Académique Documents
Professionnel Documents
Culture Documents
Glomerular Disease: Acute Nephritic Syndrome, Nephrotic Syndrome, and Chronic Glomerulonephritis
Transféré par
iron0 évaluation0% ont trouvé ce document utile (0 vote)
26 vues18 pagesGD
Titre original
Glomerular Disease
Copyright
© © All Rights Reserved
Formats disponibles
PPTX, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentGD
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PPTX, PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
26 vues18 pagesGlomerular Disease: Acute Nephritic Syndrome, Nephrotic Syndrome, and Chronic Glomerulonephritis
Transféré par
ironGD
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PPTX, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 18
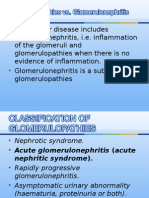
GLOMERULAR DISEASE
ACUTE NEPHRITIC SYNDROME
NEPHROTIC SYNDROME
CHRONIC GLOMERULONEPHRITIS
GLOMERULAR DISEASE
Glomerular
ACUTE NEPHRITIC SYNDROME
It reflects an acute inflammatory
response w/in the kidney & is
characterized in the urine sediment
by:
Hematuria
RBC casts
Other signs of acute inflammatory
renal injury:
proteinuria
peripheral edema
hypertension, or
renal insufficiency w/ or w/out oliguria
Pathophysiology
Pathophysiology
The hallmark of the acute nephritic syndrome is the finding
of RBCs and RBC (as well as other) casts in the urine
sediment
The finding of RBC casts in a patient w/ hematuria virtually
ensures that the patient has a glomerular pathologic process
The severity of these abnormalities also varies, since hematuria
can be either microscopic or grossly visible.
The urinary findings in acute glomerular disease vary,
ranging from normal (usu. seen in subclinical disease) to
signs of proteinuria, hematuria, pyuria, lipiduria, & RBC &
other casts
The degree of proteinuria can range from just above the upper
limit of normal to the nephrotic range
Pathophysiology
The manner in w/c RBCs pass into the urine in
glomerular dse probably due to focal disruptions in the
glomerular capillary wall produced by the underlying
inflammatory process
These focal disruptions along the glomerular capillary
wall may contribute to proteinuria & may allow plasma
proteins larger than albumin to escape into the urine
Pathophysiology
Renal Na & water retention resulting in generalized edema
is common because of poor renal perfusion stemming from
a decline in renal blood flow & proteinuria
Resulting hypoalbuminemia & a decline in intravascular
volume
Elevated blood pressure is an additional common clinical
component.
Both volume overload from inappropriate renal fluid
retention & enhanced renin secretion from renal injury &
resulting vasoconstrictor tone play important roles in this
process.
Pathophysiology
The GFR is often reduced resulting in a rise in blood
urea nitrogen
This reduction is a result of declines in:
glomerular blood flow, glomerular transcapillary hydraulic
pressure gradients, & the glomerular permeability coefficient,
w/c is a function of both porosity and surface area available for
filtration of the glomerular capillary.
Pathophysiology
Often in this syndrome, renal insufficiency is
transient, but it also can be progressive, leading to
chronic glomerulonephritis & renal failure.
Most patients w/ acute nephritis have a form of
proliferative glomerulonephritis &, occasionally, acute
tubulointerstitial nephritis
for this reason, renal biopsy is generally performed to
determine the final diagnosis.
Causes
Postreptococcal
NEPHROTIC SYNDROME
The manifestations of the nephrotic syndrome
include:
Massive proteinuria, w/ the daily loss of 3.5 gm or more
of protein (less in children)
Hypoalbuminemia, w/ plasma albumin levels <3 gm/dL
Generalized edema
Hyperlipidemia & lipiduria
Pathophysiology
The various components of nephrotic syndrome bear a
logical relationship to one another
The initial event is proteinuria
Proteinuria is due to an increase in glomerular
permeability of serum alb. & arises in response to
alterations in both the size & charge barriers of the
glomerular filtration apparatus
As a consequence of proteinuria, the serum alb. conc. &
therefore the plasma oncotic pressure fall.
