Académique Documents
Professionnel Documents
Culture Documents
Basic Lung Disease
Transféré par
Qurrataini IbanezCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Basic Lung Disease
Transféré par
Qurrataini IbanezDroits d'auteur :
Formats disponibles
Basic concepts in Lung disease
Contents
Embryology
Anatomic concepts
Physiologic concepts
Pathology
Clinical : symptoms
physical signs
disease patterns
Anatomic Concepts
Embryology : lung development starts from the
gut 24 days after conception; diaphragm forms in
cervical region at 3-4 weeks and moves
progressively downwards carrying the phrenic
nerves with; lung lobes are identifiable at 12
weeks; bronchial tree is completed at 16 weeks
and alveoli and capillaries appear at 24 28
weeks; surfactant appears at 35 weeks.
Postnatal Alveolarization: intense first 8-10 y
(alveolar buds hyperplastic growth) and
enlargement of all structures throughout
adolescence and early adulthood ( hypertrophic
growth)
Developmental abnormalities: tracheo-oesophageal
fistula, cleft palate, cysts, agenesis, sequestration,
cilia dysfunction and abnormal structure,
diaphragmatic hernias.
Shared nerve supply (Vagus) between respiratory
tract and GI tract Gastro-oesophageal reflux can
increase bronchial secretions (reflexively) and
cause bronchial constriction ( together with
oesophageal spasm).
Diaphragmatic irritation is often experienced as
pain in the cervical region (referred pain) from
where it evolved.
Anatomy
Surface Anatomy: borders of the pleura
borders of the lung
fissures
lung lobes
Bronchial tree, vascular and nerve supply,
lymphatics.
Angle of Louis
Histology, cilia, secretory and immunologic cells.
Physiology
Lung mechanics and Lung functions
Airway resistance
Diffusion :Gas laws ( Graham, alveoalar gas
equation)
Blood gases: PaO
2
, PaCO
2
, pH, HCO3, O
2
sat
Hemoglobin, dissociation curve, 2,3DPG
Surfactant
Control of Breathing
Pathology
Airway diseases: COPD, asthma, bronchiectasis,
cystic fibrosis, obstructive sleep apnoea
Parenchymal disease: pneumonia, ARDS,
Interstitial lung disease, pneumoconiosis
Pleural disease: pleural effusion, empyema.
Vascular disease: thrombo-embolism, primary
pulmonar hypertension
Neoplastic disease: Bronchus Ca, mesothelioma,
adenoma, carsinoid
Airway diseases
Causes: atopy, cigarette smoking, infection,
abnormal lung defense
Effect: obstruction to airflow
Mechanism: bronchospasm, inflammation, airway
remodelling, destruction, collapsing airways
Consequences: air flow ( FEV1, PEF); work
of breathing resp muscle fatigue respiratory
failure; PaO
2
, PaCO
2
PHT cor pulmonale
Parenchymal disease
consolidation - infection - typical/atypical
Oedema - cardiac vs non-cardiac (ARDS)
interstitial lung disease - idiopathic fibrosis,
sarcoidosis, hypersensitivity pneumonitis,
pneumoconiosis
Vascular secondary/primary PHT, cor
pulmonale, pulmonary thrombo-embolism
(unexplained dyspnea); Virchow triade: stasis,
coagulability, blood vessel abnormality, varicose
veins, endothelial dysfunction DVT risk
Pleural disease
Pleural effusion: alb, LDH, pleural/serum,
cholesterol, glucose, ADA, pH.
