Académique Documents
Professionnel Documents
Culture Documents
Alterations in Oxygenation
Transféré par
Melchor Felipe Salvosa100%(1)100% ont trouvé ce document utile (1 vote)
2K vues104 pagesNCM 103 Lecture
Copyright
© © All Rights Reserved
Formats disponibles
PPT, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentNCM 103 Lecture
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PPT, PDF, TXT ou lisez en ligne sur Scribd
100%(1)100% ont trouvé ce document utile (1 vote)
2K vues104 pagesAlterations in Oxygenation
Transféré par
Melchor Felipe SalvosaNCM 103 Lecture
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PPT, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 104
Review of Anatomy and
Physiology of the Respiratory
System
Upper Respiratory Tract
-consists of nose, sinuses, nasal passages,
pharynx, tonsils, adenoids, larynx and trachea.
Nose- composed of an internal and external
portion
external portion- protrudes from the face
supported by the nasal bones and cartilages
anterior nares- external openings of the nasal
cavities
Review of Anatomy and
Physiology of the Respiratory
System
Paranasal sinuses- include four pairs of
bony cavitites.
-connected by a series of ducts that drain
into the nasal cavity
named by their location: frontal,
ethmoidal,
sphenoidal, and maxillary
- fxn: resonating chambers in speech
- common site of infection
Review of Anatomy and
Physiology of the Respiratory
System
Turbinates(Bones)- also called conchae
-increase the surface area of the mucous
membrane in the nasal passages
- As air enters the nostrils, it comes in
contact with the mucous membrane to
trap all the dust and microorganisms; air
is moistened and warmed to body
temperature
Review of Anatomy and
Physiology of the Respiratory
System
Internal portion- hollow cavity separated
into right and left nasal cavities by the
nasal septum
Each nasal cavity divided into 3
passageways by the projection of the
turbinates(conchae) from the lateral walls
-lined with highly vascular ciliated
mucous membranes caleed the nasal
mucosa
Review of Anatomy and
Physiology of the Respiratory
System
Pharynx- tubelike structure that connects
the nasal and oral cavities to the larynx
3 regions:
nasopharynx- posterior to the nose and
above the soft palate
oropharynx- houses the palatine tonsils
laryngopharynx- extends from the hyoid
bone to the cricoid cartilage
Epiglottis- forms the entrance to the
larynx
Review of Anatomy and
Physiology of the Respiratory
System
Larynx- cartilaginous, epithelium lined structure that connects the
pharynx and the trachea
- major function: vocalization
-consists of the following:
*Epiglottis- flap of cartilage that covers the opening to the
larynx during swallowing
*Glottis- the opening between the vocal cords in the larynx
*Thyroid cartilage- the largest of the cartilage structures; part
of it forms the Adams apple
*Cricoid cartilage- the only complete cartilaginous ring in the
larynx(located below the Thyroid cartilage)
*Arytenoid cartilages- used in vocal cord movement with the
Thyroid cartilage
*Vocal cords- ligaments controlled by muscular movements
that produce sounds; located in the lumen of the larynx
Review of Anatomy and
Physiology of the Respiratory
System
Trachea- a.k.a. windpipe
composed of smooth muscle with C-shaped
rings of cartilage at regular intervals
The cartilaginous rings are incomplete on
the posterior surface and give firmness to
the wall of the trachea to prevent it from
collapsing
Serves as passage between the larynx and
the bronchi
Review of Anatomy and
Physiology of the Respiratory
System
Lungs- paired elastic structures enclosed in the
thoracic cage(airtight chamber with distensible
walls)
Ventilation- requires movement of the thoracic
cage and diaphragm(Floor)
Inspiration- air enters because of the negative
pressure in the thoracic cage
Expiration- air is forced out during lung recoil
Passive process requiring little energy
COPD- expiration requires energy
Review of Anatomy and
Physiology of the Respiratory
System
Pleura- serous membrane lining the
lungs(Visceral pleura) and the wall of the
thorax(parietal pleura)
-small amount of pleural fluid between
the two membranes serve to lubricate the
thorax and the lungs to permit smooth
motion of the lungs within the thoracic
cavity with each breath
Pleural friction rub-
Review of Anatomy and Physiology
of the Respiratory System
Mediastinum- middle of the thorax between the
pleural sacs that contain the two lungs
-extends from the sternum to the vertebral
column and contains all the thoracic tissue
outside the lungs.
Lobes
-left lobe- consists of an upper and lower lobe
-right lobe- consists of an upper, middle, and
lower lobe
*Each lobe further subdivided into two to five
segments separated by fissures
Review of Anatomy and Physiology
of the Respiratory System
Bronchi and bronchioles
-lobar bronchi- 3 in the right and 2 in the left
Lobar bronchi divide into:
Segmental bronchi- 10 on the right and 8 on the left
-structures identified when choosing the the most effective postural
drainage position for a given patient.
