Académique Documents
Professionnel Documents
Culture Documents
Renal Vascular Diseases
Transféré par
johny3333Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Renal Vascular Diseases
Transféré par
johny3333Droits d'auteur :
Formats disponibles
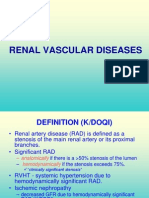
RENAL VASCULAR DISEASES
2
DEFINITION (K/DOQI)
Renal artery disease (RAD) is defined as a
stenosis of the main renal artery or its proximal
branches.
Significant RAD
anatomically if there is a >50% stenosis of the lumen
hemodynamically if the stenosis exceeds 75%.
clinically significant stenosis
RVHT - systemic hypertension due to
hemodynamically significant RAD.
Ischemic nephropathy
decreased GFR due to hemodynamically significant
RAD (K/DOQI)
impairment of renal function beyond occlusive disease
of the main renal arteries (Textor).
3
SIGNIFICANCE
The prevalence and incidence of chronic kidney
disease (CKD) are increasing.
ESRD incidente patients rates are 168 in Canada,
1 250 in the USA and 85.7 in Romania.
It is of importance to search for reversible causes
of CKD.
Renal artery stenosis (RAS) may account for 5
22% of patients with ESRD who are older than 50
years;
Correction of ischemic lesions can reverse
decrease in renal function and improve CV
outcomes.
4
PREVALENCE
RAS due to:
Atherosclerotic renovascular disease (ARVD >90%)
Fibromuscular disease (FMD).
Takayashus arteritis up to 60% (Indian subcontinent
and the Far East)
autopsy studies
- 450% of subjects, (16.4 vs. 5.5% > 60 vs < 60 years)
aortic angiography
- 38% of patients with aortic aneurysm,
- 33% in those with aortic occlusive disease
- 39% lower limb occlusive disease.
cardiac catheterization
- 1429% prevalence in coronary disease
- < 10% in normal coronary arteries .
5
PATHOGENY (1)
ARVD is associated with three major clinical
syndromes:
ischemic renal disease
hypertension.
Renal failure (acute and chronic)
6
PATHOGENY (2)
Interrelation among Renal-Artery Stenosis, Hypertension, and Chronic Renal Failure
Robert D. Safian, M.D., and Stephen C. Textor, M.D NEJM, Nr 6, vol 344:431-442,
2001
7
RAS AND KIDNEY FUNCTION (1)
27% of those with RAS develop chronic renal failure within 6 years.
Nephrol Dial Transplant (2007) 22: 10021006; Atherosclerotic renovascular
disease: beyond the renal artery stenosis; Pascal Meier, Jerome Rossert,
Pierre-Francois Plouin ,Michel Burnier
8
ISCHAEMIC NEPHROPATHY (1)
Interstitial fibrosis,
tubular atrophy,
glomerulosclerosis (including focal segmental
glomerulosclerosis),
periglomerular fibrosis
arteriolar abnormalities (hialinosclerosis,
atheroembolism).
atherosclerotic nephropathy
9
ISCHAEMIC NEPHROPATHY (2)
Histologic studies of interstitial fibrosis (Trichrome stain, left two (a) low magnification and high magnification (b) and
immunohistochemistry for NF-kappa-B (NFkB, right) in swine. The presence of renal artery stenosis (RAS) induces both
interstitial fibrosis and NFkB), which is accelerated by the presence of high cholesterol levels (HC). (Chade AR,
Rodriguez-Porcel M, Grande JP, Krier JD, Lerman A, Romero JC, Napoli C, Lerman LO: Distinct renal injury in early
atherosclerosis and renovascular disease. Circulation 106: 11651171, 2002)
10
ISCHAEMIC NEPHROPATHY (3)
Acute renal failure
bilateral renal arterial occlusion (RAO)
intra-renal cholesterol atheroembolization
damage from radiocontrast agents during intra-
arterial angiography
hypovolaemia, often with concurrent diuretic use
concurrent use of angiotensin-converting enzyme
inhibitors (ACE-I) or angiotensin II receptor blockers
(AII-RBs).
11
ARVD AND ITS ASSOCIATION WITH
HEART AND OTHER VASCULAR
DISEASES (1)
Coronary artery disease
RAS is associated with more severe and
extensive coronary artery disease
? effects of renal ischemia or is a marker
for advanced atherosclerosis and
cardiovascular risk?
