamPas encore d'évaluation
- Transferring, Logrolling and PositioningDocument89 pagesTransferring, Logrolling and PositioningJay Vincent MedranoPas encore d'évaluation
- Positioning and Its ImportanceDocument22 pagesPositioning and Its ImportanceDeepika PatidarPas encore d'évaluation
- Body Mechanics: Ms. Francisca Achaliwie AND Ms. Mabel Apaanye AvaneDocument22 pagesBody Mechanics: Ms. Francisca Achaliwie AND Ms. Mabel Apaanye AvaneAmfo Baffoe FrederickPas encore d'évaluation
- Summary - Rule 116-117Document3 pagesSummary - Rule 116-117KathrinaRodriguezPas encore d'évaluation
- Shoulder Range of Motion Exercises PDFDocument4 pagesShoulder Range of Motion Exercises PDFGade JyPas encore d'évaluation
- Erap vs. Sandiganbayan GR 148560 - DigestDocument2 pagesErap vs. Sandiganbayan GR 148560 - DigestKyle Gwapo100% (4)
- Positioning AND Draping: Wilma N. Beralde, RM, RN, Man Clinical InstructorDocument47 pagesPositioning AND Draping: Wilma N. Beralde, RM, RN, Man Clinical InstructorWilma Beralde100% (1)
- Workshop Manual: 3LD 450 3LD 510 3LD 450/S 3LD 510/S 4LD 640 4LD 705 4LD 820Document33 pagesWorkshop Manual: 3LD 450 3LD 510 3LD 450/S 3LD 510/S 4LD 640 4LD 705 4LD 820Ilie Viorel75% (4)
- Positioning & Draping: Positio Ning & DrapinDocument8 pagesPositioning & Draping: Positio Ning & DrapinBiway RegalaPas encore d'évaluation
- Chair Positions ClassDocument43 pagesChair Positions ClassAmbalavanan Parthasarathy0% (1)
- Ergonomics in DentistryDocument55 pagesErgonomics in DentistryheycoolalexPas encore d'évaluation
- VRealize Operations Manager Installation and Configuration Guide For Linux and WindowsDocument98 pagesVRealize Operations Manager Installation and Configuration Guide For Linux and Windowsamdusias67Pas encore d'évaluation
- Position of PatientDocument47 pagesPosition of PatientMuhammad Al-azzizPas encore d'évaluation
- Positioning DrapingDocument35 pagesPositioning DrapingAbigail Filio Monge60% (5)
- Ergonomics and Four Handed Dentistry HandoutDocument29 pagesErgonomics and Four Handed Dentistry HandoutPierre BouvierPas encore d'évaluation
- PositioningDocument3 pagesPositioningMabesPas encore d'évaluation
- US Vs Taylor DigestDocument1 pageUS Vs Taylor DigestKathrinaRodriguezPas encore d'évaluation
- Safe Patient Handling - Sitting Up and TransferringDocument12 pagesSafe Patient Handling - Sitting Up and TransferringgrazeyjvPas encore d'évaluation
- Barrera V BarreraDocument1 pageBarrera V BarreraKathrinaRodriguezPas encore d'évaluation
- Operator Chair PositionsDocument21 pagesOperator Chair PositionsParidhi GargPas encore d'évaluation
- Preclinical and Pain ContorolDocument57 pagesPreclinical and Pain ContorolEmad AlryashiPas encore d'évaluation
- Meeting The Physiological Needs of The Clients and CaregiversDocument45 pagesMeeting The Physiological Needs of The Clients and CaregiversShafiq Mohd NorPas encore d'évaluation
- 1-Patient and Operator PositionsDocument33 pages1-Patient and Operator PositionsNs PrótesePas encore d'évaluation
- Group 1 - ErgonomicsDocument69 pagesGroup 1 - ErgonomicsFatima Nurjanna AwaliPas encore d'évaluation
- Mandatory and Other Competency in ServicesDocument235 pagesMandatory and Other Competency in ServicesRenee ConstantinoPas encore d'évaluation
