Académique Documents
Professionnel Documents
Culture Documents
Patofisiologi Nyeri Pada Kelainan Biliodigestif
Transféré par
bocah_britpop0 évaluation0% ont trouvé ce document utile (0 vote)
213 vues25 pagesPain is an unpleasant phenomenon that is uniquely experienced by each individual. Pain is not always associated with the degree of the damaged tissue. Infants in the first 1 to 2 days of life are less sensitive to pain. A full behavioural response to pain is apparent at 3 to 12 month of life. Older children, between the ages of 15 and 18 years, tend to have a lower pain threshold than do adults.
Description originale:
Titre original
PATOFISIOLOGI NYERI PADA KELAINAN BILIODIGESTIF.pptx
Copyright
© © All Rights Reserved
Formats disponibles
PPTX, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentPain is an unpleasant phenomenon that is uniquely experienced by each individual. Pain is not always associated with the degree of the damaged tissue. Infants in the first 1 to 2 days of life are less sensitive to pain. A full behavioural response to pain is apparent at 3 to 12 month of life. Older children, between the ages of 15 and 18 years, tend to have a lower pain threshold than do adults.
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PPTX, PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
213 vues25 pagesPatofisiologi Nyeri Pada Kelainan Biliodigestif
Transféré par
bocah_britpopPain is an unpleasant phenomenon that is uniquely experienced by each individual. Pain is not always associated with the degree of the damaged tissue. Infants in the first 1 to 2 days of life are less sensitive to pain. A full behavioural response to pain is apparent at 3 to 12 month of life. Older children, between the ages of 15 and 18 years, tend to have a lower pain threshold than do adults.
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PPTX, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 25
Oleh :
Radityo Budi Leksono (DIT)
Pembimbing
dr. Syaiful Mukhtar Sp.B (K) BD
The definition of pain according to the
International Association for the Study of
Pain (IASP, 1979) is an unpleasant sensory
and emotional experience associated with
actual or potential tissue damage, or
described in terms of such damage
Pain is not always associated with the
degree of the damaged tissue
Pain is an unpleasant phenomenon that is
uniquely experienced by each individual, it
cannot be adequately defined, identified, or
measured by an observer
Pain threshold and pain tolerance
The pain threshold is the point at which a stimulus is perceived
as pain
It does not vary significantly among healthy people or in the same
person over time
Perceptual dominance- intense pain at one location may cause
an increase in the pain threshold in another location
The pain tolerance is expressed as duration of time or the
intensity of pain that an individual will endure before initiation
overt pain responses.
It is influenced by - persons cultural prescriptions
- expectations
- role behaviours
- physical and mental health
Pain tolerance is generally decreased:
- with repeated exposure to pain,
- by fatigue, anger, boredom, apprehension,
- sleep deprivation
Tolerance to pain may be increased:
- by alcohol consumption,
- medication, hypnosis,
- warmth, distracting activities,
- strong beliefs or faith
Pain tolerance varies greatly among people and in
the same person over time
A decrease in pain tolerance is also evident in the elderly,
and women appear to be more tolerant to pain than men
Age and perception of pain
Children and the elderly may experience or express pain
differently than adults
Infants in the first 1 to 2 days of life are less sensitive to pain
(or they simply lack the ability to verbalise the pain experience).
A full behavioural response to pain is apparent at 3 to 12 month of
life
Older children, between the ages of 15 and 18 years,
tend to have a lower pain threshold than do adults
Pain threshold tends to increase with ageing
This change is probably caused by peripheral neuropathies and
changes in the thickness of the skin
Pain categories
1. Somatogenic pain is pain with cause (usually known)
localised in the body tissue
a/ nociceptive pain
b/ neuropatic pain
2. Psychogenic pain is pain for which there is no known
physical cause but processing of sensitive information
in CNS is dysturbed
Acute and chronic pain
Acute pain is a protective mechanism that alerts the
individual to a condition or experience that is immediately
harmful to the body
Onset - usually sudden
Relief - after the chemical mediators that stimulate the
nociceptors, are removed
This type of pain mobilises the individual to prompt action
to relief it
Stimulation of autonomic nervous system can be observed
during this type of pain (mydriasis, tachycardia, tachypnoe,
sweating, vasoconstriction)
Responses to acute pain
- increased heart rate - diaphoresis
- increased respiratory rate - blood sugar
- elevated blood pressure - gastric acid secretion
- pallor or flushing, - gastric motility
dilated pupils - blood flow to the viscera,
kidney and skin
- nausea occasionally
occurs
Psychological and behavioural response to acute pain
- fear
- general sense of unpleasantness or unease
- anxiety
Chronic pain is persistent or intermittent usually defined as
lasting at least 6 months
The cause is often unknown, often develops insidiously, very
often is associated with a sense of hopelessness and
helplessness. Depression often results
Psychological response to chronic pain
Intermittent pain produces a physiologic response similar to
acute pain.