12
ARVD AND ITS ASSOCIATION WITH
HEART AND OTHER VASCULAR
DISEASES (2)
Cardiac dysfunction including flash pulmonary oedema
presenting clinical syndrome in 41% of patients with
bilateral ARAS and in 12% of patients with unilateral ARAS.
angiotensin II promoted sodium retention and increase in
pulmonary microcirculation permeability
ARVD patients were found to have significantly higher
prevalence
left ventricular hypertrophy (78.5% compared with
46.0%)
left ventricular diastolic dysfunction (40.5% compared
with 12.0%),
greater left ventricular mass index (183 74 g/m2
compared with 116 33 g/m2).
13
ARVD AND ITS ASSOCIATION WITH
HEART AND OTHER VASCULAR
DISEASES (3)
Aortic aneurysm and peripheral vascular disease
Prevalence of ARVD in patients undergoing aortography
for intermittent claudication varying from 33%, 39%,
44.9%;
Cerebrovascular disease
The coexistence of ARVD in patients who have stroke
and/or carotid stenoses In an autopsy series of 346
cases of brain infarcts >75% RAS was found in 10.4%
of subjects and carotid artery stenosis in 33.6%.
Patients with carotid stenosis were more likely to have
ARVD than those without carotid disease.
Conversely, ARVD patients are more likely to have
carotid disease.
14
ARVD AND ITS ASSOCIATION WITH
HEART AND OTHER VASCULAR
DISEASES (4)
ARVD and hypertension
ARVD is found in 25% of all cases of hypertension
90% of patients with ARVD are hypertensive.
hypertension precedes ARVD development in many
cases.
15
DIAGNOSIS OF ARVD (1)
Clinical features suggestive of renovascular disease
Hypertension
Abrupt onset of hypertension in patients aged <30 years (suggestive of
FMD) or >50 years (suggestive of ARVD)
Absent family history of hypertension
Accelerated or malignant hypertension
Resistance to therapy (3 drugs)
Hypertension may be absent, particularly in patients with chronic
cardiac disfunction.
Renal abnormalities
Unexplained renal failure in patients aged >50 years
Elevation in plasma creatinine level after the initiation of ACE-I or AII-RB
therapy (> 30% increase in serum creatinine)
Asymmetrical kidneys on imaging
16
DIAGNOSIS OF ARVD (2)
Other
Unexplained acute pulmonary oedema or
congestive cardiac failure
Femoral, renal, aortic or carotid bruits
Severe retinopathy
History of extra-renal vascular disease
Hypokalaemia
Neurofibromatosis
17
DIAGNOSIS OF ARVD (3)
DRASTIC
The most powerful predictors for detecting lesions of
at least 50%:
age,
symptomatic vascular disease,
elevated cholesterol
the presence of an abdominal bruit.
18
DIAGNOSIS OF ARVD (4)
Investigation of ARVD
Duplex ultrasonography
widely available, noninvasive, and
inexpensive.
First line screening test
sensitivity of 85% and specificity of 92%.
peak systolic velocity, has the highest
performance characteristics;
19
DIAGNOSIS OF ARVD (6)
Magnetic resonance imaging
the favoured imaging method for the proximal renal vasculature
The sensitivity ranges from 83% to 100% and specificity from 92% to
97%.
Gadolinium is non-nephrotoxic at low doses;
MR renal angiogram showing tight stenosis of the right renal artery and occlusion of the left
renal artery
20
DIAGNOSIS OF ARVD (7)
Computed tomography angiography
Sensitivity and specificity of 95%
Best for aortorenal calcification (utility in stent
placement);
Visualise main and accesory renal arteries.
Limitations
risk of contrast nephropathy
poor visualization of the distal main renal
artery and segmental branches.
21
DIAGNOSIS OF ARVD (8)
Renal scintigraphy and measurement of individual
kidney function
the captopril test unravel the degree of renin activation
Asymmetric result of a functional test RAS
Sensitivity and specificity variable: 43% - 93%
Insufficient sensitivity in:
Renal failure;
Renin independent hypertension
22
DIAGNOSIS OF ARVD (9)
Renal Arteriography
the gold standard diagnostic test.
risks of contrast nephropathy and
atheroembolic renal disease
23
TREATMENT OPTIONS IN ARVD (1)
Few topics provoke more controversy between
nephrologists and interventional cardiologists
than management of atherosclerotic renovascular
disease
24
TREATMENT OPTIONS IN ARVD (2)
Medical treatment
Limiting the progression of atheromatous disease
and chronic kidney disease
vigorous control of hypertension and hyperlipidemia,
diabetes control
use of antiplatelet agents,
cessation of smoking
lifestyle modification (including reduced dietary intake
of salt and increased exercise).
attention to the complications of renal insufficiency
25
TREATMENT OPTIONS IN ARVD (3)
CORAL study (Cardiovascular Outcomes in Renal Atherosclerotic
Lesions)
26
TREATMENT OPTIONS IN ARVD (4)
Antihypertensive therapy
Is there an ideal blood pressure target that confers
maximal cardiovascular protection?