Pathophysiology
The generalized edematous state common to the
nephrotic syndrome
Largely caused by this drop in plasma oncotic pressure &
the movement of fluid from the vascular to the
interstitial fluid compartment
producing a decline in plasma volume that signals the kidney
to retain Na & water
Pathophysiology
Most patients have:
Increased blood levels of cholesterol, TG, VLDL, LDL, Lp(a) lipoprotein,
& apoprotein
Decrease in HDL conc. in some patients.
These defects seem to be due in part to:
Increased synthesis of lipoproteins in the liver, abnormal transport of
circulating lipid particles
Decreased catabolism
Lipiduria follows the hyperlipidemia because not only albumin
molecules but also lipoproteins leak across the glomerular capillary wall.
The lipid appears in the urine either as free fat or as oval fat bodies,
representing lipoprotein resorbed by tubular epithelial cells & then shed
along w/ the degenerated cells.
Pathophysiology
These patients are particularly vulnerable to infection
Especially w/ staphylococci & pneumococci
This vulnerability could be related to loss of Igs or LMW
complement components in the urine
Thrombotic & thromboembolic complications are
common due to loss of anticoagulant factors (e.g.,
antithrombin III) & antiplasmin activity through the
leaky glomerulus
Renal vein thrombosis, once thought to be a cause of
nephrotic syndrome, is most often a consequence of this
hypercoagulable state
Causes
The relative frequencies of the several causes of the
nephrotic syndrome vary according to age and
geography
In children younger than 17 years in North America,
the nephrotic syndrome is almost always caused by a
lesion primary to the kidney
whereas among adults, it may often be associated w/ a
systemic disease
Causes
Approximate prevalence of primary disease = 95% in children, 60% in adults.
Approximate prevalence of systemic disease = 5% in children, 40% in adults
CHRONIC GLOMERULONEPHRITIS
Many forms of glomerular disease can progress to chronic
renal failure.
On morphologic examination, this progression is
characterized by scarring of most of the glomeruli.
UA results are more benign, w/ less proteinuria &
hematuria & w/ broad, waxy casts in the urine sediment
Occasionally, the urine may have characteristics of
nephritic, nephrotic, and chronic patterns.
This urinary finding has been called a telescoped sediment
and is usually seen in severe glomerulonephritis or
vasculitis.
Vous aimerez peut-être aussi
- Glomerular DiseaseDocument18 pagesGlomerular DiseaseironPas encore d'évaluation
- Nephrotic Syndrome-1Document21 pagesNephrotic Syndrome-1Wondimu EliasPas encore d'évaluation
- Glomerulonefritis Akut Dan Kronis: DR - Hasan Basri, Sppd-Kgh-FinasimDocument53 pagesGlomerulonefritis Akut Dan Kronis: DR - Hasan Basri, Sppd-Kgh-FinasimnadddPas encore d'évaluation
- Lecture Note On Renal Diseases For Medical Students - Nephrotic SyndromeDocument8 pagesLecture Note On Renal Diseases For Medical Students - Nephrotic SyndromeEsayas KebedePas encore d'évaluation
- AUBF Group 1 Chapter 8Document12 pagesAUBF Group 1 Chapter 8Gerald John PazPas encore d'évaluation
- Nephrotic SyndromeDocument65 pagesNephrotic SyndromemejulPas encore d'évaluation
- Lec6.nephrotic SyndromeDocument24 pagesLec6.nephrotic SyndromeMAD Bl00DPas encore d'évaluation
- SNDocument7 pagesSNArdy Syahabuddin GofarPas encore d'évaluation
- Glomerulonephritis vs GlomerulopathiesDocument58 pagesGlomerulonephritis vs GlomerulopathiesRahmailla Khanza Diana FebriliantriPas encore d'évaluation