exudate: infection, inflammation, neoplastic,
blood ( permeability)
transudate: hypoproteinemia (renal, liver -
oncotic pressure), systemic venous hypertension
( hydrostatic pressure - Heart failure)
Empyema
Chylothorax, pseudo-chylothorax
Neoplastic disease
Bronchus Ca: squamous, small cell ca,
adeno ca, large cell ca, broncho-alveolar ca
Mesothelioma
Metastatic ca
Rare tumours: lymphoma, malt-lymphoma
Benign tumours
Control and Mechanism of
breathing
Alveolar hypoventilation
Sleep-related: central and obstructive sleep
apnoea, Ondines curse
Neuro-muscular diseases: polio, Guillain-
Barre syndrome, myasthenia gravis, resp
muscle fatigue, polimyositis
Chest wall: kyphoscoliosis, rib fractures
with flail chest
Complications of Lung disease
Cor pulmonale
Respiratory failure: ventilatory failure vs
oxygenation failure hypercapnia, acidosis
and hypoxaemia
Endstage lung disease
Pneumothorax
Clinical Manifestations
Dyspnea, PND, orthopnea, trepopnea, platypnea
and orthodeoxia.
Cough: productive vs non-productive, volume,
character, blood, post-nasal discharge
Chest pain: ischaemic, pleuritic, chest wall, GE
reflux, tearing of tissue
Constitutional: fever, night sweats, weight loss
RHF: swelling, pain R hypochondrium, abdominal
distention, palpitations
Physical signs
General: Cyanosis, anaemia, jaundice,
oedema, lymphadenopathy, clubbing
Respiratory examination:
1. Observation
2. Palpation
3. Percussion
4. Auscultation
Auscultation
Intensity of breath sounds: N, or absent
Character of breath sounds: N or bronchial
breathing/ amphoric breathing
Intensity of vocal sounds: (one-one, 99)N,
(bronchophony) or or nasal ( aegophony)
Whispering pectoriloquy ( 66)
Adventitious sounds: ronchi, creps, rubs,
clicks.
Lung sounds Possible mechanism Characteristics Causes
Wheezes
Rapid airflow through obstructed
airways caused by
bronchospasm, mucosal edema
High-pitched; most
often occur during
exhalation
Asthma, congestive heart
failure, bronchitis
Stridor
Rapid airflow through obstructed
airway caused by inflammation
High-pitched; often
occurs during
inhalation
Croup, epiglottitis,
postextubation
Crackles
I nsp & exp
Excess airway secretions moving
with airflow
Coarse and often clear
with cough
Bronchitis, respiratory
infections
Early insp
Sudden opening of proximal
bronchi
Scanty, transmitted to
mouth; not affected by
cough
Bronchitis, emphysema,
asthma
Late insp
Sudden opening of peripheral
airways
Diffuse, fine; occur
initially in dependent
regions
Atelectasis, pneumonia,
pulmonary edema,
fibrosis
APPLICATION OF ADVENTITIOUS LUNG SOUNDS
Respiratory system
signs of respiratory distress,
hyperinflation,
consolidation,
pleural effusion,
pneumothorax,
sup vena cava obstruction
Abnormality Initial
impression
Inspection Palpitation Percussion Ausculation Possible
causes
Acute airways
obstruction
Appears acutely
ill
Use of
accessory
muscles
Reduced
expansion
Increased
resonance
Expiratory
wheezing
Asthma,
bronchitis
Chronic airways
obstruction
Appears
chronically ill
Increased
antero-posterior
diameter, use of
accessory
muscles
Reduced
expansion
Increased
resonance
Diffuse reduction
in breath sounds;
early inspiratory
crackles
Chronic
bronchitis,
emphysema
Consolidation May appear
acutely ill
Inspiratory lag Increased
fremitus
Dull note Bronchial breath
sounds; crackles
Pneumonia,
tumor
Pneumothorax May appear
acutely ill
Unilateral
expansion
Decreased
fremitus
Increased
resonance
Absent breath
sounds
Rib fracture, open
wound
Pleural effusion May appear
acutely ill
Unilateral
expansion
Absent fremitus Dull note Absent breath
sounds
Congestive heart
failure
Local bronchial
obstruction
Appears acutely
ill
Unilateral
expansion
Absent fremitus Dull note Absent breath
sounds
Mucous plug
Diffuse intersitial
fibrosis
Often normal Rapid shallow
breathing
Often normal;
increased
fremitus
Slight decrease in
resonance
Late inspiratory
crackles
Chronic exposure
to inorganic dust
Acute upper
airway
obstruction
Appears acutely
ill
Laboured
breathing
Often normal Often normal Inspiratory or
expiratory stridor
or both
Epiglottitis,
croup, foreign
body aspiration
Functions of the lung
Respiration: ventilation and gas exchange
Non-respiratory functions:
synthesis, activation and inactivation of vasoactive
substances, hormones, neuropeptides, eicosanoids,
lipoprotein complexes.