In CORAL, the target blood pressure is 140/ 90 mm
Hg ; 130/80 mm Hg is recommended for patients
with hypertension and diabetes or renal disease.
Is there a specific antihypertensive regimen that
provides cardiovascular benefits beyond just lowering
blood pressure?
27
TREATMENT OPTIONS IN ARVD (5)
First-line agent
Angiotensin receptor antagonist
First-line agent if ARB not tolerated - ACE inhibitor
especially for those
with proteinuric chronic parenchymal disease,
and those with coexisting coronary artery disease and
cardiac dysfunction.
Second-line agent
Thiazide diuretic
Combinations with ARB/ACE may be available
Use loop diuretics for patients with serum creatinine 2 mg/dL
Third-line agents (function of comorbidities)
Calcium channel blocker
Beta Blocker
Alfa Blocker
Vasodilator
28
TREATMENT OPTIONS IN ARVD (6)
Dyslipidemia Treatment
in terms of cardiovascular risk RAS is considered a
coronary artery disease equivalent. Third Report of the
Expert Panel on Detection, Evaluation, and Treatment of High Blood
Cholesterol in Adults (Adult Treatment Panel III)
Goal of therapy
low-density lipoprotein cholesterol <100 mg/dL
some suggesting a target of < 70 mg/dL
Statins
effects independent of lipid-lowering
stabilize, slow progression or even induce regression of
atherosclerotic plaque
reduction of proteinuria
29
TREATMENT OPTIONS IN ARVD (7)
Diabetes Mellitus
HbA1c of <7 mg/dL with oral agents and/or insulin
medical nutrition therapy;
physical activity;
multidisciplinary foot and eye care;
Chronic Renal Insufficiency
Tight control of blood pressure, dyslipidemia, diabetes;
manage anemia; hyperparathyroidism. (Guidelines)
Antiplatelet Agents
Although there are no direct data in patients with RAS,
administration of an antiplatelet agent is required in
CORAL and recommended for all patients with RAS.
Aspirin, Clopidogrel or Ticlopidin.
30
TREATMENT OPTIONS IN ARVD (8)
Effect of the Medical Therapy Intervention
reduce cardiovascular risk
progression to end-stage renal disease actually
does not respond very well to medical therapy
31
TREATMENT OPTIONS IN ARVD (9)
Surgical treatment
revascularization
nephrectomy of small kidneys with relatively complete
arterial occlusion.
32
TREATMENT OPTIONS IN ARVD (9)
Evidence for renal revascularization
Randomized Trials in Renal Artery Stenosis Intervention
Year n Medical Balloon Stent End Points
Weibull 1993 58 X X BP/renal function
Plouin 1998 49 X X BP
Webster 1998 55 X X BP/renal function
van de Ven 1999 84 X X Patency/BP/renal function
van Jaarsveld 2000 106 X X BP/renal function
Benefits:
A modest improvement in blood pressure control
no improvement in renal function.
33
TREATMENT OPTIONS IN ARVD (10)
Definite indications for renal revascularization
Recurrent flash pulmonary oedema
Severe hypertension resistant to all medical therapy.
When a patient who requires ACE-I or AII-RB
therapy (e.g. for cardiac failure) presents with
significant ACE-I-related uraemia.
RAO in a reasonably sized kidney
34
TREATMENT OPTIONS IN ARVD (11)
CONTROVERSIES
Effect of Revascularization on Blood Pressure
Revascularization may fail to cure hypertension
In long-standing hypertension, secondary processes
that sustain hypertension
Vascular remodeling,
atherosclerosis,
ischemic damage to the poststenotic kidney,
hypertensive injury to the nonstenotic kidney
35
PROGNOSIS OF PATIENTS WITH
ARVD (1)
Major mortality from cardiovascular
complications; risk of death is almost six
times that of developing ESRD
36
NEPHROSCLEROSIS
37
Definition
clinical syndrome characterized by long-
term essential hypertension, hypertensive
retinopathy, left ventricular hypertrophy,
minimal proteinuria, and progressive renal
insufficiency
38
Pathophysiology
glomerular ischemia:chronic hypertension
result in narrowing of preglomerular
arteries and arterioles, with a consequent
reduction in glomerular blood flow
Glomerulosclerosis induce by glomerular
hypertension and glomerular hyperfiltration
39
Genetics
a significant loss in kidney function was
observed in black people despite similar
levels of BP control
polymorphism in the angiotensin-
converting enzyme (ACE) gene, the DD
genotype
increased angiotensinogen mutations
40
Frequency
USA: 1985-2005, adjusted rates of ESRD
caused by hypertension increased 140%
Hypertensive nephrosclerosis accounts for
more than one third of patients on
hemodialysis.
