Académique Documents
Professionnel Documents
Culture Documents
Lepra Reaction
Transféré par
ZLOOffice Bankura0 évaluation0% ont trouvé ce document utile (0 vote)
238 vues24 pageslepra reaction
Titre original
9. Lepra Reaction
Copyright
© © All Rights Reserved
Formats disponibles
PPT, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentlepra reaction
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PPT, PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
238 vues24 pagesLepra Reaction
Transféré par
ZLOOffice Bankuralepra reaction
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PPT, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 24
Lepra Reactions
It is acute inflammatory response
occurring in the course of the disease
1
This is thought to be due to an alteration in the immunological status
of the patient
It is the major cause of nerve damage and disability in leprosy
It can occur at anytime before, during or after treatment
Occurs in 3040% of leprosy cases.
Risk factors,-
Multiple lesions
Lesions close to peripheral nerve
Lesions on the face
Pregnancy / Postpartum period
Puberty
Alcohol intake
Principal types of Lepra reactions
1.Type 1 Lepra reaction also known as Reversal
reaction and may occur both in PB and MB
leprosy 2
2.Type 2 Lepra reaction also known as Erythema
Nodosum Leprosum an occurs only in MB leprosy
3.Lucio type II phenomenon--a type of cutaneous
vasculitis,tend to affect people not taken MDT
regularly.It presents as odd shaped red patches and
ulcers on hands,feet,wrist,ankle.It is associated
with fever,arthritis,liver,kidney diseases.
Type 1
Mechanism : antigens from broken bacilli react with T-
lymphocytes resulting in alteration of cell-mediated
immunity (Delayed hypersensitivity
Note : 3
reaction)
May occur all of a sudden and may be repeated
episodes
Existing patches become raised, erythematous and
edematous
Neuritis (silent or overt) with / without sudden onset of
muscle paralysis is a common feature
If the pain and tenderness is severe and if paralysis or
anesthesia threatens to follow the neuritis, reaction is
considered severe
New lesions may appear
Systematic complaints are uncommon
Necrosis and ulcerations are seen rarely in severe
reactions
Lepra reaction Type 1 (Reversal reaction)
Features Type 1 4
Existing lesions suddenly becomes
red, swollen, warm and tender. New
lesions may appear
Skin
Lesions when subsiding may show
scales
Nerves close to the skin may
Nerves become enlarged, tender and painful
(neuritis) with loss of nerve function
Other Organs Rarely affected
General Not common
Symptoms
Type 2
Mechanism : Circulating antibodies against M.leprae react with
the M.leprae antigens (Antigen-antibody reaction) 5
Note :
It may be intermittent or continuous
New erythematous, tender nodules
ENL appear in crops
Bilateral, symmetrical in distribution
Existing skin patches do not show any
change
ENLs may be ulcerated in severe
reaction
Swelling of joints with systematic
complaints like fever, chills are
common
Other organs e.g. nerve, muscle, bone,
eye, liver, testis, spleen may be
involved. D/D.
Lepra reaction Type 2 ( ENL reaction)
Features 6 Type 2
Red, painful, tender, subcutaneous
deep) nodules (ENL) appear
commonly on the face, arms and legs
Skin
They appear in groups and subside
within a few days even without
treatment
Nerves may be affected but not as
Nerves common or severe as in Type 1
Other organs like eyes, joints, bones,
Other testis, kidney may be affected
Organs
General Fever, joint pains, fatigue
Symptoms
Silent neuritis 7
Van Brakel and Khawas proposed the term
Silent Neuropathy (SN) to described the
phenomenon of Nerve function in patient
occurring in the absence of symptoms. It is
therefore only detected if Medical Officer
perform a careful examination of the
peripheral Nervous system otherwise it may
cause disability. Treatment is same as type
I reaction.
Treatment of Lepra reaction Type 1
I. If the reaction is mild with no nerve involvement the reaction can be controlled by rest
and analgesics (aspirin or paracetamol) (8)
II. If there are signs of severe reversal reaction then in addition to rest and analgesics
corticosteroids e.g. prednisolone is given. Rest to the affected Nerve using splint.