Segmental bronchi divide into:
Subsegmental bronchi- surrounded by by connective tissue that contains
arteries, lymphatics, and nerves
Subsegmental bronchi then divide into:
Bronchioles- no cartilage in their walls
-patency depends on the elastic recoil of the surrounding smooth
muscle and on the alveolar pressure
*The bronchi and bronchioles are lined with cells that have cilia(propels
mucus and foreign substances away from the lungstowards the larynx
Review of Anatomy and
Physiology of the Respiratory
System
Alveoli- the lung is made of 300 million alveoli arranged
in clusters of 15 to 20
=70 sq. meters(tennis court)
3 Types of alveolar cells
Type1- epithelial cells that form the alveolar walls
Type2- metabolically active(secrete surfactant which is
a phospholipid that lines the inner surface to prevent
alveolar collapse
Type3- large phagocytic cells that ingest foreign
matter( bacteria, mucus)
- acts a defense mechanism
Review of Anatomy and Physiology
of the Respiratory System
Functions of Respiration
Oxygen transport- capillary-cell
exchange
Respiration- capillary-alveoli exchange
Ventilation-
inspiration from the trachea to the
alveoli
expiration- alveolar gas travels in
reverse
Review of Anatomy and Physiology
of the Respiratory System
Air Pressure Variances-
Inspiration
1.movement of the diaphragm and
thoracic cavity
2. enlarges the thoracic cavity
3. lowers the pressure inside the thorax
to a level below atmospheric pressure
4. air is drawn into the alveoli
Review of Anatomy and Physiology
of the Respiratory System
Air pressure Variances
Expiration
1. The diaphragm relaxes and the lungs recoil
2. Decrease in the size of the thoracic cavity
3. Alveolar pressure exceeds atmospheric pressure
4. Air flows from the lungs into the atmosphere
Airway Resistance
determined by the radius or size of the airway
through which the air is flowing
Eg. Changes in bronchial diameter- affects airway
resistance and alters the rate of air flow
Eg. Bronchial asthma
Review of Anatomy and Physiology
of the Respiratory System
Causes of Increased airway Resistance:
*contraction of bronchial smooth muscle-
asthma
*obstruction of the airway- mucus, tumor or
foreign body
*loss of lung elasticity- emphysema,
characterized by connective tissue
encircling the airways, keeping them
open during inspiration and expiration
Review of Anatomy and Physiology
of the Respiratory System
Compliance- measure of the elasticity,
expandability and distensibility of the
lungs
Volume-pressure relationship in the lungs
High compliance- overdistended lungs
Low or decreased- stiff lungs
eg. Pnemothorax, hemothorax, pleural
effusion, pulmonary edema, pulmonary
fibrosis, ARDS
Tidal Volume
-VT or TV
- the volume of air inhaled and ehaled
with each breath
-normal value: 500 ml
- Significance : the tidal volume may not
vary even with severe disease
Inspiratory Reserve Volume
-IRV
- the maximum volume of air that can be
inhaled after a normal inspiration
-normal value: 3000 ml
Expiratory reserve Volume
ERV
The maximum volume of air that can be
exhaled forcibly after a normal exhalation
Normal value: 1100 ml.
Decreased with restrictive conditions such
as obesity, ascites, pregnancy
Residual Volume
RV
The volume of air remaining in the lungs
after a maximum exhalation
Normal value: 1200 ml
Increased with obstructive disease
Vital Capacity
VC
The maximum volume of air exhaled from
the point of maximum inspiration
VC= TV+IRV+ERV
Normal value: 4600 ml.
Decreased VC may be found in
neuromuscular disease, generalized fatigue,
atelectasis, pulmonary edema, and COPD
Inspiratory Capacity
IC
Maximum volume of air inhaled after normal
expiration
IC=TV+IRV
Normal value: 3500 ml.
Decreased IC in restrictive disease
Functional Residual Capacity
FRC
Volume of air remaining in the lungs after a
normal expiration
FRV= ERV+RV
Normal value: 2300 ml.
May be increased with COPD
And decreased in ARDS
Total Lung capacity
TLC
The volume of air in the lungs after a
maximum inspiration
Normal value: 5800 ml.
May be decreased with restrictive disease
ie. Atelectasis, pneumonia
Increased in COPD
Diffusion- process by which oxygen and
carbon dioxide are exchanged at the air-
blood interface(alveolar- capillary
membrane)
Pulmonary perfusion- actual blood flow to
the pulmonary circulation
Ventilation- actual flow of gas in and out
of the lungs
Perfusion- filling of the pulmonary
capillaries with blood
Adequate gas exchange depends on an
adequate ventilation-perfusion ratio(V/Q)
Imbalance occurs as a result of
inadequate perfusion, inadequate
ventilation or both
Four possible V/Q states
Normal ratio
-healthy lung
-equal amount of blood passes an alveolus
matched by an equal amount of gas
- ratio is 1:1
-ventilation matches perfusion
Four possible V/Q states
Low ventilaton- perfusion ratio
-also called shunt producing disorders
-perfusion exceeds ventilation, a shunt exists
-blood bypasses the alveoli but without gas
exchange occuring
- seen in distal airway obstruction ie. Pneumothorax,
atelectasis, tumor, mucus plug
Four possible V/Q states
High Ventilation-perfusion ratio (Dead
Space)
Ventilation exceeds perfusion
Alveoli do not have adequate blood supply
for gas exchange to occur
Pulmonary emboli, pulmonary infarction,
cardiogenic, shock.
Four possible V/Q states
Silent unit
Absence or limited ventilation and perfusion
Seen in pneumothorax, severe ARDS
Health History- focuses on the physical and functional aspects of
the patient and the effects of these problems on the patient,
including activities of daily living.
Reason the patient is seeking health care often related to
DYSPNEA, HEMOPTYSIS
Dyspnea- difficult or labored breathing is a common symptom in
pulmonary and cardiac patients
May be associated in neuromuscular disorders ie. Myasthenia gravis,
Guillain-Barre syndrome, muscular dystrophy
May also occur after physical exercise in people without disease.
Common at the end of life.
Acute diseases of the lungs produce a more severe grade of dyspnea
Sudden dyspnea in a healthy person- pneumothorax, acute
respiratory obstruction, or ARDS
Sudden dyspnea in immobilized patients- pulmonary embolism
May occur with other disorders: cardiac disease, anaphylactic
reactions, severe anemia.
Orthopnea- inability to breath easily
except in the upright position
May be found in patients with heart disease
or COPD
How much exertion triggers shortness of breath
Cough?
Is dyspnea related to other symptoms?
Was the onset sudden or gradual
At what time of the day or night does SOB occur
Worse when flat in bed
Does it occur at rest? Exercise? Running? Climbing
stairs?
Is the SOB worse while walking? If so, when walking
how far? How fast
Relief measures: identify and correct cause, rest and
high Fowlers position, Oxygen
Cough- reflex that protects the lungs from
the accumulation of secretions or the
inhalation of foreign bodies
Results from the irritation of the mucous
membrane anywhere in the resp. tract
Symptom of a disorder
Causes: airborne irritant, infection, cardiac
disease, medications(ACE inhibitors),
smoking, GERD(gastro-esophageal reflux
disease)
Sputum production- reaction of the lungs to
any constantly recurring irritant
May also be associated with nasal discharge.