Europe: 12% of new patients starting renal
replacement therapy
41
Race
In black people, hypertensive
nephrosclerosis occurs earlier, is more
severe, and more often causes ESRD
(36.8% in black patients vs 26% in white
patients).
42
Age
The diagnosis of hypertensive
nephrosclerosis increases with advancing
age.
The peak age for the development of
ESRD in white patients is 65 years and
older, while the peak age is 45-65 years in
black people
43
DIAGNOSIS
Long-standing or very severe hypertension
Black race
Hypertension preceding renal dysfunction
Hypertension diagnosed prior to the onset of
proteinuria
No evidence of another renal disease
Biopsy findings compatible with the diagnosis
Proteinuria less than 0.5 g/d
Hypertensive retinal changes
Left ventricular hypertrophy
44
Lab Studies
(I)
Baseline complete blood cell count
Creatinine level
Electrolyte status
Urinalysis
Either a spot urine test for albumin or
creatinine ratio or a 24-hour urine
collection - To determine total protein
excretion
45
Lab Studies
(II)
urine protein excretion of lower than 1 g/d;
in some patients a 24-hour urinary protein
excretion greater than 1 g/d has been
described.
When secondary changes of focal
segmental glomerulosclerosis (FSGS)
related to hyperfiltration develop,
proteinuria can increase to the nephrotic
range.
46
Imaging Studies
echocardiogram to assess left ventricular size.
Renal imaging with either an ultrasound or an
intravenous pyelogram reveals that kidney size is usually
symmetric and may be normal or modestly reduced.
The renal calices and pelves are normal.
Renal asymmetry or irregularities in the contour raise the
possibility that hypertension could be secondary to renal
artery stenosis or reflux nephropathy
ECG typically shows left ventricular hypertrophy; the
sensitivity of ECG in helping to detect left ventricular
hypertrophy may be as low as 22%.
47
Histologic Findings (I)
medial and intimal thickening with intimal
fibrosis of preglomerular arterioles
hyalinosis of afferent arterioles
secondary tubular atrophy
interstitial fibrosis
malignant hypertension
Fibrinoid necrosis
microinfarcts
48
Histologic Findings (II)
GLOMERULAR CHANGES
Obsolescent glomeruli were defined as glomeruli in
which Bowman's space was occupied by collagenous,
PAS positive material, and the tuft was retracted
Solidified glomeruli were defined as glomeruli in
which the entire tuft was solidified, in the absence of
the collagenous change in the capsular space
Disappearing glomeruli were identified as globally
sclerotic glomeruli where there was an absence or
partial disappearance of Bowman's capsule
49
50
TREATMENT (I)
BP goal of less than 130/80 mm Hg to preserve renal function and to reduce
cardiovascular events in patients with hypertension and diabetes.
Lower BPs are recommended for patients with proteinuria greater than 1 g/d
and renal insufficiency, regardless of etiology
ACE inhibitors
Effects and indications
Reduce proteinuria
Specific renal protective effect both in diabetic and nondiabetic renal impairment
Reduce morbidity and mortality rates in congestive heart failure
Monotherapy less effective in older patients (>50 y)
Larger doses required in black patients
Inhibit or blunt all adverse metabolic effects of thiazides
Dose reduction required in renal failure
Reduce left ventricular hypertrophy and thirst
Adverse effects
Cough (approximately 10%)
Angioedema (rare)
Hyperkalemia (especially in renal tubular acidosis type IV)
GFR reduction in patients with impaired renal function
May precipitate acute renal failure in patients with renal artery stenosis
Interfere with breakdown of bradykinin
Contraindicated in pregnancy
51
TREATMENT (II)
Angiotensin II receptor antagonists
Effects and indications
Reduce proteinuria
Indicated in patients intolerant of ACE inhibitors
Can be used in combination with an ACE inhibitor
Do not cause cough
Reduce left ventricular hypertrophy and thirst similarly to ACE
inhibitors
Do not interfere with breakdown of bradykinin
Adverse effects
Hyperkalemia
May reduce GFR in patients with impaired renal function
May precipitate acute renal failure in patient with renal artery
stenosis
Angioedema (rare)
Contraindicated in pregnancy
Data in black patients limited
52
TREATMENT (III)
Calcium channel blockers
Effects and indications
Effective as monotherapy in black patients and elderly patients
Potentiate ACE inhibitor effects
Renal protection not proven
Reduce morbidity and mortality rates in congestive heart failure
Indicated in patients with diastolic dysfunction
No change in dose with renal failure
Adverse effects
Possible increase in cardiovascular mortality rate with short-acting
dihydropyridines
Edema
Constipation (verapamil)
Profound bradycardia possible when verapamil and diltiazem used
in combination with a beta-blocker
53
Malignant hypertension (1)
1% of patients with hypertension;
It may occur in patients with preexisting hypertension or
in a previously normotensive patient
Systolic BP can range from 150-290 mm Hg while
diastolic BP can vary from 100-180 mm Hg.