- GlomerulonephritisDocument59 pagesGlomerulonephritistressPas encore d'évaluation
- Gus156 Slide Ginjal Dan Saluran KemihDocument128 pagesGus156 Slide Ginjal Dan Saluran KemihRina ChairunnisaPas encore d'évaluation
- Nephrotic Vs Nephritic SyndromeDocument80 pagesNephrotic Vs Nephritic Syndromevan016_bunnyPas encore d'évaluation
- Sindrom NefrotikDocument22 pagesSindrom NefrotikGyta Apriati100% (1)
- Glomerular Disorders - Part I & Part II (ARI NOTES)Document144 pagesGlomerular Disorders - Part I & Part II (ARI NOTES)Laiba FatimaPas encore d'évaluation
- Glo Me Rulo NefritisDocument58 pagesGlo Me Rulo NefritisFany SholehaPas encore d'évaluation
- Kidney DiseasesDocument22 pagesKidney Diseasesphoto copyhemnPas encore d'évaluation
- Nephrotic Syndrome: BackgroundDocument25 pagesNephrotic Syndrome: BackgroundsDamnPas encore d'évaluation
- Nefrotic Syndrome: Diagnostic Criteria For Nephrotic SyndromeDocument3 pagesNefrotic Syndrome: Diagnostic Criteria For Nephrotic SyndromeIntanAsriSarasatiPas encore d'évaluation
- 2 Glomerular DiseasesDocument48 pages2 Glomerular DiseasesDammaqsaa W BiyyanaaPas encore d'évaluation
- Glomerular Diseases-Part 1Document68 pagesGlomerular Diseases-Part 1hrg79qzwc2Pas encore d'évaluation
- Nephrotic Syndrome - Armando HasudunganDocument18 pagesNephrotic Syndrome - Armando HasudunganzahraaPas encore d'évaluation
- +acute GlomerulonephritisDocument19 pages+acute GlomerulonephritisDr. SAMPas encore d'évaluation
- Glomerular DsDocument18 pagesGlomerular Dsnathan asfahaPas encore d'évaluation
- 3&4 Glomerular Diseases and Nephrotic SyndromeDocument46 pages3&4 Glomerular Diseases and Nephrotic SyndromeTor Koang ThorPas encore d'évaluation
- Lo OjiDocument7 pagesLo OjiJosephine Grace SuryadiPas encore d'évaluation
- Glomerular Diseases: DR Rashmi NazarethDocument49 pagesGlomerular Diseases: DR Rashmi NazarethRohit RajeevanPas encore d'évaluation
- Nephrotic Syndrome Guide: Causes, Symptoms & TreatmentDocument17 pagesNephrotic Syndrome Guide: Causes, Symptoms & TreatmentERICKPas encore d'évaluation
- Glomerular Diseases and The Nephrotic SyndromeDocument67 pagesGlomerular Diseases and The Nephrotic SyndromeMatyie SmkasPas encore d'évaluation
- Nephrotic SyndromeDocument29 pagesNephrotic SyndromeMusthafa Afif WardhanaPas encore d'évaluation
- Nephrotic Syndrome Is A Collection of Symptoms Due To: Citation NeededDocument6 pagesNephrotic Syndrome Is A Collection of Symptoms Due To: Citation Neededrubie ann tillorPas encore d'évaluation
- The Urinary System: Dr. Khan, MD, MCPS, DTCD PA 5402 T/W/RDocument35 pagesThe Urinary System: Dr. Khan, MD, MCPS, DTCD PA 5402 T/W/RCrystal Lynn Keener SciariniPas encore d'évaluation
- Nephritic Syndrome - Armando HasudunganDocument14 pagesNephritic Syndrome - Armando HasudunganzahraaPas encore d'évaluation
- Nephrotic Syndrome: By: Yeni Ayu Prihastuti Moderator: DR. Dr. Hani Susianti, SP - PK (K)Document42 pagesNephrotic Syndrome: By: Yeni Ayu Prihastuti Moderator: DR. Dr. Hani Susianti, SP - PK (K)yeniPas encore d'évaluation
- crf03 1Document16 pagescrf03 1Aswin DamodaranPas encore d'évaluation
- Glomer Ds TadDocument190 pagesGlomer Ds TadHaileprince MekonnenPas encore d'évaluation
- By Mohd Hafiz SumsusdinDocument17 pagesBy Mohd Hafiz SumsusdinMohd Hafiz SumsusdinPas encore d'évaluation
- Kidney Pathophysiology 2023Document19 pagesKidney Pathophysiology 2023Xerox and CompService Xerox and CompServicePas encore d'évaluation