Bacterial infection- profuse, thick yellow, green or
rusty colored sputum
Viral bronchitis- thin, mucoid sputum
Chronic bronchitis- gradual increase of sputum over
time
Lung abscess- foul smelling sputum
Relief measures: hydration, aerosolized solutions
Chest Pain- in pulmonary conditions, pain is
sharp, stabbing, intermittent, dull, aching or
persistent
May occur with pneumonia, pulmonary embolism,
lung infarction
Wheezing- may be heard with or without a
stethoscope.
High pitched, musical sound heard mainly on
expiration
Bronchodilators( oral or inhalants)
Clubbing of the fingers- sign of lung
disease in patients with chronic hypoxic
conditions
Initially manifested as sponginess of the nail
bed and loss of nail bed angle.
Hemoptysis- expectoration of blood from
the respiratory tract
May be sudden, intermittent or continuous
Most common causes: pulmonary infection,
carcinoma, pulmonary artery or vein
abnormalities, pulmonary embolus and
infarction, abnormalities of the heart and
blood vessels.
Cyanosis- bluish coloring of the skin
Assessmnet of cyanosis is affected by room
lighting, skin color, and distance of the blood
vessels from from the surface of the skin
Eupnea- normal breathing at 12-18 breaths
/minute
Bradypnea- slower than normal(<10
breaths/min) with normal depth and regular
rhythm
Tachypnea- rapid,shallow breathing >24
breaths/min
Hypoventilation- shallow,irregular breathing
Hyperventilation-increased rate and depth of
breathing( Kussmauls respiration if caused by
diabetic ketoacidosis)
Apnea- period of cessation of breathing.Time
duration varies
-may occur with other breathing disorders
ie. Sleep apnea
Cheyne- Stokes- regular cycle where the rate
and depth of breathing increase, then decrease
until apnea.
Biots Respiration- periods of normal
breathing(3-4 breaths) followed by a varying
period of apnea( usually 10-60 seconds)
Tactile Fremitus- detection of vibration on the chest wall by touch
-sound generated by the larynx travels distally along the
bronchial tree to set the chest wall in resonant motion.
Factors affecting fremitus:
1. thickness of the chest wall
2. obesity with increased subcutaneous tissue
*lower pitched sounds travel better through the normal lung and
produce greater vibration on the chest wall
*more pronounced in men than in women because of deeper male
voice
*most palpable in the upper thorax anteriorly and posteriorly
*patient is asked to repeat ninety nine, one-two-three, or eee,
eee, or tres-tres.
Air does not conduct sound well
Solid substances such as tissue conduct
sound well
Emphysema patients- decreased tactile
fremitus
Pneumonia with lung consolidation-
increased fremitus
Determines whether the underlying
tissues are filled with air, fluid or solid
material
Estimate the size and location of certain
structures within the thorax( eg.
Diaphragm, heart and liver)
Flatness----- Eg. Large pleural effusion
location example: thigh
Dullnes------Eg. Lobar pneumonia
location example: liver
Resonance-----eg. Simple chronic bronchitis
location example: normal lung
Hyperresonance--- Eg. Emphysema, pneumothorax
location example: none
Tympany----- eg. Large pneumothorax
location example: gastric air bubble; puffed out
cheek
Vesicular- inspiratory sounds lasts longer than expiratory sounds
location- entire lung field over the upper sternum and
between the scapula
Bronchovesicular- inspiratory nd expiratory sounds are about
equal
location: 1
st
and 2
nd
interspacesanteriorly and between the
scapula( over the main bronchus)
Bronchial- expiratory sounds lasts longer the inspiratory sounds
location: over the manubrium
Tracheal- inspiratory and expiratory sounds are about equal
location: over the trachea in the neck
Crackles in general- discontinuous popping sounds that occur during
inspiration
etiol: fluid in the airways or alveoli or to opening of collapsed alveoli.
coarse crackles- discontinuous popping sounds heard in early inspiration;
harsh moist sounds originating in the large bronchi
etiol: obstructive pulmonary disease
Fine crackles- discontinuos poppping sounds heard in late inspiration; like
hair rubbing together; originates in the alveoli
etiol: instertitial pneumonia, restrictive pulmonary disease(fibrosis),
bronchitis, pneumonia
Wheezes
sonorous wheezes(rhonchi)- deep low pitched rumbling sonds heard
primarily during expiration;caused by air moving through narrowed
tracheobronchial passages
etiol: secretions or tumor
Wheezes
sibilant wheezes- continuous, musical, high pitched, whistle
like sounds heard during inspiration and expiration
etiol: air passing through narrowed or partially obstructed
airways
eg. Bronchospasm, asthma
Friction rubs
Pleural friction rubs- harsh crackling sound, like 2 pieces of leather
rubbing together
-heard during inspiration alone or during inspiration and
expiration
-may subside when patient holds breath. Coughing will not
clear sound
etiol: inflammation or loss of lubricating pleural fluid
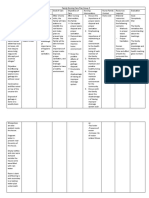
Assessment Findings in Common
Respiratory Disorders
Disorder Tactile fremitus Percussion Auscultation
Consolidation eg
pneumonia
Increased Dull Bronchial breath
sounds
Bronchitis Normal Resonant Normal to dec
breath sounds,
wheezes
Emphysema Normal to
decreased
Resonant to
hyperresonant
Dec. intensity of
breath sounds,
usually with
prolonged
expiration
Asthma Normal to
decreased
Resonant to
hyperresonant
Wheezes
Assessment Findings in Common
Respiratory Disorders
Disorder Tactile
fremitus
Percussion Auscultation
Pulmonary
edema
Normal Resonant Crackles at lung
bases,possibly
wheezes
Pleural effusion Absent Dull to flat Decreased to
absent breath
sounds
Pnemothorax Decreased Hyperresonant Absent breath
sounds
Atelectasis Absent Flat Decreased to
absent breath
sounds
Diagnostic Studies
Pulmonary function tests(PFTs)
-routinely used in patients with chronic
respiratory disorders
-assesses respiratory function and
determines the extent of destruction
-monitors the course of the patient with
an established respiratory disease and
assesses response to therapy
Pulmonary Function Tests(PFTs)
Forced Vital capacity
-FVC
-reduced in COPD because of air trapping
-performed with a maximally forced expiratory
effort
Forced Expiratory volume
-FEV1
-volume of air expired in the specified time
during the performance of forced vital capacity;
FEV1 is volume exhaled in 1 second
-clue to the severity of airway obstruction
Arterial Blood Gas Studies
Measurement of the blood pH and arterial oxygen and
CO2 tensions
Blood obtained from arterial punctures
Nsg. Responsibility: !!!!! Adequate hemostasis
PaO2- indicates the degree of oxygenation of blood
PaCO2- indicates the adequacy of alveolar ventilation
Aid in assessing the ability of the lungs to provide
adequate oxygen and remove CO2 and the ability of
the kidneys to reabsorb or excrete bicarbonate ions to
maintain normal body pH
Serial ABGs- explain to the patient the procedure
Arterial Blood Gas Studies
Normal ABG values
pH- 7.35- 7.45
PaCO2- 35 -45 mm Hg
PaO2- 80- 100 mm Hg
HCO3- 22-26 meq/L
Pulse oximeter
Non invasive method of continuously monitoring the
oxygen saturation of hemoglobin(SaO2)
Referred to as spO2 when oxygen saturation is
measured by pulse oximetry
Effective tool for monitoring for subtle or sudden
changes in oxygen saturation.