Keith-Wagener grade III (hemorrhages and exudates)
and grade IV retinal changes (papilledema) are the
hallmarks of malignant hypertension.
Acute heart failure: pulmonary edema can be the
presenting signs in approximately 10% of patients.
Left ventricular hypertrophy is present in as many as
75% of patients at presentation
54
Malignant hypertension (2)
60% of patients complain of headaches
5-10% cerebrovascular event (eg, focal
cerebral ischemia, cerebral/subarachnoid
hemorrhage)
hypertensive encephalopathy is
characterized by headache, nausea,
vomiting, and visual blurring, together with
impaired cognitive function, generalized
seizures, or cortical blindness.
55
Malignant hypertension (3)
microangiopathic hemolytic anemia (schistocytes,
thrombocytopenia, increased fibrin degradation products,
and increased fibrinogen) is frequently present
Renal involvement is common, but the degree of
severity varies
Proteinuria is common, but overt nephrotic syndrome is
unusual
30% of patients will have an elevated serum creatinine
level at presentation
Other symptoms include weakness, malaise, fatigue,
and weight loss
56
TREATMENT OF MALIGNANT
HYPERTENSION
Malignant hypertension complicated by organ
failure is a medical emergency and requires
rapid reduction in BP
In uncomplicated malignant hypertension, rapid
BP reduction is not as critical as in the previous
group with BP reduction by up to 20% of the
presenting values, or a systolic BP of greater
than 170 mm Hg in the first 24 hours has been
an acceptable target.
Vous aimerez peut-être aussi
- Curs 02 Renal Vascular DiseasesDocument56 pagesCurs 02 Renal Vascular DiseasesMadalina SercaianuPas encore d'évaluation
- Renal Vascular Diseases FinalDocument43 pagesRenal Vascular Diseases FinalAlina CazanPas encore d'évaluation
- Nefropat Vasc Rom CursDocument40 pagesNefropat Vasc Rom CursancutazPas encore d'évaluation
- Reno Vascular HypertensionDocument10 pagesReno Vascular HypertensionAhmed Ali Mohammed AlbashirPas encore d'évaluation
- Ischemic Nephropathy - Detection and Therapeutic InterventionDocument6 pagesIschemic Nephropathy - Detection and Therapeutic InterventionfransiskaPas encore d'évaluation
- Renovascular DisordersDocument60 pagesRenovascular DisordersWondwosen MulatuPas encore d'évaluation
- By DR - Vasudeva Chetty PakalaDocument97 pagesBy DR - Vasudeva Chetty Pakalaace forumPas encore d'évaluation
- Medical Management in Patients With Renovascular Hypertension 2013Document8 pagesMedical Management in Patients With Renovascular Hypertension 2013hmqPas encore d'évaluation
- Stroke Work Up: Neurosonology DR - Dedi Sutia, SP.S (N), FINADocument31 pagesStroke Work Up: Neurosonology DR - Dedi Sutia, SP.S (N), FINAaghniajolandaPas encore d'évaluation
- 4 HTA RenDocument37 pages4 HTA RenBordean LilianaPas encore d'évaluation
- Managing Acute Presentations of Atheromatous Renal Artery StenosisDocument9 pagesManaging Acute Presentations of Atheromatous Renal Artery StenosisDana MPas encore d'évaluation
- Aditya Neuro SeminarDocument53 pagesAditya Neuro SeminarAditya ParmarPas encore d'évaluation
- Renovascular Hypertension: Screening and Modern Management: Controversies in Cardiovascular MedicineDocument11 pagesRenovascular Hypertension: Screening and Modern Management: Controversies in Cardiovascular MedicineRahmat JayaPas encore d'évaluation
- Diagnosis and Management in Peripheral Artery Disease EditedDocument5 pagesDiagnosis and Management in Peripheral Artery Disease Editedwahyu suparnoPas encore d'évaluation