Persistent pain allows for adaptation (functions of the body are
normal but the pain is not reliefed)
Chronic pain produces significant behavioural and
psychological changes
The main changes are:
- depression
- an attempt to keep pain - related behaviour to a minimum
- sleeping disorders
- preoccupation with the pain
- tendency to deny pain
Acute Pain or Nociceptive Pain is pain that
elicited by activation of nociceptors
There are 4 distinct process involved:
1. Transduction
2. Transmission
3. Modulation and
4. Perception
Pain Perception
Brain
Dorsal Root
Ganglion
Dorsal Horn
Nociceptor
Spinal Cord
Gottschalk A et al. Am Fam Physician. 2001;63:1979-84.
Fields HL et al. Harrisons Principles of Internal Medicine. 1998:53-8.
1.
Transduction Conversion of noxious stimuli
(mechanical, thermal, chemical into
electrical activation
2
Transmission Communication of the nerve impulse
from the periphery to the spinal cord,
up to spinothalamic track to the
thalamus and cerebral cortex
3
Modulation Process by which impulse travel from
the brain back down to the spinal cord
to selectiveley inhibit (or sometimes
amlpify) pain impulse
4
Perception Net result of three events the
subjective experience of pain
An alarm protection tell us that something wrong in our
body
Accompanied by emotional reaction like nausea, fear,
anxiety, and discomfort
There is an urgency feeling for relieving the pain in the right
upper abdominal area
The Location of pain
The quality and intensivity of pain
Duration of pain
What time did the pain appear
Refered pain
Accompanying symptoms Symptom yang menyertai
Physical examination Pemeriksaan fisik
Laboratorium valuesLaboratorium
Ulcer
Intestinal
Colic
Biliary Colic,
Pancreatic
The Result from stimulation of the autonomic
nerve in the visceral peritoneum surrounding the
internal organs.
The Pain/noxius stimuli will be transferred to the
spinal cord through the symphatetic route.
The pain is hard to localize
Intermittent, cramp dan colicy pain
Usually accompanied with nausea, vomitting,
and diaphoresis
Stimuli occur from the iritation of the parietal
peritoneum.
Somatic pain impulses is conducted through
the peripheral nerve system, therefore it could
be better localized.
The somatic pain characteristic are continous,
constant, and usually worsen by cough or
changing of the body position. Nyeri terus
menerus, konstan, memburuk dengan
perubahan posisi, batuk
It is elicited by firmly placing a hand at the costal
margin in the right upper abdominal quadrant and
asking the patient to breathe deeply. If the gallbladder
is inflamed, the patient will experience pain and catch
their breath as the gallbladder descends and contacts
the palpating hand.
A positive Murphy's sign is seen in acute cholecystitis.
In cholecystitis, the gallbladder becomes inflamed
secondary to blockage of the cystic duct, usually by a
gallstone. Subsequently, this inflammation causes the
release of prostaglandins, which cause more
inflammation of the gallbladder. Patients with acute
cholecystitis experience discomfort with the Murphys
sign maneuver because the inflamed gallbladder
descends toward the examiners fingers, which
irritates the peritoneum, thereby causing pain.