Probe may be attached to:
finger tip, ear lobe, bridge of the nose, forehead
Normal spO2- 95-100%?
Factors that affect SpO2 Vales
dyes, vasoconstrictor medications, cardiac arrest
and shock
Cultures
Cultures from the throat or nose- useful in
identifying organisms responsible for causing
the disease
Sputum Studies
Obtained for analysis to identify the pathogenic
organisms and to determine whether malignant
cells are present.
May also be used for hypersensitivity states to
guide treatment.
Expectoration is the usual method of collection
Sputum Studies
Other methods of collecting sputum
1.Endotracheal aspiration
2. bronchoscopic removal
3. transtracheal aspiration
Nsg responsibility: 1. specimen should be
delivered to the lab within 2 hours of
collection
Imaging Studies
Chest x-ray
normal pulmonary tissue- radiolucent
Routine chest x-ray- 2 views
PA view; lateral projection
usually taken with a full inspiration
X-ray: shows major contrasts between
body densities such as bone, soft
tissues, and air
Imaging Studies
Computed Tomography
-imaging method where the lungs are
scanned in successive layers by a
narrow beam x-ray
-provides a cross sectional view of the
chest
- may use contrast agents
Nsg Responsibility:
allergy to iodine or seafoods
BUN/Creatinine levels
Imaging Studies
Magnetic Resonance Imaging (MRI)
-similar to CT scan except magnetic
fields and radiofrequency are used
instead of a narrow beam x-ray
-yields more detailed images than a
CT.
Imaging Studies
Pulmonary Angiography
- commonly used to investigate
thromboembolic diseases of the lungs.
eg. Pulmonary embolism,congenital
abnormalities of the pulmonary vascular tree
Procedure: rapid injection of a radiopaque
agent into the vasculature of the lungs for
radiographic study of the pulmonary vessels
Endoscopic Procedures
Bronchoscopy- direct inspection and
examination of the larynx, trachea, and
bronchi through a flexible fiberoptic
bronchoscope
Purposes: Diagnostic
1. determine the location and extent of the
pathologic process
2. examine tissues or collect secretions
3. determine whether a tumor can be resected
surgically
4. obtain tissue sample for diagnosis
5. diagnose bleeding sites
Endoscopic Procedures
Bronchoscopy
Purposes: Therapeutic
1. remove foreign bodies from the tracheobronchial tree
2. remove secretions when the patient cannot clear them
3. treat post op atelectasis
4. destroy and excise lesions
Complications of Bronchoscopy
1. reaction to local anesthetic
2. infection
3. aspiration
4. bronchospasm
5. hypoxemia
6. pnemothorax
7. bleeding
8. perforation
Endoscopic Procedures
Bronchoscopy-
Nursing Interventions
1. consent
2. withhold food and fluids 6 hours
3. Preop meds- atropine- vagal
stimulation and bradycardia
opioids-
4. remove dentures
5. post op- nothing by mouth until cough
reflex returns, then ice chips---fluids
Imaging Studies
Thoracentesis
-accumulation of pleural fluid may occur with
some disorders of which a sample of this fluid
can be obtained thoracentesis
- aspiration of pleural fluid for diagnostic or
therapeutic purposes
-may be ultrasound guided- less complications
-Studies include: Gram staining, C/S, acid fast
staining and culture, differential cell count,
cytology, pH, sp. Gravity, total protein, and
lactic dehydrogenase
Thoracentesis
Nursing Activities
Ascertain in advance- chest x-ray has been ordered
Assess for allergy to the local anesthetic
Administer sedation if prescribed
Inform the patient:
1. remain immobile
2. pressure sensations expected
3. minimal discomfort after the procedure
Position: Upright- facilitates removal of fluid that
localizes at the base of the thorax
*sitting on the edge of the bed with the feet
supported and arms and head on a padded over the
bed table.
Imaging Studies
Biopsy- excision of a small amount of tissue for
examination of cells
Pleural Biopsy
-accomplished by needle biopsy of the pleura or
pleuroscopy(visual explorationthrough a
fiberoptic bronchoscope inserted into the
pleural space.
-performed when there is pleural exudateof
undetermined origin or when there is a need to
stain or culture the tissue to identify
tuberculosis or fungi.
Pulmonoray Angiography
Used to investigate thromboembolic
disease of the lungs eg. Pulmonary
embolism, congenital abnormalities of the
pulmonary system
Procedure- rapid injection of a
radiopaque substance into a vein while
simultaneously doing a radiographic
study (CT Scan).