- Management of Coronary Artery Disease in Patients With Chronic Kidney DiseaseDocument4 pagesManagement of Coronary Artery Disease in Patients With Chronic Kidney Diseaseopi neanPas encore d'évaluation
- Prevalencia de La Enfermedad Ateroesclerotica Renal JH 2009Document8 pagesPrevalencia de La Enfermedad Ateroesclerotica Renal JH 2009Diego Andrés Mejía VascoPas encore d'évaluation
- Cardiorenal Syndrome: Asist. Univ. DR Tanasa AnaDocument30 pagesCardiorenal Syndrome: Asist. Univ. DR Tanasa AnaSofia RhellabPas encore d'évaluation
- RenoVascular HypertensionDocument34 pagesRenoVascular HypertensionAbira KhanPas encore d'évaluation
- Nrneph 2009 230Document9 pagesNrneph 2009 230Sergio GonzalezPas encore d'évaluation
- Renovascular Hypertension: Department of Vascular Interventional Radiology Kem HospitalDocument45 pagesRenovascular Hypertension: Department of Vascular Interventional Radiology Kem Hospitalamrita narangPas encore d'évaluation
- Wellen's Syndrome: Mohan GameshDocument28 pagesWellen's Syndrome: Mohan Gameshmyolie wuPas encore d'évaluation
- RENAL VASCULAR DISEASES UpdatedDocument97 pagesRENAL VASCULAR DISEASES UpdatedgibreilPas encore d'évaluation
- Problem 3.12 Study Guide 1 Causes of Renal Failure 1. Discuss The Causes of Acute (Pre-Renal, Renal and Post-Renal) and Chronic Renal FailureDocument48 pagesProblem 3.12 Study Guide 1 Causes of Renal Failure 1. Discuss The Causes of Acute (Pre-Renal, Renal and Post-Renal) and Chronic Renal FailureAnishilPas encore d'évaluation
- Influence of Progressive Renal Dysfunction in Chronic Heart FailureDocument6 pagesInfluence of Progressive Renal Dysfunction in Chronic Heart Failurenandhini raguPas encore d'évaluation
- Carotid Artery DiseaseDocument29 pagesCarotid Artery DiseaseJoe KhdeirPas encore d'évaluation
- Renal Artery InterventionsDocument43 pagesRenal Artery InterventionsVivek JaganathanPas encore d'évaluation
- Chronic Renal Failure 4-9-18Document27 pagesChronic Renal Failure 4-9-18Muhammad MakkiPas encore d'évaluation
- Renovascular Hypertension (M2) : G. Ashuntantang-SoméDocument23 pagesRenovascular Hypertension (M2) : G. Ashuntantang-SoméIdrissou FmsbPas encore d'évaluation
- Am Fam Physician. 2003 Jan 1 67 (1) :67-74.: January 1, 2003 Table of ContentsDocument13 pagesAm Fam Physician. 2003 Jan 1 67 (1) :67-74.: January 1, 2003 Table of ContentsaanyogiPas encore d'évaluation
- (Journal Reading) Renovascular HypertensionDocument18 pages(Journal Reading) Renovascular HypertensionAfza KerenPas encore d'évaluation
- Cardiovascular Problems in Long Term HemodialisisiDocument40 pagesCardiovascular Problems in Long Term Hemodialisisifransiska wijoyoPas encore d'évaluation
- 3 Renal Vascular Disease 3Document46 pages3 Renal Vascular Disease 3Coy NuñezPas encore d'évaluation
- Secondary HypertensionDocument9 pagesSecondary HypertensionGautam JoshPas encore d'évaluation
- Renovascular Hypertension (RVH) SeminarDocument58 pagesRenovascular Hypertension (RVH) SeminarfaizalmasoodiPas encore d'évaluation
- A Doppler-Based Evaluation of Peripheral Lower Limb Arterial Insufficiency in Diabetes MellitusDocument4 pagesA Doppler-Based Evaluation of Peripheral Lower Limb Arterial Insufficiency in Diabetes Mellitusresta_pxdPas encore d'évaluation
- Nephrosclerosis. The Cinderella of Chronic KidneydiseasDocument5 pagesNephrosclerosis. The Cinderella of Chronic KidneydiseasMario Ivan De la Cruz LaraPas encore d'évaluation
- ADPKDDocument75 pagesADPKDVenkataramanan KrishnamoorthyPas encore d'évaluation
- Cardiac SarcoidosisDocument13 pagesCardiac SarcoidosisEmeric Jorge Macedo VendezuPas encore d'évaluation