TERIMA KASIH
Vous aimerez peut-être aussi
- Worksheet SR-FAITHDocument4 pagesWorksheet SR-FAITHPPDSNeurologiAgustus 2021Pas encore d'évaluation
- Manajemen Fraktur PelvisDocument30 pagesManajemen Fraktur PelvisNadya Wiratami NurrakhmawatiPas encore d'évaluation
- Intraabdominal Pressure MonitoringDocument10 pagesIntraabdominal Pressure Monitoringbocah_britpopPas encore d'évaluation
- US Gall Bl. Biliary TreeDocument20 pagesUS Gall Bl. Biliary TreeNenad V. DjokicPas encore d'évaluation
- Mirizzi Syndrome - UpToDateDocument15 pagesMirizzi Syndrome - UpToDateEdgar Miguel ContrerasPas encore d'évaluation
- Jurnal CA TyroidDocument4 pagesJurnal CA TyroidErvina ZelfiPas encore d'évaluation
- Cara Mengukur Tekanan IntrakompartemenDocument2 pagesCara Mengukur Tekanan Intrakompartemenfatimah putriPas encore d'évaluation
- Soft Tissue TumorDocument248 pagesSoft Tissue TumorDabessa MosissaPas encore d'évaluation
- Jurnal Tyroid PDFDocument3 pagesJurnal Tyroid PDFVinnaPas encore d'évaluation
- Jurnal Hepatitis BDocument42 pagesJurnal Hepatitis BGiffari AnugrahPas encore d'évaluation
- Kompartemen SindromDocument9 pagesKompartemen SindromPutri PratiwiPas encore d'évaluation
- HEMOROIDDocument29 pagesHEMOROIDDanang Aryo PinujiPas encore d'évaluation
- Gambaran Benigna Prostat Hiperplasia Di RSUP Prof. Dr. R. D. Kandou Manado Periode Januari 2014 - Juli 2017Document3 pagesGambaran Benigna Prostat Hiperplasia Di RSUP Prof. Dr. R. D. Kandou Manado Periode Januari 2014 - Juli 2017Gado GadoPas encore d'évaluation
- Trauma BuliDocument32 pagesTrauma BulimoonlightsoantaPas encore d'évaluation
- Klippel Trenaunay SyndromeDocument15 pagesKlippel Trenaunay SyndromeamsirlimbongPas encore d'évaluation
- Infeksi NosokomialDocument29 pagesInfeksi NosokomialAlunaficha Melody KiraniaPas encore d'évaluation
- Oeis SyndromeDocument9 pagesOeis SyndromeADEEPas encore d'évaluation
- Kuliah Radiologi Emergensi - Maret 2020 - PlainDocument67 pagesKuliah Radiologi Emergensi - Maret 2020 - PlainArief VerditoPas encore d'évaluation
- EGDT SepsisDocument8 pagesEGDT Sepsissiti fatmalaPas encore d'évaluation
- Gastric Carcinoma: Professor Ravi KantDocument44 pagesGastric Carcinoma: Professor Ravi KantAna Quintana100% (1)
- Hubungan Beberapa Indikator Obesitas Dengan Kadar Asam UratDocument17 pagesHubungan Beberapa Indikator Obesitas Dengan Kadar Asam UratarbiantoniPas encore d'évaluation
- Definisi NyeriDocument10 pagesDefinisi NyeriDaniel ZaputraPas encore d'évaluation
- Giant Juvenile Fibroadenoma of Breast Mimicking Phylloides Tumour - A Case ReportDocument8 pagesGiant Juvenile Fibroadenoma of Breast Mimicking Phylloides Tumour - A Case ReportsridharPas encore d'évaluation
- 2013 - Pancreaticoduodenectomy (Whipple Procedure) TechniquesDocument11 pages2013 - Pancreaticoduodenectomy (Whipple Procedure) TechniquesOlteanu IonutPas encore d'évaluation
- Hirschsprung DiseaseDocument20 pagesHirschsprung DiseaseIyan AsianaPas encore d'évaluation
- Bone: Cystic & Neoplastic LesionsDocument83 pagesBone: Cystic & Neoplastic LesionsPuspita PrihatiniPas encore d'évaluation
- Stress UlcerDocument20 pagesStress UlcerTaufik Akbar Faried LubisPas encore d'évaluation
