Académique Documents
Professionnel Documents
Culture Documents
Hemolytic Uremic Syndrome
Transféré par
ummi ulfah100%(2)100% ont trouvé ce document utile (2 votes)
384 vues20 pagesHemolytic-uremic syndrome (HUS) is characterized by renal failure, hemolytic anemia, and thrombocytopenia. It is primarily caused by shiga toxin-producing bacteria like E. coli damaging endothelial cells in the kidneys. This leads to microvascular thrombosis and organ ischemia. Clinically, it presents as pallor, decreased urine output, and often diarrhea. Treatment involves supportive care, antibiotics for identifiable infections, plasma therapy for complement factor deficiencies, and immunosuppression in severe cases. With treatment, over 90% of patients survive the acute phase, though some develop long-term complications like high blood pressure, seizures, or end-stage renal disease.
Description originale:
simple description of Hemolytic Uremic Syndrome
Copyright
© © All Rights Reserved
Formats disponibles
PPTX, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentHemolytic-uremic syndrome (HUS) is characterized by renal failure, hemolytic anemia, and thrombocytopenia. It is primarily caused by shiga toxin-producing bacteria like E. coli damaging endothelial cells in the kidneys. This leads to microvascular thrombosis and organ ischemia. Clinically, it presents as pallor, decreased urine output, and often diarrhea. Treatment involves supportive care, antibiotics for identifiable infections, plasma therapy for complement factor deficiencies, and immunosuppression in severe cases. With treatment, over 90% of patients survive the acute phase, though some develop long-term complications like high blood pressure, seizures, or end-stage renal disease.
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PPTX, PDF, TXT ou lisez en ligne sur Scribd
100%(2)100% ont trouvé ce document utile (2 votes)
384 vues20 pagesHemolytic Uremic Syndrome
Transféré par
ummi ulfahHemolytic-uremic syndrome (HUS) is characterized by renal failure, hemolytic anemia, and thrombocytopenia. It is primarily caused by shiga toxin-producing bacteria like E. coli damaging endothelial cells in the kidneys. This leads to microvascular thrombosis and organ ischemia. Clinically, it presents as pallor, decreased urine output, and often diarrhea. Treatment involves supportive care, antibiotics for identifiable infections, plasma therapy for complement factor deficiencies, and immunosuppression in severe cases. With treatment, over 90% of patients survive the acute phase, though some develop long-term complications like high blood pressure, seizures, or end-stage renal disease.
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PPTX, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 20
BY: NAILUL MUNA BINTI AHMAD MUSADAD
Hemolytic-uremic syndrome (HUS) is a
clinical syndrome characterized by
progressive renal failure that is associated
with :
microangiopathic (nonimmune, Coombs-
negative) Hemolytic anemia
Uremia
Thrombocytopenia (Low platelet count)
.
The pathologic lesion of HUS
E. Coli Shigatoxin damages
endothelial cells
Endothelial swelling narrows
vessel lumen
Platelet/fibrin clots form blocking
blood flow
Poor blood flow(microcirculation
in kidney)
Low tissue oxygen (hypoxia)
Hypoxia
Cell dysfunction
Cell necrosis (death)
The typical pathophysiology involves the shiga-toxin binding to proteins on
the surface of glomerular endothelium and inactivating a metalloproteinase
called ADAMTS13, which is also involved in the closely related TTP
The arterioles and capillaries of the body become obstructed by the
resulting complexes of activated platelets which have adhered to
endothelium via large multimeric vWF.
The growing thrombi lodged in smaller vessels destroy RBCs as they
squeeze through the narrowed blood vessels, forming schistocytes, or
fragments of sheared RBCs.
The consumption of platelets as they adhere to the thrombi lodged in
the small vessels typically leads to mild or moderate
thrombocytopaenia
Type of HUS / TTP Specific Cause
Infection related Shiga toxin producing E.coli/Shigella***
Pneumococcal infection
HIV Typical
Other viral or bacterial infections
Complement factor abnormality Factor H deficiency
CTD Factor I deficiency
Miscellaneous Drugs Atypical
Malignancy
SLE
Radiation
Non-
Diarrhea
Related HUS
Diarrhea
associated/
Shiga Toxin
associated
HUS
Typical/Diarrhea associated/Shiga Toxin
associated HUS
Enterohaemorrhagic E. coli
Shigella dysenteriae type 1
Rarely, HUS can occur with E. coli UTI
Sources of infection are :
Milk and animal products (incompletely cooked beef, pork,
poultry,lamb)
Human feco-oral transmission
Vegetables, salads and drinking water
may be contaminated by bacteria
shed in animal wastes
The commonest clinical presentation of HUS
is :
Acute pallor
Oliguria
Diarrhea or dysentery
It occurs commonly in children between 1-5 years of
age
HUS develops about 5-10 days after onset of
diarrhea
Hematuria and hypertension are common.