- Group 41Document61 pagesGroup 41angelito cubeloPas encore d'évaluation
- Working in BalanceDocument86 pagesWorking in BalanceKathrinaRodriguezPas encore d'évaluation
- Positions 140601013927 Phpapp01Document49 pagesPositions 140601013927 Phpapp01angelito cubeloPas encore d'évaluation
- PositionDocument21 pagesPositionمحمد عبدالعالم البدويPas encore d'évaluation
- Positioningppt 220203114455Document41 pagesPositioningppt 220203114455angelito cubeloPas encore d'évaluation
- Dental Chair: Patient PositionsDocument2 pagesDental Chair: Patient PositionsBatool ZahraPas encore d'évaluation
- Mobility 1Document47 pagesMobility 1Jan LagriaPas encore d'évaluation
- Neck Exercises and AdviceDocument4 pagesNeck Exercises and AdviceShamsuddin HasnaniPas encore d'évaluation
- Position S: Pratiksha RaiDocument49 pagesPosition S: Pratiksha RaiJoanne Cristie TolopiaPas encore d'évaluation
- Collecting Objective DataDocument6 pagesCollecting Objective DataJoyce ElizaldePas encore d'évaluation
- Coordination Exercise 3Document16 pagesCoordination Exercise 3Ella CooperPas encore d'évaluation
- Comfort MeasuresDocument7 pagesComfort MeasuresMary MenuPas encore d'évaluation
- Keeping Your Shoulders HealthyDocument38 pagesKeeping Your Shoulders Healthyxyz84Pas encore d'évaluation
- Patient Positioning: Complete Guide For Nurses: Marjo S. Malabanan, R.N.,M.NDocument43 pagesPatient Positioning: Complete Guide For Nurses: Marjo S. Malabanan, R.N.,M.NMercy Anne EcatPas encore d'évaluation
- Tugas RiaDocument16 pagesTugas RiaSafitri SampulawaPas encore d'évaluation
- Bed Positioning With DiagnosisDocument149 pagesBed Positioning With DiagnosisGrace Marquez BilogPas encore d'évaluation
- Watchers' Class On Range of Motion (ROM) ExercisesDocument19 pagesWatchers' Class On Range of Motion (ROM) ExercisesMaumau Camba ZafraPas encore d'évaluation
- NCM 112 SL Prelim 2 EditedDocument34 pagesNCM 112 SL Prelim 2 EditedRy LlanesPas encore d'évaluation
- Positioning&DrapingDocument7 pagesPositioning&DrapingBiway RegalaPas encore d'évaluation
- Proper PositioningDocument13 pagesProper PositioningAbriann Vince ImpenioPas encore d'évaluation
- PositionsDocument16 pagesPositionsdenver matonPas encore d'évaluation
- Reaction PaperDocument7 pagesReaction PaperEunice FaithPas encore d'évaluation
- Psa AlgoDocument111 pagesPsa AlgoRupesh SushirPas encore d'évaluation
- Types of BedDocument42 pagesTypes of BedS AnthonyPas encore d'évaluation
- Fundamentals of Caregiving II - PrintedDocument13 pagesFundamentals of Caregiving II - Printedmoira77Pas encore d'évaluation
- COMFORT MEASURES and BODY MECHANICS MW Midterm 2016Document51 pagesCOMFORT MEASURES and BODY MECHANICS MW Midterm 2016Keesha Mae Urgelles TimogPas encore d'évaluation
- Body Mechanics and Patient CareDocument79 pagesBody Mechanics and Patient CareChristian DioPas encore d'évaluation
- Positioning OkDocument23 pagesPositioning OkDencel BarramedaPas encore d'évaluation
- Prelim-Wk-4 ActivityDocument4 pagesPrelim-Wk-4 ActivityKimberly Wyne SantosPas encore d'évaluation