III. In both the cases MDT is to be continued.
Schedule for Prednisolone therapy for an adult patient Type 1
- 40 mg once a day for first 2 weeks then
- 30 mg once a day for weeks 3rd and 4th
- 20 mg once a day for weeks 5th and 6th
- 15 mg once a day for weeks 7th and 8th
- 10 mg once a day for weeks 9th and 10th
- 5 mg once a day for weeks 11th and 12th
[Daily dose should not exceed 1 mg per Kg body weight]
Note : For neuritis (involvement of peripheral nerve trunk) period of treatment prolonged
according to response each period would be for 4 weeks from 20 mg
Enquire for the following before starting steroids (precautions)
# Hypertension # Peptic ulcer # Tuberculosis #
Diabetes # Inter-current infections
Treatment of Lepra reaction (ENL) Type 2
I. If the reaction is mild with no nerve involvement and having few
nodules and mild fever the reaction can be controlled by rest and
analgesics (aspirin or paracetamol) (9)
II. If there are signs of ENL reaction then in addition to rest and
analgesics corticosteroids e.g. prednisolone is given
Drugs used in type II reaction :-
1. Prednisolone already mentioned.
2. Clofazimine therapy it is also effective for type II reaciton but less
potent then corticosteroid, 300 mg daily (max. 1 month) in three
divided doses and tappered gradually to 100mg daily, can be given
max. upto 12 months.
3. Thalidomide therapy 200 mg twice daily / 100 mg 4 times daily and
then gradually tapered off. Must be used cautiously.
4. Chloroquine 250mg 3 times daily for 1 week then 250mg 2 times daily
for 1 week then 250mg once daily for 1 week
Indications for referral 10
Failure to respond after 4 weeks of steroid treatment
Eye involvement
Other systemic involvement
Recurrent lepra reactions
Distinguishing Relapse from Reaction (11)
Criteria Relapse Reaction
Time since completion Usually more than 3 Usually less than 3
of treatment years years
Progression of signs & Slow Fast
symptoms
Site of lesions In new places Over old patches
Pain, tenderness or Usually No Usually Yes skin &
swelling nerves
Damage Occurs slowly Sudden onset
General condition Not affected Inflammation
Role of Medical Officer 12
Medical Officer should know to diagnose lepra reaction in
early stage
Medical Officer should know treatment of lepra reaction.
MDT should not be suspended during reactions
MDT significantly reduces the frequency and severity of
reactions
During counseling possible occurrence of reactions should be
explained since signs and symptoms of reactions could be
misunderstood as adverse effects of drugs
THANK YOU
DR. SWAPAN KUMAR SARKAR
ZONAL LEPROSY OFFICER
BANKURA
MDT should be continued without interruption
along with anti-reaction treatment in patients
taking MDT and MDT need not be started for
those having completed MDT
Review progress every two weeks
If treatment not responding same dose may be
continued for further two weeks (if not
responding even after four weeks or condition
worsening then refer)
In severe conditions rest is provided by applying
a padded splint / any suitable alternative material
to immobilize joints near affected nerves
Schedule for Prednisolone therapy for an adult
patient Type 2
Type 2 reaction Treatment
Mild few nodules, mild Analgesics
fever
Severe severe pain over Steroid Prednisolone whole
nodules, tendency for course not exceeding 2 to 3 weeks
ulceration, high fever, ( same dose as for Type 1 reactions
involvement of internal but tapering should be done fast
organs based on response )
Neuritis Prednisolone regimen as for
neuritis in Type 1
Iridocyclitis pain, redness Mild cases application of atropine
and watering of eyes and steroid eye drops/ointments
Severe referred to eye specialist
Clofazimine in the treatment of Type 2 Lepra reaction
Less potent than corticosteroids
Often takes 4-6 weeks to develop full effect
Should not be started as the sole agent for
treatment of Type 2 reaction
Useful for reducing or withdrawing corticosteroids
on corticosteroids dependant patients
Dose is 300 mg daily (max. of 1 month) given in
three divided doses to minimize gastro intestinal
side effects
Tapered to 100 mg daily
Total duration should not exceed 12 months
Response seen after 2-4 weeks of starting
Peripheral Level Signs indicating that a reaction
is severe and patient must referred
Red, painful, single or multiple nodules in the skin with / without
ulceration
Pain / tenderness in one / more nerves, with / without loss of
function
Silent neuritis nerve function impairment, without skin
inflammation
A red, swollen skin patch on the face, overlying another major
nerve trunk
A skin lesion that becomes ulcerated, or that is accompanied by
a high fever
Marked edema of hands, feet or face
Pain / redness of eyes, with / without loss of visual acuity
Painful swelling of joints with fever
[Reactions which show none of these signs of severity but limited
to mildly inflamed skin lesions may be treated symptomatically
with analgesics]
Assessment of patient previously treated for leprosy
Take full history of current problem including -
The duration of previous treatment and the onset of new
symptoms
Did new lesions appear quickly or over a long period ?