Complications of fluid overload may present
with:
Pulmonary edema
Hypertensive encephalopathy
Despite thrombocytopenia, bleeding
manifestations are rare
Neurological symptoms like:
Irritability
Encephalopathy
Seizures
Full Blood Count (FBC)
Anaemia
thrombocytopenia
Peripheral blood smears
schistocytes
Reticulocyte count
reticulocytosis
Features of intravascular hemolysis
Raised unconjugated Bilirubin
Raised Lactate Dehydrogenase(LDH)
Decreased circulating level of haptoglobin
Creatinine
Urine analysis
Hemoglobinuria
Hematuria
Proteinuria
Schistocytes
In patients with diarrhea, the identification
of pathogenic EHEC or Shigella is performed
by:
Stool culture
Further serotyping by agglutination or enzyme
immunoassay
Rarely HUS can occur with E. coli UTI:
Urine cultures are indicated in non-diarrheal
patients
Bacteriological cultures of body fluids are
indicated in suspected pneumococcal
disease.
Sputum
CSF
Blood
Pus
Supportive Therapy
Antibiotics
Plasma Therapy
Miscellaneous
1. Supportive Therapy
In all patients, supportive treatment is primary.
Close clinical monitoring of :
Hydration status
Blood pressure
Neurological
Ventilatory parameters
Blood levels of glucose, electrolytes, creatinine
and full blood count need frequent monitoring
2. Antibiotics
E. coli
Shigellosis
pneumococcal HUS
3. Plasma Therapy
In aHUS due to :
complement factor abnormality
ADAMTS13 deficiency
The replacement of the deficient factor with Fresh Frozen Plasma
Daily plasma infusions (10 to 20 mL/kg/day)
Exchange of 1.5 times plasma volume ( 60 to 75 mL/kg/day) using FFP
With the onset of acute renal failure :
Fluid restriction
Diuretics
4. Miscellaneous
In infants with HUS associated with cobalamin abnormalities:
Treatment with hydroxycobalamin
Oral betaine
Folic acid
Normalizes the metabolic abnormalities can help to prevent further
episodes.
In patients with persistent ADAMTS13 antibodies and poor response to
plasma exchange:
Immunosuppressive therapy with high dose
steroids/cyclophosphamide/ cyclosporin/rituximab
Splenectomy
Recently, impressive results have been reported with the anti-C5
monoclonal antibody, eculizumab, which binds to C5, thereby
preventing activation of the terminal complement cascade.
With aggressive treatment, more than
90% survive the acute phase.
About 9% may develop end stage
renal disease.
About one-third of persons with HUS
have abnormal kidney function many
years later, and a few require long-
term dialysis.