- Emergent Management of Acute Glomerulonephritis - Overview, Emergency Department Care, ConsultationsDocument4 pagesEmergent Management of Acute Glomerulonephritis - Overview, Emergency Department Care, ConsultationsHafiz Maulana AhmadPas encore d'évaluation
- Nephritic Syndrome: Pyuza, MDDocument41 pagesNephritic Syndrome: Pyuza, MDawadh mbaroukPas encore d'évaluation
- Nephrotic SyndromeDocument43 pagesNephrotic SyndromegopscharanPas encore d'évaluation
- Nephrotic Syndrome GuideDocument12 pagesNephrotic Syndrome GuidePutra Fatkhul Rizqi QoroidPas encore d'évaluation
- Glomerular Disease Types and PresentationsDocument58 pagesGlomerular Disease Types and PresentationsJosa Anggi Pratama0% (1)
- Wa0011.Document180 pagesWa0011.Mohamed AbdelmoniemPas encore d'évaluation
- Nephrotic and Nephritic Syndrome: Med5010 LectureDocument65 pagesNephrotic and Nephritic Syndrome: Med5010 LectureFreeburn Simunchembu100% (1)
- +nephrotic SyndromeDocument22 pages+nephrotic SyndromeDr. SAMPas encore d'évaluation
- Clinicopath Correlation of Renal DiseasesDocument7 pagesClinicopath Correlation of Renal DiseasesDeshan AdikariPas encore d'évaluation
- Chronic Kidney Disease. GolwallaDocument8 pagesChronic Kidney Disease. GolwallaAbdul QuyyumPas encore d'évaluation
- Red Flags in Pedia NephrDocument46 pagesRed Flags in Pedia NephrDoaa YoussefPas encore d'évaluation
- Lecture 4 (1of3) - Nephritic SyndromeDocument45 pagesLecture 4 (1of3) - Nephritic SyndromeAliye BaramPas encore d'évaluation
- Understanding Haemolytic Anaemia and Sickle Cell DiseaseDocument26 pagesUnderstanding Haemolytic Anaemia and Sickle Cell DiseaseGideon HaburaPas encore d'évaluation
- 22 - Proteinuria and HematuriaDocument73 pages22 - Proteinuria and HematuriaArsalan NadeemPas encore d'évaluation
- Approach To HematuriaDocument45 pagesApproach To HematuriaArun GeorgePas encore d'évaluation
- Seminar On Nephrotic Syndrome: Medical Surgical NursingDocument15 pagesSeminar On Nephrotic Syndrome: Medical Surgical NursingGargi MP100% (1)
- Management: DiagnosisDocument6 pagesManagement: DiagnosisAhmed El-MalkyPas encore d'évaluation
- Clinical Manifestations and Diagnosis of RhabdomyolysisDocument5 pagesClinical Manifestations and Diagnosis of RhabdomyolysisemirkurtalicPas encore d'évaluation
- Renal Failure and Kidney DiseaseDocument41 pagesRenal Failure and Kidney Disease12046Pas encore d'évaluation
- Glomerular Disorders - GlomerulonephrtisDocument56 pagesGlomerular Disorders - GlomerulonephrtisValerie Suge-MichiekaPas encore d'évaluation
- Narrative Pathophysiology of Nephrotic SyndromeDocument1 pageNarrative Pathophysiology of Nephrotic SyndromeNicaMariannePañaPas encore d'évaluation
- Practical Hemostasis and ThrombosisD'EverandPractical Hemostasis and ThrombosisNigel S. KeyPas encore d'évaluation
- Treatment Viral MeningitisDocument9 pagesTreatment Viral MeningitisironPas encore d'évaluation
- SOP 36 Pemeriksaan Urine LengkapDocument3 pagesSOP 36 Pemeriksaan Urine LengkapSevy AyuayuPas encore d'évaluation
- TREATMENT Bacterial MeningitisDocument32 pagesTREATMENT Bacterial MeningitisironPas encore d'évaluation
- PregnacyDocument12 pagesPregnacyironPas encore d'évaluation
- Frequent Urination Case StudyDocument13 pagesFrequent Urination Case StudyironPas encore d'évaluation
- Pathophysiology of SeizuresDocument11 pagesPathophysiology of SeizuresironPas encore d'évaluation