- CCDuodenum Periampullary Neoplasms ChuDocument68 pagesCCDuodenum Periampullary Neoplasms ChuSahirPas encore d'évaluation
- Kuliah Prinsip 4 Box Etik (Compatibility Mode)Document3 pagesKuliah Prinsip 4 Box Etik (Compatibility Mode)Olivia NurudhiyaPas encore d'évaluation
- 6INVAGINASIDocument18 pages6INVAGINASIhazelelPas encore d'évaluation
- Hernia UmbilikalisDocument16 pagesHernia UmbilikalisWibhuti EmrikoPas encore d'évaluation
- Shock Management, by Ayman RawehDocument15 pagesShock Management, by Ayman RawehaymxPas encore d'évaluation
- Tumor Jaringan LunakDocument64 pagesTumor Jaringan LunakEdo Pramana PutraPas encore d'évaluation
- Fistel Vesicovaginalis, Ureterocutaneous, Dan UreterorectalisDocument24 pagesFistel Vesicovaginalis, Ureterocutaneous, Dan Ureterorectalismizz_jcPas encore d'évaluation
- Patologi Anatomi Kelainan MuskuloskeletalDocument38 pagesPatologi Anatomi Kelainan Muskuloskeletalmuthia saniPas encore d'évaluation
- WIFI Score For Diabetes Foot UlcerDocument17 pagesWIFI Score For Diabetes Foot Ulcertonylee24100% (1)
- Thyroid Cancer Diagnosis and ManagementDocument45 pagesThyroid Cancer Diagnosis and Managementapi-3704562100% (1)
- ROZERPLASTYDocument13 pagesROZERPLASTYSaraya AmajidaPas encore d'évaluation
- Cleftlipandpalate 111008125422 Phpapp02Document81 pagesCleftlipandpalate 111008125422 Phpapp02samira fatimaPas encore d'évaluation
- PPT Bedah DigestifDocument28 pagesPPT Bedah DigestifFatima Rima AndiniPas encore d'évaluation
- Sitogenetika&variasi GenetikDocument147 pagesSitogenetika&variasi GenetikDiniPas encore d'évaluation
- PPTDocument27 pagesPPTmonicanasutionPas encore d'évaluation
- Hartmann's Procedure: Patient Information - General SurgeryDocument7 pagesHartmann's Procedure: Patient Information - General SurgeryputriPas encore d'évaluation
- Fraktur Humerus Sepertiga DistalDocument26 pagesFraktur Humerus Sepertiga DistalNurul Rezki Fitriani AzisPas encore d'évaluation
- Blunt Adominal TraumaDocument13 pagesBlunt Adominal TraumaIlham RamadhanPas encore d'évaluation
- Tumor GinjalDocument26 pagesTumor GinjalElisa NurmahidaPas encore d'évaluation
- Clinical Trial Design Kuliah MKDU 2020Document51 pagesClinical Trial Design Kuliah MKDU 2020Christine100% (1)
- Primary Management of Maxillofacial TraumaDocument34 pagesPrimary Management of Maxillofacial TraumafitsumPas encore d'évaluation
- Checklist Jurnal STARDDocument17 pagesChecklist Jurnal STARDDhiyaulhaq Aqilatul FHPas encore d'évaluation
- Spleen: DR - Supriti Demonstrator Anatomy Deptt TMMC&RCDocument35 pagesSpleen: DR - Supriti Demonstrator Anatomy Deptt TMMC&RCBilal Yimam100% (1)
- Abdominal Distention inDocument45 pagesAbdominal Distention inArif Rahman DmPas encore d'évaluation
- Memahami Prima FacieDocument26 pagesMemahami Prima Faciewicak_spPas encore d'évaluation
- Lefort 1 OsteotomyDocument36 pagesLefort 1 OsteotomyNidhi Jayan100% (2)
- JAAOS-Management of Hemorrhage in Life-Threatening Pelvic Fracture 162Document11 pagesJAAOS-Management of Hemorrhage in Life-Threatening Pelvic Fracture 162Enny Yunita HariantiPas encore d'évaluation