Upper Airway Infections
Rhinitis- inflammation and irritation of the
mucous membranes of the nose
-acute, chronic, non allergic, allergic
-Allergic rhinitis- may be classified as
seasonal (pollen seasons)
Perennial(occurs throughout the year)
Pathopyhysiology: environmental factors
changes in temp., odors, food, drugs
such as cocaine and antihypertensive
meds., infection.
Rhinitis
Management
1. H and P
- ask for possible exposure to allergens
- swollen and congested nasal mucosa
Meds: decongestants/paracetamol
corticosteroids
desensitizing immunizations
antibiotics
antihistamines
saline sprays
Viral Rhinitis/common cold: rhinorrhea, nasal congestion, sneezing,
headache, muscle pains
- highly contagious
Cause: rhinovirus
other causes: adenovirus, Coronavirus, RSV, influenza
virus
***Each virus has many strains---vacccine is impossible
Acute Sinusitis
Inflammation of the mucous membranes of the paranasal sinuses
Often follows URIobstruction of the nasal cavities--- bacterial
growth
Most often caused by bacteria (60%)
Other causes: abnormal structures of the nose, diving and
swimming, trauma
S/Sx: facial pain
fatigue
purulent nasal discharge
fever, headache
ear pain
nasal obstruction
sense of fullness
decrease sense of smell
sore throat
snoring
periorbital edema
Acute Sinusitis
Assessment
1.tenderness to palpation of the sinus
area
2. tenderness on tapping of the sinus
area
3. transillumination with light-
decrease transmission
Complications: meningitis, abscess,
osteomyelitis,
Meds: same as in rhinitis
Acute Sinusitis
Nsg. Management
1. Steam inhalation
2. Warm compresses
3. Avoid- swimming, diving, air travel
4. Nasal decongestant- rebound congestion
5. Follow recommended antibiotic regimen
6. Advise for signs of complications: nuchal
rigidity, severe headache, fever
Chronic Sinusitis
Symptoms of sinusitis lasting more than
3 months
Pathopysiology: same as in Acute
sinusitis
S/sx: same as in acute
Medical mgt: same as in acute
*surgery to correct to correct structural
deformities eg. Excising nasal polyps,
correcting deviated nasal septum
Acute Pharyngitis
Sudden inflammation of the pharynx
Sore throat- primary symptom
Causes: bacterial and viral(self limiting)
Complications:
1. sinusitis
2. otitis media
3. peritonsillar abscess
4. pneumonia
5. meningitis
6. rheumatic fever (Group A B-hemolytic
Streptococcus)
8. nephritis
S/Sx: swollen pharyngeal membrane and
tonsils(exudate), lymphadenopathy
Chronic Sinusitis
Persistent inflammation
Causes:
-Common in adults, over use of voice,
alcohol, tobacco
S/Sx: soreness /fulness of the throat
dysphagia
postnasal drip
Management:
antibiotics, antihistamines, decongestants
Tonsillitis/Adenoiditis
Acute tonsillitis- can be confused with
pharyngitis
Group A Beta hemolytic Sreptococcus- most
common organism
S/sx: fever, sore throat, snoring, mouth
breathing, earache,
May spread to the middle ears via Eustachian
tubes otitis media
Management: increased fluid intake, salt water
gargles, pain mends, PCN,
Surgery: tonsillectomy/ adenoidectomy for
repeated episodes
Tonsillitis/Adenoiditis
Post op care in tonsillectomy
1. immediate post op care- patient in prone
position with head turned to the side
2. ice collar to the neck
3. frequent swallowing- warrants investigation-
may suggest hemorrhage
4. Vital signs- increasing heart rate (^Temp or
decreasing BP)
5. check for swallowing reflex- ice chips
6. Advise: refrain from too much talking
7. control coughing
Peritonsillar abscess
Collection of purulent exudate between the
tonsillar capsule and the surrounding tissues
Common cause : Beta hemolytic streptococcus
Edema can cause airway obstruction-life
threatening
S/Sx: fever, trismus, drooling, odynophagia
swelling of the soft palate, unilateral
tonsillar hypertrophy
Med Management: antibiotics(PCN)- effective
-fine needle aspiration of the of pus or
incision and drainage
Laryngitis
Result from voice abuse, dust, chemicals,
smoke, or as part of URI, allergies
S/Sx: hoarseness
aphonia
severe cough
Management: voice rest, antibiotics and
steroids, dysphagia, hemoptysis
Obstruction and Trauma of the
Upper Respiratory Airway
Sleep Apnea
1. excessive daytime sleepiness
2. frequent nocturnal awakening
3. insomnia
4. loud snoring
5. morning headaches
6. intellectual deterioration
7. irritabilty
8. impotence
9. dysrhythmias
10. severe hypertension
11. pulmonary hypertension
12. polycythemia
13. enuresis
Sleep Apnea
Managementt
1.avoid sleeping on the back
2.avoid alcohol and meds that depress the
upper airway
3. weight loss
4. CPAP or biPAP(bilevel positive airway
pressure)
5. surgery- uvulopalatopharyngoplasty
6. Meds: Protryptiline increases the
respiratory drive
Medroxyprogesterone ?
Acetazolamide(Diamox) ?