What is the relationship with the old skin patches ?
Has there been any pain, tenderness or swelling ?
Has there been any recent loss of function in any nerves ?
[ Carry out full examination of the skin and of
nerve function, in order to identify any signs of
a recent reaction ]
Key messages for persons completing treatment
successfully
If the person suspects the disease (relapse) has
returned, they should come for further examination if
leprosy reoccurs it can be treated
If any unusual (reactions) symptoms occur ( including
weakness, numbness or pain in the limbs, or loss of
vision or other eye problems ) the person should come
back for examination and treatment especially
important for MB patients
If some disability is already present the person should
know what they need to do at home to manage the
problem
Relapse
Def :The re-occurrence of the disease at any
time after the completion of a full course of
treatment
There is reappearance or increase in the number of lesions
In case of MB relapse confirmed by skin smear examination .
(If skin smear has been done at RFT then usually two log
increase is seen in bacteriological index BI (e.g. 1+ at RFT
and 3+ at recurrence)
Patients who start treatment with high BI are more likely to
suffer relapse later
Most relapse occur long after the treatment is given
sometimes over 10 years
Lepra reaction can also occur after RFT and can be
usually distinguished from relapse
In lepra reaction
a. time of onset usually within 3 years of RFT.
b. If there is signs of recent nerve damage a reaction is very
likely
c. its favorable response to steroid therapy
(A reaction may be treated with steroids while relapse
will not be greatly affected by a course of steroids, so
using steroids as a therapeutic trial can help clarify
thee diagnosis)
Treatment:
MB patients given another course of standard MDT
regimen for MB
PB patients should be treated with MDT regimen of PB
if the disease is PB but if MB is diagnosed at relapse
then a course of MDT regimen of MB
Cell Mediated Immunity Humoral Antibodies
Is the reaction to the protein of the Humoral antibodies appear in
organism physiologically response to polysaccharide fraction of
capable of altering the histiocytes organism macrophages not
to improve their capacity to lyse influenced and organisms multiply in it
bacteria
1 Localized, well defined, Extensive, diffuse poorly delimited
circumscribed lesion lesions
2 Few bacilli demonstrated Myriads of bacilli
Intense macrophage (epitheloid) Abundant macrophage (foam cell)
3 cell response effective response with efficient phagocytosis
phagocytosis and disposal of but ineffectual disposal of bacilli
bacilli
4 Lepromin +ve Lepromin -ve
5 Granulomatous inflammation True granuloma absent
Cell Mediated Immunity Humoral Antibodies
6 Circulation (humoral) Humoral antibodies readily
antibodies insignificant demonstrable
7 Immunological reactional Immunological reactions
exacerbation characterized exacerbation (ENL)
primarily by reactions of characterized primarily by
cellular hypersensitivity reactions of immediate type
(anaphylactoid) hypersensitivity
8 Effective accelerated Sluggish therapeutic response
therapeutic response
Vous aimerez peut-être aussi
- Drug Allergy BookDocument332 pagesDrug Allergy Bookmegah_asia13Pas encore d'évaluation
- MELANOMA: Risk Factors, Diagnosis, Staging and TreatmentDocument25 pagesMELANOMA: Risk Factors, Diagnosis, Staging and TreatmentFazaKhilwanAmnaPas encore d'évaluation
- Leprosy Reaction: Oleh: Aryo Wibowo C11103224 Pembimbing: Dr. Cyntia Yulyana Supervisor: Dr. Muhlis, SP - KK, M.KesDocument14 pagesLeprosy Reaction: Oleh: Aryo Wibowo C11103224 Pembimbing: Dr. Cyntia Yulyana Supervisor: Dr. Muhlis, SP - KK, M.Kesjoe ashikawaPas encore d'évaluation