- Coordinative Physiotherapy For Patients With Ataxia: Frequently Asked Questions About..Document4 pagesCoordinative Physiotherapy For Patients With Ataxia: Frequently Asked Questions About..johnsonkk125Pas encore d'évaluation
- Assignment IN Health Assessment: Brgy.96, Calanipawan Road, Tacloban City, 6500Document7 pagesAssignment IN Health Assessment: Brgy.96, Calanipawan Road, Tacloban City, 6500Marimiel PagulayanPas encore d'évaluation
- Spine Conditioning ProgramDocument7 pagesSpine Conditioning Programmaimunabegam766Pas encore d'évaluation
- 2017-Rehab Spine PDFDocument7 pages2017-Rehab Spine PDFPerpetua KamikadzePas encore d'évaluation
- Musculoskeletal SystemDocument160 pagesMusculoskeletal SystemAirene Aquino BusaniaPas encore d'évaluation
- ACHQC Abdominal Core Surgery Rehabilitation Protocol Patient Guide 6.17.20Document43 pagesACHQC Abdominal Core Surgery Rehabilitation Protocol Patient Guide 6.17.20Brka223Pas encore d'évaluation
- Tips for Everyday Life and Sports With an Artificial Joint: Expert guidebook for dealing with a prosthesis for patients with a new hip or knee jointD'EverandTips for Everyday Life and Sports With an Artificial Joint: Expert guidebook for dealing with a prosthesis for patients with a new hip or knee jointPas encore d'évaluation
- Financial Accounting - NotesDocument28 pagesFinancial Accounting - NotesKathrinaRodriguezPas encore d'évaluation
- Lesson - December 16Document8 pagesLesson - December 16KathrinaRodriguezPas encore d'évaluation
- Annual ReportDocument44 pagesAnnual ReportKathrinaRodriguezPas encore d'évaluation
- Case 4 Krispy Kreme - OutlineDocument5 pagesCase 4 Krispy Kreme - OutlineKathrinaRodriguezPas encore d'évaluation
- 2 Cases ConstiDocument17 pages2 Cases ConstiKathrinaRodriguezPas encore d'évaluation
- Case Digest Part 2Document4 pagesCase Digest Part 2KathrinaRodriguezPas encore d'évaluation
- Case DigestDocument4 pagesCase DigestKathrinaRodriguezPas encore d'évaluation
- Case Digest Part 2Document4 pagesCase Digest Part 2KathrinaRodriguezPas encore d'évaluation
- LalaDocument25 pagesLalaKathrinaRodriguezPas encore d'évaluation
- Works Cited: Concise Review: Adult Salivary Gland Stem Cells and A Potential Therapy For XerostomiaDocument1 pageWorks Cited: Concise Review: Adult Salivary Gland Stem Cells and A Potential Therapy For XerostomiaKathrinaRodriguezPas encore d'évaluation
- Working in BalanceDocument86 pagesWorking in BalanceKathrinaRodriguezPas encore d'évaluation
- Oral Health Care For People With Mental Health Problems Guidelines and RecommendationsDocument21 pagesOral Health Care For People With Mental Health Problems Guidelines and RecommendationsKathrinaRodriguezPas encore d'évaluation
- J Dent Res 90 (3) :371-376, 2011Document3 pagesJ Dent Res 90 (3) :371-376, 2011KathrinaRodriguezPas encore d'évaluation
- Developmental Ages at LEH DevelopmentDocument11 pagesDevelopmental Ages at LEH DevelopmentKathrinaRodriguezPas encore d'évaluation
- Patient Positioning, Operator Positioning, Direct and Indirect Vision Simple Stretching and PosturedonticsDocument12 pagesPatient Positioning, Operator Positioning, Direct and Indirect Vision Simple Stretching and PosturedonticsKathrinaRodriguezPas encore d'évaluation
- Placement Report EditedDocument2 pagesPlacement Report EditedKathrinaRodriguezPas encore d'évaluation