Vous aimerez peut-être aussi
- Beauty Pageant QuestionsDocument14 pagesBeauty Pageant QuestionsMelchor Felipe Salvosa70% (10)
- A. Nursing Process in The Care of Population, Groups, and CommunityDocument6 pagesA. Nursing Process in The Care of Population, Groups, and Communityanne marie50% (2)
- Theories, Frameworks, and ModelsDocument34 pagesTheories, Frameworks, and Modelsgctv049182% (11)
- PALS Study Guide Short FormDocument11 pagesPALS Study Guide Short FormLenTheRN88% (8)
- Nursing Informatics TheoriesDocument11 pagesNursing Informatics TheoriesFilamae Jayahr Caday60% (5)
- NCM 110 Lec Nursing Informatics Technology Part 1Document5 pagesNCM 110 Lec Nursing Informatics Technology Part 1Krizle Adaza0% (1)
- Family Nursing Care Plan - Inadequate Living SpaceDocument1 pageFamily Nursing Care Plan - Inadequate Living SpaceMushy_ayaPas encore d'évaluation
- Lec 1 105Document70 pagesLec 1 105Melchor Felipe SalvosaPas encore d'évaluation
- Interprofessional Care in The CommunityDocument18 pagesInterprofessional Care in The CommunityCreciabullecer100% (1)
- I. Framework For Maternal and Child Health Nursing (MCN) Focusing On At-Risk, High Risk, and Sick ClientsDocument5 pagesI. Framework For Maternal and Child Health Nursing (MCN) Focusing On At-Risk, High Risk, and Sick ClientsSophia Loraine Dorone Jesura100% (1)
- Typology of Nursing Problems in Family Health CareDocument7 pagesTypology of Nursing Problems in Family Health CareJunathan L. DelgadoPas encore d'évaluation
- Micro OBSDocument10 pagesMicro OBSMelchor Felipe SalvosaPas encore d'évaluation
- Family Health Nursing ProcessDocument37 pagesFamily Health Nursing ProcessNeethu Vincent100% (3)
- Unit Iv: Application in Evidence - Based Nursing PracticeDocument43 pagesUnit Iv: Application in Evidence - Based Nursing PracticeRaquel MonsalvePas encore d'évaluation
- Chapter 7 - Lecture Outline Nursing Care of Clients Having SurgeryDocument8 pagesChapter 7 - Lecture Outline Nursing Care of Clients Having SurgeryMelchor Felipe SalvosaPas encore d'évaluation
- Chn-New Technologies Related To Public Health Electronic Information-ReportDocument7 pagesChn-New Technologies Related To Public Health Electronic Information-ReportAmadea WP100% (2)
- CHNDocument18 pagesCHNRamaida TalibPas encore d'évaluation
- Community Health Nursing 1 Chapter 1Document42 pagesCommunity Health Nursing 1 Chapter 1Lawrence Ryan Daug100% (2)
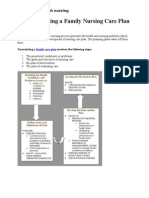
- Steps in Making A Family Nursing Care PlanDocument4 pagesSteps in Making A Family Nursing Care PlanMary LouPas encore d'évaluation
- NCM 100 Lecture NotesDocument9 pagesNCM 100 Lecture NotesanreilegardePas encore d'évaluation
- 4th Stage of LabourDocument57 pages4th Stage of LabourBlessy Solomon91% (11)
- What Happens in The Operating RoomDocument137 pagesWhat Happens in The Operating RoomMelchor Felipe Salvosa100% (1)
- Nursing Informatics 1-2Document15 pagesNursing Informatics 1-2Jenny Agustin Fabros100% (1)
- Trends in Maternal and Child CareDocument24 pagesTrends in Maternal and Child CareJose Richard Giray100% (1)
- NCM 112 Lecture Module 4 Cellular AberrationDocument16 pagesNCM 112 Lecture Module 4 Cellular AberrationMeryville JacildoPas encore d'évaluation
- Bag Technique ChecklistDocument3 pagesBag Technique Checklistpppamm100% (9)
- The ACM v2.0 International PDFDocument76 pagesThe ACM v2.0 International PDFTiago SilvaPas encore d'évaluation
- Immediate Newborn Care Definition 23Document6 pagesImmediate Newborn Care Definition 23Courtney Dela FierraPas encore d'évaluation
- N104 01 Alteration in Perception and CoordinationDocument75 pagesN104 01 Alteration in Perception and CoordinationMax Loco100% (2)
- Fundamentals of NursingDocument220 pagesFundamentals of NursingdgratyPas encore d'évaluation
- Nursing Care of A Family When A Child Has A Cardiovascular DisorderDocument9 pagesNursing Care of A Family When A Child Has A Cardiovascular DisorderMarianne Gail100% (1)
- Health As A Multifactorial PhenomenonDocument2 pagesHealth As A Multifactorial PhenomenonJan Jamison Zulueta100% (9)
- Impaired Gas ExchangeDocument2 pagesImpaired Gas ExchangeHanya Bint PotawanPas encore d'évaluation
- Rle NCM 107 - Maternal & Child Nursing 1 (Well Clients)Document4 pagesRle NCM 107 - Maternal & Child Nursing 1 (Well Clients)ChelleyOllitro100% (4)
- Fundamentals of NursingDocument3 pagesFundamentals of NursingMelvin Aurelio100% (1)
- CHNN211 Week 2 Health Care Delivery SystemDocument7 pagesCHNN211 Week 2 Health Care Delivery SystemABEGAIL BALLORANPas encore d'évaluation
- Family Nursing Care Plan Group 5Document2 pagesFamily Nursing Care Plan Group 5Aireen100% (1)
- Policies, Guidelines and Laws in Nursing Informatics: Unit IvDocument77 pagesPolicies, Guidelines and Laws in Nursing Informatics: Unit IvCybill Diaz100% (1)
- Unit 1 - Over ViewDocument28 pagesUnit 1 - Over ViewRaquel MonsalvePas encore d'évaluation
- Electrocardiogram Return Demonstration ScriptDocument3 pagesElectrocardiogram Return Demonstration ScriptRio Dante100% (1)
- Cellular AberrationsDocument94 pagesCellular AberrationsKatherineCentenoIlaganRNPas encore d'évaluation
- Home Visit and Bag TechniqueDocument34 pagesHome Visit and Bag TechniqueEdralyn MatalangPas encore d'évaluation