- Dermatomyositis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsD'EverandDermatomyositis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsPas encore d'évaluation
- Psoriasis Comorbidities ReviewDocument8 pagesPsoriasis Comorbidities ReviewIvanWinardyPas encore d'évaluation
- UrticariaDocument12 pagesUrticarialilyrbrtPas encore d'évaluation
- Hisham Hussein Mohamed Ahmed - Gynaecomastia Paper Dr. AymanDocument14 pagesHisham Hussein Mohamed Ahmed - Gynaecomastia Paper Dr. Aymanhoremheb1100% (1)
- Version 3.0, 04/2013: Summary of Product Characteristics, Labelling and Package LeafletDocument12 pagesVersion 3.0, 04/2013: Summary of Product Characteristics, Labelling and Package Leafletkhangsiean89Pas encore d'évaluation
- Leprosy LecDocument26 pagesLeprosy LecAL Babaran CanceranPas encore d'évaluation
- Mattress SuturesDocument2 pagesMattress SuturesIo DobriPas encore d'évaluation
- Everything You Need to Know About PsoriasisDocument40 pagesEverything You Need to Know About PsoriasisAmrit Preet KaurPas encore d'évaluation
- Acne Vulgaris: Nelson P. Tandayu 0 9 - 1 0 0Document39 pagesAcne Vulgaris: Nelson P. Tandayu 0 9 - 1 0 0ntandayuPas encore d'évaluation
- Steroid Pulse Therapies in DermatologyDocument4 pagesSteroid Pulse Therapies in DermatologyWelly WijayantiPas encore d'évaluation
- Anti-Fungal Drugs Guide for Mycosis TreatmentDocument6 pagesAnti-Fungal Drugs Guide for Mycosis Treatmentbilal ahmadPas encore d'évaluation
- Cutaneous Leishmaniasis: A Case StudyDocument7 pagesCutaneous Leishmaniasis: A Case StudyIJAR JOURNALPas encore d'évaluation
- Eczema and DermatitisDocument43 pagesEczema and DermatitisArvinth Guna SegaranPas encore d'évaluation
- Acne Vulgaris (Or Acne) Is A CommonDocument21 pagesAcne Vulgaris (Or Acne) Is A CommonNia YuniarPas encore d'évaluation
- Skin Cancer!Document8 pagesSkin Cancer!HudiansyahPas encore d'évaluation
- PsoriasisDocument61 pagesPsoriasisWilliam WongPas encore d'évaluation
- Topical AntifungalsDocument14 pagesTopical AntifungalsRasha Mohammad100% (1)
- IKD6 - Contrast Associated AKIDocument44 pagesIKD6 - Contrast Associated AKIRenal Association MauritiusPas encore d'évaluation
- An Approach To The Patient With ErythrodermaDocument42 pagesAn Approach To The Patient With ErythrodermaShakilPas encore d'évaluation
- Viral Warts (Verrucae) : College of Medicine Name: Qasim Hussain AL-Haleimi AC:207002113Document18 pagesViral Warts (Verrucae) : College of Medicine Name: Qasim Hussain AL-Haleimi AC:207002113Qasim HaleimiPas encore d'évaluation
- Cutaneous Leishmaniasis: Caused by A Protozoa Called Leishmania PathogenesisDocument30 pagesCutaneous Leishmaniasis: Caused by A Protozoa Called Leishmania PathogenesisHudh HudPas encore d'évaluation
- Eczema and Nummular Dermatitis GuideDocument91 pagesEczema and Nummular Dermatitis GuideJhost Clinton PurbaPas encore d'évaluation
- Dermatitis Atopic Presentation (Prof - Harijono)Document38 pagesDermatitis Atopic Presentation (Prof - Harijono)Yovan PrakosaPas encore d'évaluation
- Dermaroller FaqsDocument9 pagesDermaroller Faqsjp516Pas encore d'évaluation
- Dermatomyositis: A Guide to Clinical Features, Diagnosis and ManagementDocument26 pagesDermatomyositis: A Guide to Clinical Features, Diagnosis and Managementzaki100% (1)
- Dms146 Slide DermatitisDocument65 pagesDms146 Slide DermatitisAdhitya Rama Jr.Pas encore d'évaluation
- Stevens-Johnson SyndromeDocument6 pagesStevens-Johnson SyndromeLau ColastrePas encore d'évaluation
- Eczema Types, Causes, and Management in 40 CharactersDocument56 pagesEczema Types, Causes, and Management in 40 CharactersAdam AriwibawaPas encore d'évaluation