- Nephrogenic Diabetes Insipidus (Includes: Nephrogenic Diabetes Insipidus, Autosomal Nephrogenic Diabetes Insipidus, X-Linked)Document18 pagesNephrogenic Diabetes Insipidus (Includes: Nephrogenic Diabetes Insipidus, Autosomal Nephrogenic Diabetes Insipidus, X-Linked)ironPas encore d'évaluation
- Diabetes MellitusDocument32 pagesDiabetes Mellitusiron100% (1)
- Type 1 Diabetes Mellitus: TreatmentDocument25 pagesType 1 Diabetes Mellitus: TreatmentironPas encore d'évaluation
- DM Labs TherapDocument54 pagesDM Labs TherapironPas encore d'évaluation
- DIABETES EXCHANGE LISTSDocument10 pagesDIABETES EXCHANGE LISTSironPas encore d'évaluation
- Chronic Complications of Diabetes MellitusDocument40 pagesChronic Complications of Diabetes MellitusironPas encore d'évaluation
- Acute Complication of DM: Clinical Manifestation Laboratory Procedures Therapeutic Plan Possible Problem AssociatedDocument12 pagesAcute Complication of DM: Clinical Manifestation Laboratory Procedures Therapeutic Plan Possible Problem AssociatedironPas encore d'évaluation
- Weight, height, BMI and calorie needsDocument4 pagesWeight, height, BMI and calorie needsironPas encore d'évaluation
- Case #3 (Macazo, Manueke, Purba) : CBC ResultsDocument2 pagesCase #3 (Macazo, Manueke, Purba) : CBC ResultsironPas encore d'évaluation
- Comprehensive assessment and management plan for type 1 diabetesDocument37 pagesComprehensive assessment and management plan for type 1 diabetesironPas encore d'évaluation
- Managing Diabetes ComplicationsDocument35 pagesManaging Diabetes ComplicationsironPas encore d'évaluation
- Etiopathogenesis of Diabetes MellitusDocument35 pagesEtiopathogenesis of Diabetes MellitusironPas encore d'évaluation
- Interpretation of Laboratory Tests: CBC Chest X-Ray ABG Sputum GsDocument5 pagesInterpretation of Laboratory Tests: CBC Chest X-Ray ABG Sputum GsironPas encore d'évaluation
- Pancreas: - Anatomy and Histology - Normal Physiology of The Endocrine PancreasDocument34 pagesPancreas: - Anatomy and Histology - Normal Physiology of The Endocrine PancreasironPas encore d'évaluation
- Pharmacological treatment for type 1 and type 2 diabetes mellitusDocument26 pagesPharmacological treatment for type 1 and type 2 diabetes mellitusiron100% (1)
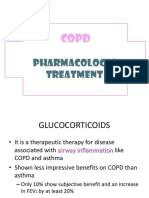
- COPD Treatment with Inhaled GlucocorticoidsDocument9 pagesCOPD Treatment with Inhaled GlucocorticoidsironPas encore d'évaluation
- Mechanisms of Cough From AngiotensinDocument1 pageMechanisms of Cough From AngiotensinironPas encore d'évaluation
- Therapeutic Plan 4 Acute DMDocument21 pagesTherapeutic Plan 4 Acute DMironPas encore d'évaluation
- Pathology and Pathogenesis of CopdDocument19 pagesPathology and Pathogenesis of CopdironPas encore d'évaluation
- Medical History (Cough)Document3 pagesMedical History (Cough)ironPas encore d'évaluation
- Mechanism of CoughDocument7 pagesMechanism of Coughiron100% (1)
- Emphysema 1Document7 pagesEmphysema 1ironPas encore d'évaluation
- COPD Treatment with Inhaled GlucocorticoidsDocument9 pagesCOPD Treatment with Inhaled GlucocorticoidsironPas encore d'évaluation
- EmphysemaDocument19 pagesEmphysemaironPas encore d'évaluation
- Comparison of three muscle types and skeletal muscle functionDocument5 pagesComparison of three muscle types and skeletal muscle functionjttizzle1995Pas encore d'évaluation
- Integumentary System HandoutDocument18 pagesIntegumentary System HandoutbarchlrPas encore d'évaluation
- Case Study Anaphysio IsDocument4 pagesCase Study Anaphysio IsKaira GoPas encore d'évaluation