- Care of The Mother and The Fetus During Perinatal PeriodDocument11 pagesCare of The Mother and The Fetus During Perinatal PeriodMaria KawilanPas encore d'évaluation
- Care of Mother, Child, Adolescent (Autosaved)Document23 pagesCare of Mother, Child, Adolescent (Autosaved)Shing Mae Marie100% (10)
- Group 9 - Roles of Community Health Nurse in EhealthDocument11 pagesGroup 9 - Roles of Community Health Nurse in EhealthCharlene RepolloPas encore d'évaluation
- APA FormatDocument47 pagesAPA FormatMelchor Felipe SalvosaPas encore d'évaluation
- Nursing Informatics Models &theoriesDocument30 pagesNursing Informatics Models &theoriesmagdaashaabanPas encore d'évaluation
- Ethical Issues Related To Technology in The Delivery of Health CareDocument19 pagesEthical Issues Related To Technology in The Delivery of Health CareKaye Viola100% (1)
- Lesson 8. Policies, Laws and Guidelines in Nursing InformaticsDocument9 pagesLesson 8. Policies, Laws and Guidelines in Nursing InformaticsGroup 8 BSN 33Pas encore d'évaluation
- Care of Mother Child, Adolescent (Well Clients)Document2 pagesCare of Mother Child, Adolescent (Well Clients)Shheeeeeshh100% (1)
- Care - of - Mother - Child - and - Adolescent 2Document48 pagesCare - of - Mother - Child - and - Adolescent 2Jmarie Brillantes PopiocoPas encore d'évaluation
- UNIT 2 Concepts Principles and Theories in Nursing InformaticsDocument12 pagesUNIT 2 Concepts Principles and Theories in Nursing InformaticsGabbi KimPas encore d'évaluation
- UNIT 3 - Information Technology System Applicable in Nursing PracticeDocument85 pagesUNIT 3 - Information Technology System Applicable in Nursing PracticeRaquel MonsalvePas encore d'évaluation
- Information Technology System Applicable in Nursing Practice Notes 1Document7 pagesInformation Technology System Applicable in Nursing Practice Notes 1Stephanie Lee100% (2)
- Professional Adjustment and Nursing JurisprudenceDocument38 pagesProfessional Adjustment and Nursing JurisprudenceCandy Garcia Aceveda ReyesPas encore d'évaluation
- Nursing Care of Children With Alterations in HealthDocument44 pagesNursing Care of Children With Alterations in HealthAmy Del Carmen50% (2)
- Community Health Nursing by Maglaya PDFDocument2 pagesCommunity Health Nursing by Maglaya PDFNicole Marie MartusPas encore d'évaluation
- FCP (Gorres)Document3 pagesFCP (Gorres)Kaloy KamaoPas encore d'évaluation
- Nursing Diagnosis Nursing Intervention Rationale Breathing PatternDocument7 pagesNursing Diagnosis Nursing Intervention Rationale Breathing PatternJinaan MahmudPas encore d'évaluation
- Family Nursing Care Plan - Cough and ColdsDocument1 pageFamily Nursing Care Plan - Cough and ColdsArnx QuilonPas encore d'évaluation
- CHN-RLE Module 2 (Home Visits)Document5 pagesCHN-RLE Module 2 (Home Visits)Ems Rio Bal100% (1)
- The Nursing Diagnosis Body Image Disturbance Is Most Likely To Be Written For Which of The Following PersonsDocument3 pagesThe Nursing Diagnosis Body Image Disturbance Is Most Likely To Be Written For Which of The Following PersonsenzoPas encore d'évaluation
- Competency Standards of Nursing Practice in The PhilippinesDocument5 pagesCompetency Standards of Nursing Practice in The Philippinespamcarl100% (2)
- Crisostomo Soapie ChartingDocument2 pagesCrisostomo Soapie ChartingMica OmotsosircPas encore d'évaluation
- Case Study 2: A Matter of Freedom: AnswerDocument1 pageCase Study 2: A Matter of Freedom: AnswerApple Mae ToñacaoPas encore d'évaluation
- CHN 1 Module 1Document10 pagesCHN 1 Module 1Dianne LabisPas encore d'évaluation
- Enc Return DemoDocument3 pagesEnc Return DemoJoyce MadarangPas encore d'évaluation
- Checklist For Newborn: Cavite State UniversityDocument2 pagesChecklist For Newborn: Cavite State UniversityChloe MorningstarPas encore d'évaluation
- 16 Respiratory SystemDocument40 pages16 Respiratory SystemchromaPas encore d'évaluation
- PAin and Oxygenation HandoutsPRELIMSDocument7 pagesPAin and Oxygenation HandoutsPRELIMSJhoanna de ChavezPas encore d'évaluation
- The Respiratory System: ASTIKA NUR ROHMAH, S.Kep., NS., M.BiomedDocument43 pagesThe Respiratory System: ASTIKA NUR ROHMAH, S.Kep., NS., M.BiomedAdek KhazeliaPas encore d'évaluation
- Tracer Study of SPC GRADUATES 2015-2016Document18 pagesTracer Study of SPC GRADUATES 2015-2016Melchor Felipe Salvosa100% (1)
- Phil HX and Consti OBEDocument10 pagesPhil HX and Consti OBEMelchor Felipe SalvosaPas encore d'évaluation
- Chapter 4 - Lecture Outline: Joyce Hammer 1/23/2018Document5 pagesChapter 4 - Lecture Outline: Joyce Hammer 1/23/2018Melchor Felipe SalvosaPas encore d'évaluation
- Con Mission, Vision, ObjectivesDocument1 pageCon Mission, Vision, ObjectivesMelchor Felipe SalvosaPas encore d'évaluation
- Tracer Study SPC GRADUATES 2015 and 2016Document6 pagesTracer Study SPC GRADUATES 2015 and 2016Melchor Felipe SalvosaPas encore d'évaluation
- OBE Syllabus HA Summer 2014Document16 pagesOBE Syllabus HA Summer 2014Melchor Felipe SalvosaPas encore d'évaluation
- Elective 2 Lecture 1 Concept of IllnessDocument9 pagesElective 2 Lecture 1 Concept of IllnessMelchor Felipe Salvosa100% (1)
- NCM 106 Resource UnitDocument15 pagesNCM 106 Resource UnitMelchor Felipe SalvosaPas encore d'évaluation