- Lupus EritematousDocument27 pagesLupus EritematousNazwa Warda Amalia100% (2)
- VERUCCA VULGARIS PresentationDocument28 pagesVERUCCA VULGARIS PresentationBrilliantIbnuSina100% (2)
- Paraneoplastic DermatosesDocument57 pagesParaneoplastic DermatosesMohamed Riyaz100% (1)
- Sclerotherapy Information and Consent FormDocument3 pagesSclerotherapy Information and Consent FormDaniel DePrince IIIPas encore d'évaluation
- PediatricsDocument38 pagesPediatricskhanPas encore d'évaluation
- SkinDocument26 pagesSkinMario Baemamenteng100% (1)
- Tetanus RabiesDocument67 pagesTetanus RabiesWaNda GrPas encore d'évaluation
- Skin CancerDocument112 pagesSkin CancerLampd PilPas encore d'évaluation
- My Cancrum OrisDocument22 pagesMy Cancrum OrisSoyebo Alegría OluseyePas encore d'évaluation
- Alopecia AreataDocument71 pagesAlopecia AreatadrbhaveshpPas encore d'évaluation
- Antifungal Drugs: Activity No. 7Document16 pagesAntifungal Drugs: Activity No. 7Junah SeninaPas encore d'évaluation
- Birthmarks Identificationandmx201205ryanDocument4 pagesBirthmarks Identificationandmx201205ryanDanielcc LeePas encore d'évaluation
- Hemodiafiltration Principles and Advantages Over Conventional HD PDFDocument40 pagesHemodiafiltration Principles and Advantages Over Conventional HD PDFsajna CPas encore d'évaluation
- LeprosyDocument26 pagesLeprosyFamous manPas encore d'évaluation
- Atopic DermatitisDocument10 pagesAtopic DermatitisIboy ZulhamPas encore d'évaluation
- NemaoDocument94 pagesNemaoRoxenette Gil Bernales PangilinanPas encore d'évaluation
- Bab I Pendahuluan 1.1 Latar Belakang: Case Report Session Ini Disusun Untuk Memenuhi Tugas Kepaniteraan KlinikDocument33 pagesBab I Pendahuluan 1.1 Latar Belakang: Case Report Session Ini Disusun Untuk Memenuhi Tugas Kepaniteraan KlinikNurifnaPas encore d'évaluation
- Chapter 11Document23 pagesChapter 11Hannah BuquironPas encore d'évaluation
- Introduction To Dermatology Assessment of A Dermatologic PatientDocument86 pagesIntroduction To Dermatology Assessment of A Dermatologic PatientAtifPas encore d'évaluation
- Antifungal AgentsDocument37 pagesAntifungal AgentsChandrashekhar UnakalPas encore d'évaluation
- WILMs TumorDocument3 pagesWILMs TumorLorie May GuillangPas encore d'évaluation
- DddsDocument50 pagesDddsOsama AlhasePas encore d'évaluation
- Acute Leukemia Types and TreatmentDocument22 pagesAcute Leukemia Types and TreatmentFelix Allen100% (1)
- JIA Eye Risks and TreatmentsDocument5 pagesJIA Eye Risks and TreatmentsDyan Friska Yanty LbsPas encore d'évaluation
- Antifungal Drugs 3Document54 pagesAntifungal Drugs 3Mikee MeladPas encore d'évaluation
- Psoriasis and Comorbid DeseaseDocument67 pagesPsoriasis and Comorbid DeseaseAl NaifPas encore d'évaluation
- Scabies RijiDocument29 pagesScabies RijirijivincentPas encore d'évaluation
- Approach To Photosensitivity - DR Pankaj AIIMS, New DelhiDocument80 pagesApproach To Photosensitivity - DR Pankaj AIIMS, New DelhiDr Pankaj Chaturvedi100% (4)
- Updated Operational Guidelines For Mission IndradhanushDocument76 pagesUpdated Operational Guidelines For Mission IndradhanushZLOOffice BankuraPas encore d'évaluation
- 1 Indradhanush Card 2nd ProofDocument2 pages1 Indradhanush Card 2nd ProofZLOOffice BankuraPas encore d'évaluation
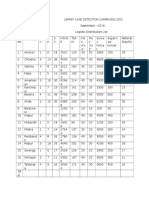
- Logistic DistributionDocument2 pagesLogistic DistributionZLOOffice BankuraPas encore d'évaluation
- World Population FortnightDocument3 pagesWorld Population FortnightZLOOffice BankuraPas encore d'évaluation
- Mock Exam 2Document33 pagesMock Exam 2Althea Karmylle M. BonitaPas encore d'évaluation
- MF 04Document21 pagesMF 04Carlos De la CruzPas encore d'évaluation