- Presentation 1Document5 pagesPresentation 1KathrinaRodriguezPas encore d'évaluation
- GRADE 302: Element Content (%)Document3 pagesGRADE 302: Element Content (%)Shashank Saxena100% (1)
- Btech CertificatesDocument6 pagesBtech CertificatesSuresh VadlamudiPas encore d'évaluation
- Dial 1298 For Ambulance - HSBCDocument22 pagesDial 1298 For Ambulance - HSBCDial1298forAmbulancePas encore d'évaluation
- P&CDocument18 pagesP&Cmailrgn2176Pas encore d'évaluation
- Heart Attack Detection ReportDocument67 pagesHeart Attack Detection ReportAkhil TejaPas encore d'évaluation
- Bridging The Divide Between Saas and Enterprise Datacenters: An Oracle White Paper Feb 2010Document18 pagesBridging The Divide Between Saas and Enterprise Datacenters: An Oracle White Paper Feb 2010Danno NPas encore d'évaluation
- Assignment OSDocument11 pagesAssignment OSJunaidArshadPas encore d'évaluation
- Ethernet: Outline Multiple Access and Ethernet Intro Ethernet Framing CSMA/CD Protocol Exponential BackoffDocument25 pagesEthernet: Outline Multiple Access and Ethernet Intro Ethernet Framing CSMA/CD Protocol Exponential BackoffcheckPas encore d'évaluation
- Abbott 2021 ApJL 915 L5Document24 pagesAbbott 2021 ApJL 915 L5Manju SanthakumariPas encore d'évaluation
- Pep 2Document54 pagesPep 2vasubandi8Pas encore d'évaluation
- Reaffirmed 1998Document13 pagesReaffirmed 1998builconsPas encore d'évaluation
- KKS Equipment Matrik No PM Description PM StartDocument3 pagesKKS Equipment Matrik No PM Description PM StartGHAZY TUBePas encore d'évaluation
- Zanussi Parts & Accessories - Search Results3 - 91189203300Document4 pagesZanussi Parts & Accessories - Search Results3 - 91189203300Melissa WilliamsPas encore d'évaluation
- EVS (Yuva)Document88 pagesEVS (Yuva)dasbaldev73Pas encore d'évaluation
- Splash25 Winner InstructionsDocument8 pagesSplash25 Winner InstructionsRamkrishna PaulPas encore d'évaluation
- 2017 Hu Spence Why Globalization Stalled and How To Restart ItDocument11 pages2017 Hu Spence Why Globalization Stalled and How To Restart Itmilan_ig81Pas encore d'évaluation
- Def - Pemf Chronic Low Back PainDocument17 pagesDef - Pemf Chronic Low Back PainFisaudePas encore d'évaluation
- Prevention of Power Theft Using Concept of Multifunction Meter and PLCDocument6 pagesPrevention of Power Theft Using Concept of Multifunction Meter and PLCMuhammad FarhanPas encore d'évaluation
- ReflectionDocument3 pagesReflectionapi-174391216Pas encore d'évaluation
- Chapter5A TorqueDocument32 pagesChapter5A TorqueShuq Faqat al-FansuriPas encore d'évaluation
- Good Manufacturing Practices in Postharvest and Minimal Processing of Fruits and VegetablesDocument40 pagesGood Manufacturing Practices in Postharvest and Minimal Processing of Fruits and Vegetablesmaya janiPas encore d'évaluation
- CV - Mohsin FormatDocument2 pagesCV - Mohsin FormatMuhammad Junaid IqbalPas encore d'évaluation
- DCNF Vs Hhs Nov 2020Document302 pagesDCNF Vs Hhs Nov 2020SY LodhiPas encore d'évaluation
- Dental Clinic - Floor Plan R3-2Document1 pageDental Clinic - Floor Plan R3-2kanagarajodisha100% (1)
- PresentationDocument6 pagesPresentationVruchali ThakarePas encore d'évaluation