- Care of Mother, Child, Family and Population Group At-Risk or With ProblemsDocument52 pagesCare of Mother, Child, Family and Population Group At-Risk or With ProblemsMelchor Felipe Salvosa100% (1)
- Homeostasis, Stress, and AdaptationDocument16 pagesHomeostasis, Stress, and AdaptationMelchor Felipe SalvosaPas encore d'évaluation
- Enrichment of The Outcomes-Based Education (Obe) Syllabus CON-School of Midwifery AY 2013-2014 First SemesterDocument6 pagesEnrichment of The Outcomes-Based Education (Obe) Syllabus CON-School of Midwifery AY 2013-2014 First SemesterMelchor Felipe SalvosaPas encore d'évaluation
- Concept of Health and IllnessDocument29 pagesConcept of Health and IllnessMelchor Felipe SalvosaPas encore d'évaluation
- Pain Lecture 2Document23 pagesPain Lecture 2Melchor Felipe SalvosaPas encore d'évaluation
- NCM 102 LectureDocument165 pagesNCM 102 LectureMelchor Felipe SalvosaPas encore d'évaluation
- CSDocument6 pagesCSMelchor Felipe SalvosaPas encore d'évaluation
- Endocrine DisordersDocument12 pagesEndocrine DisordersMelchor Felipe SalvosaPas encore d'évaluation
- Respiratory ModalitiesDocument61 pagesRespiratory ModalitiesMelchor Felipe Salvosa100% (1)
- Spiritual Care NursingDocument34 pagesSpiritual Care NursingMelchor Felipe SalvosaPas encore d'évaluation
- San Pablo Colleges College of Nursing San Pablo City: Dr. Anita R. Rico 2011Document1 pageSan Pablo Colleges College of Nursing San Pablo City: Dr. Anita R. Rico 2011Melchor Felipe SalvosaPas encore d'évaluation
- Livelihood Documentation School of NursingDocument28 pagesLivelihood Documentation School of NursingMelchor Felipe SalvosaPas encore d'évaluation
- Evaluation Tool RubricDocument9 pagesEvaluation Tool RubricMelchor Felipe SalvosaPas encore d'évaluation
- Outcomes Based SyllabusDocument15 pagesOutcomes Based SyllabusMelchor Felipe SalvosaPas encore d'évaluation
- Vital Signs Monitoring SheetDocument2 pagesVital Signs Monitoring SheetMelchor Felipe SalvosaPas encore d'évaluation
- Angelica M.docx LFD 4Document2 pagesAngelica M.docx LFD 4Angelica Malacay RevilPas encore d'évaluation
- Types of CPRDocument12 pagesTypes of CPRSaid OmaryPas encore d'évaluation
- Ventilation Servo-I Universal: Data SheetDocument20 pagesVentilation Servo-I Universal: Data SheetBreno VieiraPas encore d'évaluation
- Safety Data Sheet: TeppekiDocument12 pagesSafety Data Sheet: TeppekiSloPas encore d'évaluation
- Imaging Request: Diagnostic ProcedureDocument4 pagesImaging Request: Diagnostic ProcedureMarielle ChuaPas encore d'évaluation
- Asphyxialconditions 120917062150 Phpapp02Document93 pagesAsphyxialconditions 120917062150 Phpapp02minaaminmaPas encore d'évaluation
- Heights of Summerlin Statement of DeficienciesDocument26 pagesHeights of Summerlin Statement of DeficienciesLas Vegas Review-JournalPas encore d'évaluation
- Sss AssigmentDocument11 pagesSss Assigmentindran SuppiahPas encore d'évaluation
- Msds-Incense SticksDocument5 pagesMsds-Incense SticksFlavioPas encore d'évaluation
- ADVIA Chemistry Lithium 2 LITH 2 United Kingdom DXDCM 09017fe98079651c-1671061174537Document20 pagesADVIA Chemistry Lithium 2 LITH 2 United Kingdom DXDCM 09017fe98079651c-1671061174537EFS SalesPas encore d'évaluation
- 2022 American Society of Anesthesiologists Practice GuidelinesDocument7 pages2022 American Society of Anesthesiologists Practice GuidelinesIrving Alexis Pérez DuquePas encore d'évaluation
- CPRDocument41 pagesCPRPreethi BPas encore d'évaluation
- Conservative and Surgical Modalities in The Management of Pediatric Parapneumonic Effusion and EmpyemaDocument14 pagesConservative and Surgical Modalities in The Management of Pediatric Parapneumonic Effusion and EmpyemaPamela JumpPas encore d'évaluation
- Streptokinase Versus Unfractionated Heparin Nebu in ARDS RCT 2020Document8 pagesStreptokinase Versus Unfractionated Heparin Nebu in ARDS RCT 2020Fransisca Dewi KumalaPas encore d'évaluation
- Cardiopulmonary Exercise Testing (CPET)Document2 pagesCardiopulmonary Exercise Testing (CPET)frandi wirajayaPas encore d'évaluation
- Centurion Lead Acid Battery, Wet, Non Spillable Sds 01898 03042018Document7 pagesCenturion Lead Acid Battery, Wet, Non Spillable Sds 01898 03042018Munya BengezaPas encore d'évaluation
- Surfactant TherapyDocument11 pagesSurfactant TherapyDiksha DuhanPas encore d'évaluation
- Asthma Action Plan For Children PDF DownloadDocument2 pagesAsthma Action Plan For Children PDF DownloadAlejandro MalagáPas encore d'évaluation
- Script Wat So EverDocument14 pagesScript Wat So EverJastine SabornidoPas encore d'évaluation
- PneumococcalDocument13 pagesPneumococcalRahul JaganPas encore d'évaluation
- Pneumothorax+Case+Study+ 1Document2 pagesPneumothorax+Case+Study+ 1Anonymous iOpPt7sIoPas encore d'évaluation
- Komparasi Lyra X1Document1 pageKomparasi Lyra X1Ikhsan FakhurroziPas encore d'évaluation
- Mechanical VentilationDocument86 pagesMechanical Ventilationremjith rajendranPas encore d'évaluation
- PICAREDocument2 pagesPICAREagus susantoPas encore d'évaluation
- Nursing Careplan Inadequate Tissue PerfusionDocument2 pagesNursing Careplan Inadequate Tissue PerfusionAudrey LewisPas encore d'évaluation