Hemostatic functions
Lung defense: complement activation, leucocyte
recruitment, cytokines and growth factors
Lung sounds Possible mechanism Characteristics Causes
Wheezes
Rapid airflow through obstructed
airways caused by
bronchospasm, mucosal edema
High-pitched; most
often occur during
exhalation
Asthma, congestive heart
failure, bronchitis
Stridor
Rapid airflow through obstructed
airway caused by inflammation
High-pitched; often
occurs during
inhalation
Croup, epiglottitis,
postextubation
Crackles
I nsp & exp
Excess airway secretions moving
with airflow
Coarse and often clear
with cough
Bronchitis, respiratory
infections
Early insp
Sudden opening of proximal
bronchi
Scanty, transmitted to
mouth; not affected by
cough
Bronchitis, emphysema,
asthma
Late insp
Sudden opening of peripheral
airways
Diffuse, fine; occur
initially in dependent
regions
Atelectasis, pneumonia,
pulmonary edema,
fibrosis
APPLICATION OF ADVENTITIOUS LUNG SOUNDS
Abnormality Initial
impression
Inspection Palpitation Percussion Ausculation Possible
causes
Acute airways
obstruction
Appears acutely
ill
Use of
accessory
muscles
Reduced
expansion
Increased
resonance
Expiratory
wheezing
Asthma,
bronchitis
Chronic airways
obstruction
Appears
chronically ill
Increased
antero-posterior
diameter, use of
accessory
muscles
Reduced
expansion
Increased
resonance
Diffuse reduction
in breath sounds;
early inspiratory
crackles
Chronic
bronchitis,
emphysema
Consolidation May appear
acutely ill
Inspiratory lag Increased
fremitus
Dull note Bronchial breath
sounds; crackles
Pneumonia,
tumor
Pneumothorax May appear
acutely ill
Unilateral
expansion
Decreased
fremitus
Increased
resonance
Absent breath
sounds
Rib fracture, open
wound
Pleural effusion May appear
acutely ill
Unilateral
expansion
Absent fremitus Dull note Absent breath
sounds
Congestive heart
failure
Local bronchial
obstruction
Appears acutely
ill
Unilateral
expansion
Absent fremitus Dull note Absent breath
sounds
Mucous plug
Diffuse intersitial
fibrosis
Often normal Rapid shallow
breathing
Often normal;
increased
fremitus
Slight decrease in
resonance
Late inspiratory
crackles
Chronic exposure
to inorganic dust
Acute upper
airway
obstruction
Appears acutely
ill
Laboured
breathing
Often normal Often normal Inspiratory or
expiratory stridor
or both
Epiglottitis,
croup, foreign
body aspiration
Vous aimerez peut-être aussi
- Essential pediatric fluid and electrolyte formulas under 40 charactersDocument8 pagesEssential pediatric fluid and electrolyte formulas under 40 charactersQurrataini IbanezPas encore d'évaluation
- HydrocephalusDocument28 pagesHydrocephalusQurrataini Ibanez100% (1)
- CBC Parameters and QCDocument17 pagesCBC Parameters and QCQurrataini IbanezPas encore d'évaluation
- Chapter 17Document44 pagesChapter 17Qurrataini IbanezPas encore d'évaluation
- Grading of TonsilDocument3 pagesGrading of TonsilQurrataini IbanezPas encore d'évaluation
- CBC Parameters and QCDocument17 pagesCBC Parameters and QCQurrataini IbanezPas encore d'évaluation
- Grading of TonsilDocument3 pagesGrading of TonsilQurrataini IbanezPas encore d'évaluation