- Slide Perbedaan Appendicitis Akut, Appendicitis Infiltrat Dan AbsesDocument30 pagesSlide Perbedaan Appendicitis Akut, Appendicitis Infiltrat Dan AbsesJessica Giovanni RuntuPas encore d'évaluation
- BPHDocument10 pagesBPHMichelle SalimPas encore d'évaluation
- Modul Wound Bed Preparation DR Ardianto SucintaDocument37 pagesModul Wound Bed Preparation DR Ardianto SucintaArdianto SucintaPas encore d'évaluation
- Anal Stenosis and Mucosal EctropionDocument7 pagesAnal Stenosis and Mucosal EctropionpologroPas encore d'évaluation
- Chest TubeDocument8 pagesChest TubeTaufik Nur YahyaPas encore d'évaluation
- Trauma UrogenitalDocument17 pagesTrauma UrogenitalsultantraPas encore d'évaluation
- Jejunum IleumDocument55 pagesJejunum IleumDitas ChuPas encore d'évaluation
- Unit 5 PainDocument133 pagesUnit 5 Painnoo.wannPas encore d'évaluation
- Unit 9 - Pain ManagementDocument36 pagesUnit 9 - Pain ManagementPetrinaPas encore d'évaluation
- 03 - Energy BalanceDocument8 pages03 - Energy Balancebocah_britpopPas encore d'évaluation
- 17 - The Traumatized PatientDocument7 pages17 - The Traumatized Patientbocah_britpopPas encore d'évaluation
- 03 - Nutritional Screening and Assessment PDFDocument8 pages03 - Nutritional Screening and Assessment PDFbocah_britpop100% (1)
- ACS SabistonDocument10 pagesACS Sabistonbocah_britpopPas encore d'évaluation
- 08 - Oral and Sip FeedingDocument11 pages08 - Oral and Sip Feedingbocah_britpopPas encore d'évaluation
- 17 - Enhanced Recovery PrinciplesDocument7 pages17 - Enhanced Recovery Principlesbocah_britpopPas encore d'évaluation
- 08 - Indications, Contraindications, Complications and Monitoring of enDocument13 pages08 - Indications, Contraindications, Complications and Monitoring of enbocah_britpopPas encore d'évaluation
- Case Disc RadioDocument29 pagesCase Disc Radiobocah_britpopPas encore d'évaluation
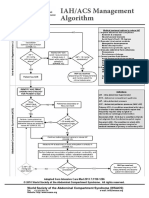
- IAH ACS Management 2014Document1 pageIAH ACS Management 2014bocah_britpopPas encore d'évaluation
- Tuesday, March 09 2015: Team in ChargeDocument2 pagesTuesday, March 09 2015: Team in Chargebocah_britpopPas encore d'évaluation
- IAH ACS Medical Management 2014Document1 pageIAH ACS Medical Management 2014bocah_britpopPas encore d'évaluation
- University of Colorado NICHE Practice Survey SummaryDocument48 pagesUniversity of Colorado NICHE Practice Survey Summarybocah_britpopPas encore d'évaluation
- Tuesday, March 09 2015: Team in ChargeDocument7 pagesTuesday, March 09 2015: Team in Chargebocah_britpopPas encore d'évaluation
- Femur Fractures in Infants and Young ChildrenDocument3 pagesFemur Fractures in Infants and Young Childrenbocah_britpopPas encore d'évaluation
- Femur Fractures in The Pediatric Population: Abuse or Accidental Trauma?Document7 pagesFemur Fractures in The Pediatric Population: Abuse or Accidental Trauma?bocah_britpopPas encore d'évaluation
- Spectrum of Operative Childhood Intra-Articular Shoulder PathologyDocument4 pagesSpectrum of Operative Childhood Intra-Articular Shoulder Pathologybocah_britpopPas encore d'évaluation
- Art 3A10.1007 2Fs11832 014 0590 3Document7 pagesArt 3A10.1007 2Fs11832 014 0590 3bocah_britpopPas encore d'évaluation