Another 8% of persons with HUS have
other lifelong complications, such as :
High blood pressure
Seizures
Blindness
Paralysis
Vous aimerez peut-être aussi
- Pancytopenia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsD'EverandPancytopenia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsPas encore d'évaluation
- Hemolytic UremicsyndromeDocument60 pagesHemolytic UremicsyndromeMuhammad AleemPas encore d'évaluation
- A Simple Guide to Hyperaldosteronism, Diagnosis, Treatment and Related ConditionsD'EverandA Simple Guide to Hyperaldosteronism, Diagnosis, Treatment and Related ConditionsPas encore d'évaluation
- Hemolytic Uremic Syndrome: Ankit GurjarDocument18 pagesHemolytic Uremic Syndrome: Ankit GurjarAnkit Tonger AnkyPas encore d'évaluation
- Acute GlomerulonephritisDocument4 pagesAcute GlomerulonephritisJulliza Joy PandiPas encore d'évaluation
- Hemolytic Uremic SyndromeDocument10 pagesHemolytic Uremic SyndromeYonz LedesmaPas encore d'évaluation
- Hemolytic Uremic Syndrome (HUS) : Presented by Muhammad TariqDocument19 pagesHemolytic Uremic Syndrome (HUS) : Presented by Muhammad TariqHanif ullahPas encore d'évaluation
- Nephrotic Syndrome What Is Nephrotic Syndrome? CauseDocument10 pagesNephrotic Syndrome What Is Nephrotic Syndrome? CauseThuganamix50% (2)
- Acute GlomerulonephritisDocument11 pagesAcute Glomerulonephritisdayt0na_forda3464Pas encore d'évaluation
- DicDocument17 pagesDicCLEMENT0% (1)
- Schistosomiasis Case StudyDocument5 pagesSchistosomiasis Case Studyapi-318749549Pas encore d'évaluation
- Lecture Hemophilia and Thrombocytopenic PurpuraDocument55 pagesLecture Hemophilia and Thrombocytopenic PurpuraaymenPas encore d'évaluation
- PallorDocument16 pagesPallorManal AlQuaimi100% (1)
- Nephrotic SyndromeDocument57 pagesNephrotic SyndromePradnya WarthePas encore d'évaluation
- Nephrotic Syndrome: Ron Christian Neil T. Rodriguez, MD 1 Year Pedia ResidentDocument26 pagesNephrotic Syndrome: Ron Christian Neil T. Rodriguez, MD 1 Year Pedia ResidentRon Christian Neil RodriguezPas encore d'évaluation
- Nephrotic SyndromeDocument31 pagesNephrotic Syndromedrhananfathy100% (1)
- Rheumatic FeverDocument56 pagesRheumatic Feveralmawang100% (1)
- POLYCYTHEMIADocument29 pagesPOLYCYTHEMIAFaizan KhanPas encore d'évaluation
- Acute Liver FailureDocument24 pagesAcute Liver FailureMohd Johari Mohd ShafuwanPas encore d'évaluation
- Nephrotic SyndromeDocument35 pagesNephrotic SyndromesudhaPas encore d'évaluation
- Nephrotic SyndromeDocument42 pagesNephrotic SyndromeSushmaPas encore d'évaluation
- Hemolytic Disease of NewbornDocument15 pagesHemolytic Disease of Newborncyphochilus100% (1)
- Renal DisordersDocument77 pagesRenal Disorderslorelee_espaldon100% (1)
- Hepatitis VirusDocument37 pagesHepatitis Virusapi-19916399Pas encore d'évaluation
- HemophiliaDocument60 pagesHemophiliavibhurocksPas encore d'évaluation
- Infective Endocarditis: Ainal Fadly Adigama PF Enny SuryantiDocument50 pagesInfective Endocarditis: Ainal Fadly Adigama PF Enny SuryantiFaisal Reza AdiebPas encore d'évaluation
- Acute Glomerulonephritis (AGN)Document35 pagesAcute Glomerulonephritis (AGN)jennalyn_dejelo100% (1)
- Stroke and Cerebrovascular DiseaseDocument14 pagesStroke and Cerebrovascular DiseaseMarwan M.Pas encore d'évaluation
- UROLITHIASISDocument84 pagesUROLITHIASISJheanAlphonsineT.MeansPas encore d'évaluation
- Gastro Intestinal Bleeding DR - muayAD ABASSDocument59 pagesGastro Intestinal Bleeding DR - muayAD ABASSMAFADHELPas encore d'évaluation
- Poststreptococcal Glomerulonephritis - UpToDateDocument21 pagesPoststreptococcal Glomerulonephritis - UpToDateHandre Putra100% (1)