- Revista Médica de ChileDocument8 pagesRevista Médica de ChileLudwigPlateBargielaPas encore d'évaluation
- Hypertensive Retinopathy - Yanoff and DukerDocument13 pagesHypertensive Retinopathy - Yanoff and DukerriveliPas encore d'évaluation
- Review Trombosis CerebrovascularDocument10 pagesReview Trombosis CerebrovascularDiego Velásquez HerreraPas encore d'évaluation
- Renovascular Hypertension and Ischemic Nephropathy: Marc A. PohlDocument24 pagesRenovascular Hypertension and Ischemic Nephropathy: Marc A. PohlFadli DalvinPas encore d'évaluation
- Cheitlin 2006Document3 pagesCheitlin 2006JuanPas encore d'évaluation
- Preoperative Care of Patients With Kidney DiseaseDocument13 pagesPreoperative Care of Patients With Kidney Disease84ghmynprvPas encore d'évaluation
- Boala Cronica de Rinichi Adrian CovicDocument85 pagesBoala Cronica de Rinichi Adrian CovicLorenaPas encore d'évaluation
- Surgical Coronary Revascularization Who, What, WhenDocument68 pagesSurgical Coronary Revascularization Who, What, WhenAlaaGaballaPas encore d'évaluation
- Grant2014 PDFDocument10 pagesGrant2014 PDFRalucaPas encore d'évaluation
- L11 Renal Failure General Approach 230213 002819Document16 pagesL11 Renal Failure General Approach 230213 002819S sPas encore d'évaluation
- Evidence-Based NephrologyD'EverandEvidence-Based NephrologyDonald A. Molony, M.D.Pas encore d'évaluation
- Neurovascular Disorders and NeurotoxicologyDocument33 pagesNeurovascular Disorders and NeurotoxicologyMaroofAliPas encore d'évaluation
- Carotid Endarterectomy FinalDocument48 pagesCarotid Endarterectomy Finalimad mokalledPas encore d'évaluation
- Eci 12222Document9 pagesEci 12222Andikaputra Brahma WidiantoroPas encore d'évaluation
- Acute Renal Failure in The Hospital: Diagnosis and ManagementDocument8 pagesAcute Renal Failure in The Hospital: Diagnosis and ManagementJulio César Valdivieso AguirrePas encore d'évaluation
- Cardiovaskular Disease & Risk of Kidney DiseaseDocument34 pagesCardiovaskular Disease & Risk of Kidney DiseaseErwin RachmadPas encore d'évaluation
- Primary Care - Nephrology Interface: Providing Coordinated CKD CareDocument158 pagesPrimary Care - Nephrology Interface: Providing Coordinated CKD CarecamidocPas encore d'évaluation
- Cardiac Sarcoidosis EditedDocument45 pagesCardiac Sarcoidosis Editedgovind rajPas encore d'évaluation
- Cardiorenal SyndromeDocument21 pagesCardiorenal SyndromeAndy McCulloughPas encore d'évaluation
- Hiponatremia e Hiper Natremia y MortalidadDocument8 pagesHiponatremia e Hiper Natremia y MortalidadJCPas encore d'évaluation
- High Prevalence of Subclinical Left Ventricular Dysfunction in Patients With Psoriatic ArthritisDocument8 pagesHigh Prevalence of Subclinical Left Ventricular Dysfunction in Patients With Psoriatic ArthritisEmanuel NavarretePas encore d'évaluation
- 1 ExClinic NefrologieDocument26 pages1 ExClinic NefrologieRodica BadeaPas encore d'évaluation
- Installation of A Mac Book LaptopDocument1 pageInstallation of A Mac Book Laptopjohny3333Pas encore d'évaluation
- TiroidaDocument68 pagesTiroidaayannapui100% (1)
- Apple MagazineDocument92 pagesApple Magazinejohny3333Pas encore d'évaluation
- Apple MagazineDocument92 pagesApple Magazinejohny3333Pas encore d'évaluation
- Windowsitpro201206 DLDocument168 pagesWindowsitpro201206 DLjohny3333Pas encore d'évaluation
- Abdominal Compartment Syndrome in ChildrenDocument12 pagesAbdominal Compartment Syndrome in Childrendian adiPas encore d'évaluation
- Acute Glomerulonephriti S: Group 3Document25 pagesAcute Glomerulonephriti S: Group 3AradhanaRamchandaniPas encore d'évaluation