- Anxiety DisorderDocument62 pagesAnxiety DisorderQurrataini Ibanez100% (3)
- Pharma Local AnestheticsDocument1 pagePharma Local AnestheticsQurrataini IbanezPas encore d'évaluation
- Grading of TonsilDocument1 pageGrading of TonsilQurrataini IbanezPas encore d'évaluation
- Common Gynecologic Procedures ExplainedDocument55 pagesCommon Gynecologic Procedures ExplainedQurrataini IbanezPas encore d'évaluation
- Pharmacology IntroductionDocument5 pagesPharmacology IntroductionQurrataini IbanezPas encore d'évaluation
- Bleeding Time, Clotting Time PT and PTT2Document41 pagesBleeding Time, Clotting Time PT and PTT2Qurrataini Ibanez100% (1)
- Tetanus ImmunizationDocument11 pagesTetanus ImmunizationQurrataini IbanezPas encore d'évaluation
- HemostasisDocument40 pagesHemostasisQurrataini IbanezPas encore d'évaluation
- Chemotherapeutic Agents: Mechanisms of Action and ClassesDocument29 pagesChemotherapeutic Agents: Mechanisms of Action and ClassesQurrataini IbanezPas encore d'évaluation
- Pharmaco TherapeuticsDocument1 pagePharmaco TherapeuticsQurrataini IbanezPas encore d'évaluation
- Pediatrics Notes, SOAP, DischargeDocument5 pagesPediatrics Notes, SOAP, DischargeQurrataini IbanezPas encore d'évaluation
- 1 Hypersensitivity ReactionsDocument55 pages1 Hypersensitivity ReactionsQurrataini IbanezPas encore d'évaluation
- G6PD and SulfonamidesDocument1 pageG6PD and SulfonamidesQurrataini IbanezPas encore d'évaluation
- Chelation TherapyDocument2 pagesChelation TherapyQurrataini IbanezPas encore d'évaluation
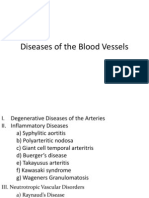
- Diseases of The Blood VesselsDocument40 pagesDiseases of The Blood VesselsQurrataini IbanezPas encore d'évaluation
- Introduction To Surgical PathologyDocument29 pagesIntroduction To Surgical PathologyQurrataini IbanezPas encore d'évaluation
- Anti ViralDocument17 pagesAnti ViralQurrataini IbanezPas encore d'évaluation
- Toxidromes and Antidotes SummaryDocument11 pagesToxidromes and Antidotes SummaryQurrataini IbanezPas encore d'évaluation
- Filming Guides ProjectDocument4 pagesFilming Guides ProjectQurrataini IbanezPas encore d'évaluation
- Breast CADocument15 pagesBreast CAQurrataini IbanezPas encore d'évaluation
- BSFCR Cardio Case Group 1Document23 pagesBSFCR Cardio Case Group 1Qurrataini IbanezPas encore d'évaluation
- Fungal Infections: Alma E. Malilong, MD, FPSPDocument33 pagesFungal Infections: Alma E. Malilong, MD, FPSPQurrataini IbanezPas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Respiratory System Assessment PDFDocument53 pagesRespiratory System Assessment PDFJay RomePas encore d'évaluation
- TEST Cardiovascular and Respiratory AssessmentDocument2 pagesTEST Cardiovascular and Respiratory AssessmentGabriel VelascoPas encore d'évaluation
- Assessment of Respiratory System for AnesthesiaDocument49 pagesAssessment of Respiratory System for AnesthesiaMilanisti22Pas encore d'évaluation
- Chest and Lungs ExaminationDocument75 pagesChest and Lungs Examinationdhainey100% (10)
- NGNTestPacket 110322Document64 pagesNGNTestPacket 110322romeliza romeliza0% (1)