- Systemic Lupus Erythematosus (SLE)Document39 pagesSystemic Lupus Erythematosus (SLE)Nadya SabrinaPas encore d'évaluation
- Case Study Presentation - Nephrotic SyndromeDocument56 pagesCase Study Presentation - Nephrotic SyndromeVivien Marie89% (27)
- Acute Post-Streptococcal GlomerulonephritisDocument15 pagesAcute Post-Streptococcal GlomerulonephritisJeanne Marie ValesPas encore d'évaluation
- Transfusion Reaction and Coombs Test: Moderator:-Dr Sanjay Agrwal Presenter: - DR Pratima Singh PG Jr-1Document33 pagesTransfusion Reaction and Coombs Test: Moderator:-Dr Sanjay Agrwal Presenter: - DR Pratima Singh PG Jr-1UmikaguptaPas encore d'évaluation
- Aplastic Anemia Lecture 1aDocument39 pagesAplastic Anemia Lecture 1aniaaseta100% (2)
- Idiopathic Thrombocytopenic PurpuraDocument8 pagesIdiopathic Thrombocytopenic PurpuraMonette Abalos MendovaPas encore d'évaluation
- Nephroticsyndromeandacasereport 140727015201 Phpapp02Document38 pagesNephroticsyndromeandacasereport 140727015201 Phpapp02TareqhoseinPas encore d'évaluation
- Coagulation Disorders: Roxanne Jeen L. FornollesDocument42 pagesCoagulation Disorders: Roxanne Jeen L. FornollesAyen Fornolles100% (1)
- Thyroid StormDocument23 pagesThyroid Stormtogi_siahaanPas encore d'évaluation
- Exchange Blood TransfusionDocument38 pagesExchange Blood TransfusionMeseret Hamer Zewdie100% (1)
- Acute GlomerulonephritisDocument21 pagesAcute Glomerulonephritisbrinda johnPas encore d'évaluation
- Abruptio PlacentaDocument3 pagesAbruptio Placentachichilovesyou100% (1)
- Nephrotic SyndromeDocument36 pagesNephrotic SyndromedrtpkPas encore d'évaluation
- Presentation of Nephrotic SyndromeDocument15 pagesPresentation of Nephrotic SyndromeBagas NovandyPas encore d'évaluation
- GlomerulonephritisDocument58 pagesGlomerulonephritisJosa Anggi Pratama0% (1)
- Alcoholic Liver Disease HarrisonDocument3 pagesAlcoholic Liver Disease HarrisonJesly Charlies0% (1)
- Presentation Liver CirrhosisDocument26 pagesPresentation Liver CirrhosisFaye Dominique Roxas PalmaresPas encore d'évaluation
- Disseminated Intravascular CoagulationDocument2 pagesDisseminated Intravascular CoagulationGerardLum100% (1)
- Anemia of Chronic Disease - Inflammation - UpToDateDocument36 pagesAnemia of Chronic Disease - Inflammation - UpToDateDomenica MurilloPas encore d'évaluation
- CME Cyanotic Heart DiseaseDocument38 pagesCME Cyanotic Heart DiseaseTan Zhi HongPas encore d'évaluation
- Intestinal ObstructionDocument27 pagesIntestinal ObstructionAna AvilaPas encore d'évaluation
- Hepatitis ADocument21 pagesHepatitis Avanessa100% (6)
- Sickle Cell AnemiaDocument63 pagesSickle Cell Anemiaoss-20502745100% (4)
- Acute Kidney InjuryDocument19 pagesAcute Kidney InjuryAmit Ramrattan0% (1)
- Rheumatic FeverDocument21 pagesRheumatic FeverUmar Azlan50% (2)
- Chronic Kidney Disease Case StudyDocument52 pagesChronic Kidney Disease Case StudyGi100% (1)
- Chronic Renal FailureDocument46 pagesChronic Renal Failurestepharry08100% (1)
- Immune Thrombocytopenic Purpura PDFDocument12 pagesImmune Thrombocytopenic Purpura PDFAlvin PratamaPas encore d'évaluation
- Acute Glomerulonephritis: Mohd Zamir Ghouse 060100848Document40 pagesAcute Glomerulonephritis: Mohd Zamir Ghouse 060100848zamirsg100% (1)
- Surat CutiDocument1 pageSurat Cutiummi ulfahPas encore d'évaluation
- Acute Lymphoid LeukemiaDocument41 pagesAcute Lymphoid Leukemiaummi ulfahPas encore d'évaluation
- Surat CutiDocument1 pageSurat Cutiummi ulfahPas encore d'évaluation
- Comparison Chart Betw OA and RADocument4 pagesComparison Chart Betw OA and RAummi ulfah100% (1)
- Forever Living Presentation PDFDocument34 pagesForever Living Presentation PDFCasey Rion100% (1)