- RPNDocument21 pagesRPNAruna Teja Chennareddy50% (8)
- DLP-Bohol - Science9 Q1 W2 D4Document6 pagesDLP-Bohol - Science9 Q1 W2 D4Marfe MontelibanoPas encore d'évaluation
- Arterias FacialesDocument23 pagesArterias FacialesDaniela GonzalezPas encore d'évaluation
- The Renin-Angiotensin Aldosterone System: Pathophysiological Role and Pharmacologic InhibitionDocument12 pagesThe Renin-Angiotensin Aldosterone System: Pathophysiological Role and Pharmacologic Inhibitionfatimah hasibuanPas encore d'évaluation
- Ventricular Septal DefectDocument6 pagesVentricular Septal DefectYannah Mae EspineliPas encore d'évaluation
- WelfareDocument23 pagesWelfareUmar BajwaPas encore d'évaluation
- Lecture 1 GestosesDocument22 pagesLecture 1 GestosesDrRaghavender ReddyPas encore d'évaluation
- "A Research Proposal On Drug As Social Problem ": EnglishDocument5 pages"A Research Proposal On Drug As Social Problem ": EnglishArsalan HahaPas encore d'évaluation
- Aapher Physical Fitness Test: S.No Test Items ProposeDocument15 pagesAapher Physical Fitness Test: S.No Test Items ProposeS. VeeravelPas encore d'évaluation
- NURS325 05 Antepartum ComplicationDocument81 pagesNURS325 05 Antepartum ComplicationaliPas encore d'évaluation
- Hum For HealthDocument2 pagesHum For HealthRoland DuretPas encore d'évaluation
- MDN Info Services IIDocument80 pagesMDN Info Services IIapi-3752698100% (2)
- Kishi2019-Carvedilol and Bisoprolol As Initial Therapy For Adult HypertensionDocument8 pagesKishi2019-Carvedilol and Bisoprolol As Initial Therapy For Adult HypertensionfikriafisPas encore d'évaluation
- Antihypertensives Summary Katzung PharmacologyDocument8 pagesAntihypertensives Summary Katzung PharmacologyRobin TolentinoPas encore d'évaluation
- Hipertension ArticuloDocument8 pagesHipertension ArticuloAngie CalderónPas encore d'évaluation
- Tensoval Comfort Classic ManualDocument2 pagesTensoval Comfort Classic Manualpocopepe2023Pas encore d'évaluation
- Al-Rokh's Pacemaker of PacesDocument312 pagesAl-Rokh's Pacemaker of PacesM H Safayet80% (5)
- HOPE: Health Optimizing Physical EducationDocument41 pagesHOPE: Health Optimizing Physical Educationjoe blowPas encore d'évaluation
- Hypertension SlidesDocument166 pagesHypertension SlidesStella CooKeyPas encore d'évaluation
- C.2 Computing and Justifying Score of Health ProblemsDocument3 pagesC.2 Computing and Justifying Score of Health ProblemsHannah Angelu Cabading100% (1)
- 1st Level Assessment JAVIER FOR STA CRUZ CASEDocument4 pages1st Level Assessment JAVIER FOR STA CRUZ CASEAndee SalegonPas encore d'évaluation
- 1 CV Disorder Case Presentation 1 (2022)Document5 pages1 CV Disorder Case Presentation 1 (2022)Wendera T. S CooperPas encore d'évaluation
- Pulmonary HypertensionDocument8 pagesPulmonary Hypertensionmerin sunilPas encore d'évaluation
- Blood Pressure Chart - Normal Blood Pressure RangeDocument6 pagesBlood Pressure Chart - Normal Blood Pressure RangeKho Cheng KhangPas encore d'évaluation
- CRS Report For Congress: Life Expectancy in The United StatesDocument33 pagesCRS Report For Congress: Life Expectancy in The United StatesAdrian Saporta100% (1)
- Xii Physical Education PracticalDocument47 pagesXii Physical Education PracticalNikhil SainiPas encore d'évaluation
- Present Perfect Tense and Checking Vital SignDocument21 pagesPresent Perfect Tense and Checking Vital SignSyah TrianaPas encore d'évaluation
- Readers Digest International May 2017Document131 pagesReaders Digest International May 2017HalaPas encore d'évaluation