- Pediatrics 2010 Ravichandiran 60 6Document9 pagesPediatrics 2010 Ravichandiran 60 6bocah_britpopPas encore d'évaluation
- Gastrointestinal Quiz AnswersDocument5 pagesGastrointestinal Quiz AnswersFranciskhokhyx III100% (5)
- CholelithiasisDocument6 pagesCholelithiasisLara GatbontonPas encore d'évaluation
- CholecystitisDocument10 pagesCholecystitisCris Pin BumatangPas encore d'évaluation
- Gallbladder Diseases Are Most Often Caused by GallstonesDocument8 pagesGallbladder Diseases Are Most Often Caused by GallstonesCharlie C. SanchezPas encore d'évaluation
- MS QuizDocument18 pagesMS QuizCharlyn JenselPas encore d'évaluation
- Cue and Clue PL Idx PDX PTX Pmo&EdDocument3 pagesCue and Clue PL Idx PDX PTX Pmo&EdIka AyuPas encore d'évaluation
- Gastrointestinal Imaging (Radcases)Document224 pagesGastrointestinal Imaging (Radcases)Marcelo RibeiroPas encore d'évaluation
- 3Document50 pages3akreditasirsurPas encore d'évaluation
- Gastrointestinal Osmosis HY Pathology Notes ATFDocument177 pagesGastrointestinal Osmosis HY Pathology Notes ATFaslamPas encore d'évaluation
- Acute Cholecystitis Ppt. DR Dilip S. RajpalDocument42 pagesAcute Cholecystitis Ppt. DR Dilip S. Rajpaldiliprajpal73100% (1)
- Plabable-Gems-6. Gastroenterology Plabable GemsDocument39 pagesPlabable-Gems-6. Gastroenterology Plabable GemsHabo Habo100% (1)
- DocxDocument53 pagesDocxkuro hanabusaPas encore d'évaluation
- Subhepatic Appendicitis - A Diagnostic DilemmaDocument4 pagesSubhepatic Appendicitis - A Diagnostic DilemmaAnonymous ysrxggk21c100% (1)
- 1 A PDFDocument51 pages1 A PDFMysheb SSPas encore d'évaluation
- Med-Surg HESI Study GuideDocument13 pagesMed-Surg HESI Study GuideTravis Hargett93% (14)
- TG 13 PDFDocument109 pagesTG 13 PDFnostra83Pas encore d'évaluation
- CHolelitiasis, CholesistitisDocument44 pagesCHolelitiasis, CholesistitistrianaamaliaPas encore d'évaluation
- Acute Acalculous CholecystitisDocument17 pagesAcute Acalculous CholecystitisTriono AssamsulPas encore d'évaluation
- Caso NEJM 27-2017Document9 pagesCaso NEJM 27-2017Leonardo PgPas encore d'évaluation
- DD 1Document73 pagesDD 1Abhirami Nair100% (1)
- Blangko BPJSDocument259 pagesBlangko BPJSJuwita Wonder GerL'womenchet ApriLioPas encore d'évaluation
- Hepatobiliary and Pancreatic AscariasisDocument12 pagesHepatobiliary and Pancreatic AscariasisVictoria CarvajalPas encore d'évaluation
- Abdominal UltrasoundDocument15 pagesAbdominal UltrasoundAmin100% (2)
- CASE STUDY CholecystitisDocument69 pagesCASE STUDY CholecystitisJustine CapunongPas encore d'évaluation
- Calculous Cholecystitis Revised 1Document70 pagesCalculous Cholecystitis Revised 1Gefran GefranPas encore d'évaluation
- MD MD MD MD MD MD: Since 1985, When The First Successful Laparoscopic Cho-Lecystectomy (LC) Was Performed by MüheDocument6 pagesMD MD MD MD MD MD: Since 1985, When The First Successful Laparoscopic Cho-Lecystectomy (LC) Was Performed by MüheJohn SmithPas encore d'évaluation
- Gallbladder CancerDocument5 pagesGallbladder CancerandyjayaPas encore d'évaluation
- Gallstones: Session 4Document2 pagesGallstones: Session 4Valeria Casiano CelisPas encore d'évaluation