- Lista Verbelor Regulate - EnglezaDocument5 pagesLista Verbelor Regulate - Englezaflopalan100% (1)
- Gandhi Was A British Agent and Brought From SA by British To Sabotage IndiaDocument6 pagesGandhi Was A British Agent and Brought From SA by British To Sabotage Indiakushalmehra100% (2)
- Nahs Syllabus Comparative ReligionsDocument4 pagesNahs Syllabus Comparative Religionsapi-279748131Pas encore d'évaluation
- #6 Decision Control InstructionDocument9 pages#6 Decision Control InstructionTimothy King LincolnPas encore d'évaluation
- Work Immersion Experience at Formaply Inustry in Brgy. de Ocampo, Trece Martires City, CaviteDocument34 pagesWork Immersion Experience at Formaply Inustry in Brgy. de Ocampo, Trece Martires City, CaviteKen AshleyPas encore d'évaluation
- Module 3 - Lesson 3.1Document2 pagesModule 3 - Lesson 3.1Cj RomoPas encore d'évaluation
- Reliability Technoology For Submarine Repeaters PDFDocument8 pagesReliability Technoology For Submarine Repeaters PDFbolermPas encore d'évaluation
- 28Document12 pages28physicsdocsPas encore d'évaluation
- The Importance of Logo DesignDocument1 pageThe Importance of Logo DesignDanielPas encore d'évaluation
- The Recipe For Oleander Sou1Document4 pagesThe Recipe For Oleander Sou1Anthony SullivanPas encore d'évaluation
- Ergatividad Del Vasco, Teoría Del CasoDocument58 pagesErgatividad Del Vasco, Teoría Del CasoCristian David Urueña UribePas encore d'évaluation
- 206f8JD-Tech MahindraDocument9 pages206f8JD-Tech MahindraHarshit AggarwalPas encore d'évaluation
- Quarter 3 Week 6Document4 pagesQuarter 3 Week 6Ivy Joy San PedroPas encore d'évaluation
- List de VerbosDocument2 pagesList de VerbosmarcoPas encore d'évaluation
- Julie Jacko - Professor of Healthcare InformaticsDocument1 pageJulie Jacko - Professor of Healthcare InformaticsjuliejackoPas encore d'évaluation
- Balezi - Annale Générale Vol 4 - 1 - 2 Fin OkDocument53 pagesBalezi - Annale Générale Vol 4 - 1 - 2 Fin OkNcangu BenjaminPas encore d'évaluation
- My ResumeDocument2 pagesMy ResumeWan NaqimPas encore d'évaluation
- Foxit PhantomPDF For HP - Quick GuideDocument32 pagesFoxit PhantomPDF For HP - Quick GuidekhilmiPas encore d'évaluation
- 221-240 - PMP BankDocument4 pages221-240 - PMP BankAdetula Bamidele OpeyemiPas encore d'évaluation
- Q&A JurisdictionDocument20 pagesQ&A JurisdictionlucasPas encore d'évaluation
- 011 - Descriptive Writing - UpdatedDocument39 pages011 - Descriptive Writing - UpdatedLeroy ChengPas encore d'évaluation
- Java ReviewDocument68 pagesJava ReviewMyco BelvestrePas encore d'évaluation
- Panulaang FilipinoDocument21 pagesPanulaang FilipinoKriza Erin B BaborPas encore d'évaluation
- Liver Disease With PregnancyDocument115 pagesLiver Disease With PregnancyAmro Ahmed Abdelrhman100% (3)
- Old San Agustin NHS MSISAR Sept 2021Document2 pagesOld San Agustin NHS MSISAR Sept 2021ERICSON SABANGANPas encore d'évaluation
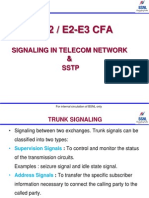
- Signalling in Telecom Network &SSTPDocument39 pagesSignalling in Telecom Network &SSTPDilan TuderPas encore d'évaluation
- Childbirth Self-Efficacy Inventory and Childbirth Attitudes Questionner Thai LanguageDocument11 pagesChildbirth Self-Efficacy Inventory and Childbirth Attitudes Questionner Thai LanguageWenny Indah Purnama Eka SariPas encore d'évaluation
- Klabin Reports 2nd Quarter Earnings of R$ 15 Million: HighlightsDocument10 pagesKlabin Reports 2nd Quarter Earnings of R$ 15 Million: HighlightsKlabin_RIPas encore d'évaluation
- Analog Electronic CircuitsDocument2 pagesAnalog Electronic CircuitsFaisal Shahzad KhattakPas encore d'évaluation