- NEJM 2014 Fundamentals of Lung AuscultationDocument7 pagesNEJM 2014 Fundamentals of Lung AuscultationFelipe CeaPas encore d'évaluation
- Pulmonology Exam: Comprehensive Chest AssessmentDocument33 pagesPulmonology Exam: Comprehensive Chest AssessmentSagit Nauman81Pas encore d'évaluation
- Auscultation Landmarks PDFDocument17 pagesAuscultation Landmarks PDFYoga HanditaPas encore d'évaluation
- Assessment of the Respiratory SystemDocument20 pagesAssessment of the Respiratory SystemnadyaPas encore d'évaluation
- ncp-Nursing-Diagnosis - Ineffective - 510.htmlDocument2 pagesncp-Nursing-Diagnosis - Ineffective - 510.htmlrayearth_109368Pas encore d'évaluation
- Lung Sounds: Inasa Nabila 1810211113Document10 pagesLung Sounds: Inasa Nabila 1810211113Inasa NabilaPas encore d'évaluation
- Chapter 46 Chest AssessmentDocument12 pagesChapter 46 Chest Assessmentmj CanilangPas encore d'évaluation
- Lung Examination: AbnormalDocument56 pagesLung Examination: AbnormalBECAREFUL89APas encore d'évaluation
- Impaired Gas ExchangeDocument3 pagesImpaired Gas ExchangePaul VincentPas encore d'évaluation
- Respiratory Assessment Interview and Exam GuideDocument13 pagesRespiratory Assessment Interview and Exam GuideChristine LeePas encore d'évaluation
- Spring 2009 Intramural Indoor Soccer Teams: Tuesday Men's Carefree "A" 6:30PM - 8:30PMDocument28 pagesSpring 2009 Intramural Indoor Soccer Teams: Tuesday Men's Carefree "A" 6:30PM - 8:30PMapi-3700892Pas encore d'évaluation
- A4.Fundamentals - 25item With RationaleDocument4 pagesA4.Fundamentals - 25item With RationaleBlardy Falking You Benchod BlardyPas encore d'évaluation
- Respiratory System (Physical Examination)Document30 pagesRespiratory System (Physical Examination)Noor Ahmad AhadiPas encore d'évaluation
- ConsultsDocument16 pagesConsultsRaq KhoPas encore d'évaluation
- Unit 06 Assessment of Thorax and LungDocument55 pagesUnit 06 Assessment of Thorax and Lunghuma100% (1)
- Monterozo, Ronel Von O. Prime 4Document7 pagesMonterozo, Ronel Von O. Prime 4Ronel MonterozoPas encore d'évaluation
- Adventitious Breath SoundsDocument1 pageAdventitious Breath SoundsEdwin Delos Reyes AbuPas encore d'évaluation
- Nursing Care Plan for Infiltrative TB of the LungDocument6 pagesNursing Care Plan for Infiltrative TB of the LungMargarette Mae VillanuevaPas encore d'évaluation
- Breath Sounds Study GuideDocument28 pagesBreath Sounds Study GuideGustavo OlguinPas encore d'évaluation
- Opd Soap Format: For Follow Up PatientsDocument2 pagesOpd Soap Format: For Follow Up PatientsMicaPas encore d'évaluation
- Fijian University Pediatrics GuideDocument77 pagesFijian University Pediatrics GuideShariti DeviPas encore d'évaluation
- Abnormal Lung SoundsDocument6 pagesAbnormal Lung SoundsQuinn Madalang100% (1)
- Thorax and Lungs ReferenceDocument8 pagesThorax and Lungs Referencegwynth ripaldaPas encore d'évaluation
- Breath Sounds: ConsiderationsDocument10 pagesBreath Sounds: ConsiderationsKarl RoblePas encore d'évaluation
- Thorax, Skin, Hair, Nails ObjectivesDocument3 pagesThorax, Skin, Hair, Nails Objectivesctramel001100% (1)