- Chinese Acupuncture TestsDocument257 pagesChinese Acupuncture TestsCeline de Haan100% (20)
- Functional Neuroanatomy and Clinical Neuroscience - Foundations For Understanding Disorders of Cognition and Behavior 2022Document465 pagesFunctional Neuroanatomy and Clinical Neuroscience - Foundations For Understanding Disorders of Cognition and Behavior 2022Eduardo RodriguezPas encore d'évaluation
- Peripheral Nervous System: Lesson A1.3Document29 pagesPeripheral Nervous System: Lesson A1.3Khobie PabilicoPas encore d'évaluation
- End-Stage Renal DiseaseDocument3 pagesEnd-Stage Renal DiseaseAkira Pongchad B100% (1)
- Veterinary Sistemic PathologyDocument602 pagesVeterinary Sistemic PathologyEstefania Morales100% (1)
- Iycf AsiaDocument68 pagesIycf AsiaYahye CMPas encore d'évaluation
- Physiology, Lecture 8, The Renal System (Lecture Notes)Document18 pagesPhysiology, Lecture 8, The Renal System (Lecture Notes)Ali Al-Qudsi100% (3)
- History Essay ExamplesDocument6 pagesHistory Essay Examplesb72d994zPas encore d'évaluation
- COBAS 6000: E601 Reagent Inventory MONTH/YEAR: - AUGUST 2020Document3 pagesCOBAS 6000: E601 Reagent Inventory MONTH/YEAR: - AUGUST 2020Charmaine CorpuzPas encore d'évaluation
- Neuroanatomy SamplexDocument2 pagesNeuroanatomy SamplexMineTagraPas encore d'évaluation
- VICTORIA MARTENS AUTOPSY REPORT - Sensitive ContentDocument31 pagesVICTORIA MARTENS AUTOPSY REPORT - Sensitive ContentCourtOnCamera100% (3)
- PowerPoint - Presentation - About - Integumentary - SystemDocument27 pagesPowerPoint - Presentation - About - Integumentary - SystemPrayl Hope NapanoPas encore d'évaluation
- Cardinal Manifestetions of Renal DiseaseDocument61 pagesCardinal Manifestetions of Renal Diseasekirubel deribPas encore d'évaluation
- Understanding the Complex Structure and Function of the Human BrainDocument2 pagesUnderstanding the Complex Structure and Function of the Human Brainbubblegumlover96Pas encore d'évaluation
- FCPS 1 Radiology + AnswersDocument25 pagesFCPS 1 Radiology + AnswersZahid Qamar100% (2)
- Menstrual Cycle Test - Hormones, Phases & FertilityDocument8 pagesMenstrual Cycle Test - Hormones, Phases & FertilityKvmLly100% (1)
- The Three Minds of The Body - Brain, Heart and Gut: Anil K. Rajvanshi Nimbkar Agricultural Research Institute (NARI)Document5 pagesThe Three Minds of The Body - Brain, Heart and Gut: Anil K. Rajvanshi Nimbkar Agricultural Research Institute (NARI)Vashish RamrechaPas encore d'évaluation
- Class Activity Urine FormationDocument2 pagesClass Activity Urine FormationMaryam SheiduPas encore d'évaluation
- Urinary System Review QuestionsDocument3 pagesUrinary System Review QuestionsSaajid AmraPas encore d'évaluation
- Histology Drawings PDFDocument19 pagesHistology Drawings PDFVishwanath Sinduvadi100% (1)
- Digestive System EmbryologyDocument104 pagesDigestive System EmbryologyAlistair WalkerPas encore d'évaluation
- Body Part Ruled By: Sign Ruled By: PlanetDocument7 pagesBody Part Ruled By: Sign Ruled By: PlanetyyyuoPas encore d'évaluation
- Ope-101-Human Anatomy-ModuleDocument37 pagesOpe-101-Human Anatomy-ModuleAlbert MartinezPas encore d'évaluation
- Exam NeurolinguisticsDocument2 pagesExam NeurolinguisticsNatalia NiewiadomskaPas encore d'évaluation
- PDF&Rendition 1Document6 pagesPDF&Rendition 1Budong BernalPas encore d'évaluation
- Skin Anatomy and PhysiologyDocument5 pagesSkin Anatomy and PhysiologyKhan KamaalPas encore d'évaluation
- Calcium PPT BSDocument58 pagesCalcium PPT BSMedical NotesPas encore d'évaluation