- Forms and Types of Business OrganizationDocument2 pagesForms and Types of Business Organizationjune hetrePas encore d'évaluation
- 6 - English-How I Taught My Grandmother To Read and Grammar-Notes&VLDocument11 pages6 - English-How I Taught My Grandmother To Read and Grammar-Notes&VLManav100% (2)
- Design of Efficient Serial Divider Using HAN CARLSON AdderDocument3 pagesDesign of Efficient Serial Divider Using HAN CARLSON AdderInternational Journal of Innovative Science and Research TechnologyPas encore d'évaluation
- CQI - Channel Quality Indicator - Ytd2525Document4 pagesCQI - Channel Quality Indicator - Ytd2525TonzayPas encore d'évaluation
- Life Convict Laxman Naskar Vs State of West Bengal & Anr On 1 September, 2000Document6 pagesLife Convict Laxman Naskar Vs State of West Bengal & Anr On 1 September, 2000Kimberly HardyPas encore d'évaluation
- Ch.24.2 Animal Evolution and DiversityDocument34 pagesCh.24.2 Animal Evolution and DiversityweldeenytPas encore d'évaluation
- The Sims FreeplayDocument14 pagesThe Sims FreeplayFlorianPas encore d'évaluation
- ArenavirusDocument29 pagesArenavirusRamirez GiovarPas encore d'évaluation
- Module 2 - Content and Contextual Analysis of Selected Primary andDocument41 pagesModule 2 - Content and Contextual Analysis of Selected Primary andAngelica CaldeoPas encore d'évaluation
- Comparative Ethnographies: State and Its MarginsDocument31 pagesComparative Ethnographies: State and Its MarginsJuan ManuelPas encore d'évaluation
- Mr. Honey's Large Business DictionaryEnglish-German by Honig, WinfriedDocument538 pagesMr. Honey's Large Business DictionaryEnglish-German by Honig, WinfriedGutenberg.orgPas encore d'évaluation
- ADSL Line Driver Design Guide, Part 2Document10 pagesADSL Line Driver Design Guide, Part 2domingohPas encore d'évaluation
- Ehlers-Danlos Syndromes (EDS) : Fiona Li Pharm D Candidate University of Saint Joseph School of PharmacyDocument22 pagesEhlers-Danlos Syndromes (EDS) : Fiona Li Pharm D Candidate University of Saint Joseph School of PharmacyDiogo CapellaPas encore d'évaluation
- Di OutlineDocument81 pagesDi OutlineRobert E. BrannPas encore d'évaluation
- Financial MarketsDocument323 pagesFinancial MarketsSetu Ahuja100% (2)
- The Other Side of Love AutosavedDocument17 pagesThe Other Side of Love AutosavedPatrick EdrosoloPas encore d'évaluation
- ViscosityDocument7 pagesViscositykiran2381Pas encore d'évaluation
- German composer known for political worksDocument4 pagesGerman composer known for political worksGeorge PikPas encore d'évaluation
- Chapter 10 HandoutDocument18 pagesChapter 10 HandoutChad FerninPas encore d'évaluation
- 2200SRM0724 (04 2005) Us en PDFDocument98 pages2200SRM0724 (04 2005) Us en PDFMayerson AlmaoPas encore d'évaluation
- Functional Appliances 2018Document45 pagesFunctional Appliances 2018tonhanrhmPas encore d'évaluation
- 17 Lagrange's TheoremDocument6 pages17 Lagrange's TheoremRomeo Jay PragachaPas encore d'évaluation
- INTRODUCTION Quali Observation ReportDocument2 pagesINTRODUCTION Quali Observation Reportmira hamzahPas encore d'évaluation
- Henderson - Historical Documents of The Middle AgesDocument536 pagesHenderson - Historical Documents of The Middle AgesVlad VieriuPas encore d'évaluation
- BCOM 302 BookDocument179 pagesBCOM 302 BookHitanshi AgarwalPas encore d'évaluation
- Philosophical Perspectives Through the AgesDocument13 pagesPhilosophical Perspectives Through the Agesshashankmay18Pas encore d'évaluation
- Ns5e rw3 SB Ak HyeDocument24 pagesNs5e rw3 SB Ak HyeKeys Shield JoshuaPas encore d'évaluation
- Pin Block Formats Explained in DetailDocument3 pagesPin Block Formats Explained in DetailJinay SanganiPas encore d'évaluation