Académique Documents
Professionnel Documents
Culture Documents
Etosuksimid
Transféré par
Maharani Indriaty0 évaluation0% ont trouvé ce document utile (0 vote)
102 vues14 pagesobat etosuksimid
Titre original
etosuksimid
Copyright
© © All Rights Reserved
Formats disponibles
PPTX, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentobat etosuksimid
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PPTX, PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
102 vues14 pagesEtosuksimid
Transféré par
Maharani Indriatyobat etosuksimid
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PPTX, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 14
INTRODUCTION
Ethosuximide is succinimide compound that is effective in the
treatment of absence seizures. It is the product of an intense
structure-activity research effort to find an specific agent to
suppress absence seizures with a relatively low side effect
profile. While the exact mechanism of action is not known, the
antiepileptic effect of ethosuximide is thought to result from
its ability to decrease low-threshold calcium currents in
thalamic neurons. The thalamus has a key role in the
production of 3-Hz spike-wave rhythms that are a hallmark of
absence seizures. Ethosuximide may also inhibit the sodium-
potassium ATPase system and NADPH-linked aldehyde
reductase.
THERAPEUTIC AND TOXIC CONCENTRATIONS
The therapeutic range for ethosuximide is defined
by most laboratories as 40100 g/mL, although
some clinicians suggest drug concentrations as high
as 150 g/mL with appropriate monitoring of
serum concentrations and possible side effects.5
The most common adverse effects of ethosuximide
are gastric distress, nausea, vomiting, and anorexia,
but these gastrointestinal problems appear to be
caused by local irritation of gastric mucosa.
Generally, administration of smaller doses and more
frequent dosing of the drug produce relief from these
side effects. In the upper end of the therapeutic range
(>70 g/mL) some patients will begin to experience the
concentration-dependent adverse effects of
ethosuximide treatment: drowsiness, fatigue, lethargy,
dizziness, ataxia, hiccups, euphoria, and headaches.
Idiosyncratic side effects that are independent of
concentration include rash, systemic lupus-like
syndromes, and blood dyscrasias (leukopenia,
pancytopenia).
CLINICAL MONITORING PARAMETERS
The goal of therapy with anticonvulsants is to reduce seizure
frequency and maximize quality of life with a minimum of
adverse drug effects. While it is desirable to entirely abolish all
seizure episodes, it may not be possible to accomplish this in
many patients. Patients should be monitored for
concentration-related side effects (drowsiness, fatigue,
lethargy, dizziness, ataxia, hiccups, euphoria, headaches) as
well as gastrointestinal upset associated with local irritation of
gastric mucosa (gastric distress, nausea, vomiting, anorexia).
Serious, but rare, idiosyncratic side effects include systemic
lupus-like syndromes, leukopenia, and pancytopenia.
Ethosuximide serum concentrations should be measured
in most patients. Because epilepsy is an episodic disease
state, patients do not experience seizures on a
continuous basis. Thus, during dosage titration it is
difficult to tell if the patient is responding to drug therapy
or simply is not experiencing any abnormal central
nervous system discharges at that time. Ethosuximide
serum concentrations are also valuable tools to avoid
adverse drug effects. Patients are more likely to accept
drug therapy if adverse reactions are held to the absolute
minimum.
BASIC CLINICAL PHARMACOKINETIC PARAMETERS
Ethosuximide is eliminated primarily by hepatic metabolism (7080%)
via hydroxylation and then conjugated to inactive metabolites. About
2030% of an ethosuximide dose is recovered as unchanged drug in
the urine. Ethosuximide is not significantly bound to plasma proteins.
At concentrations exceeding 100 g/mL, the drug may follow
nonlinear pharmacokinetics, presumably owing to Michaelis-Menten
(concentration dependent or saturable) metabolism. Because an
intravenous form of the drug is not commercially available, the
absolute bioavailability in humans is not known. However, based on
animal studies, ethosuximide oral bioavailability of capsules (250 mg)
and syrup (250 mg/5 mL) is assumed to be 100%. The typical
maintenance dose for ethosuximide is 20 mg/kg/d for pediatric
patients (<12 years old) and 15 mg/kg/d for older patients.
EFFECTS OF DISEASE STATES AND CONDITIONS
ON PHARMACOKINETICS AND DOSING
Ethosuximide oral clearance rate (Cl/F) for older children (12 years
old) and adults is 12 mL/h/kg and for younger children is 16
mL/h/kg. Ethosuximide volume of distribution (V/F) equals 0.7 L/kg,
and its half life averages 30 hours in children and 60 hours in adults.
Although studies in patients with hepatic disease are not available,
7080% of the drug is eliminated by hepatic metabolism. Because of
this, patients with liver cirrhosis or acute hepatitis may have
reduced ethosuximide clearance because of destruction of liver
parenchyma. This loss of functional hepatic cells reduces the
amount of enzymes available to metabolize the drug and decreases
clearance. An index of liver dysfunction can be gained by applying
the Child-Pugh clinical classification system to the patient (Table 14-
2).
DRUG INTERACTIONS
Unlike other antiepileptic drugs, ethosuximide
is not a hepatic enzyme inducer or inhibitor,
and appears to cause no clinically important
drug interactions. Valproic acid can inhibit
ethosuximide metabolism and increase
steady-state concentrations, especially when
ethosuximide serum concentrations are in the
upper end of the therapeutic range.
INITIAL DOSAGE DETERMINATION
METHODS
Several methods to initiate ethosuximide therapy are
available. The pharmacokinetic dosing method is the most
flexible of the techniques. It allows individualized target serum
concentrations to be chosen for a patient, and each
pharmacokinetic parameter can be customized to reflect
specific disease states and conditions present in the patient.
Literature-based recommended dosing is a very commonly
used method to prescribe initial doses of ethosuximide. Doses
are based on those that commonly produce steady-state
concentrations in the lower end of the therapeutic range,
although there is a wide variation in the actual concentrations
for a specific patient.
Pharmacokinetic Dosing Method
The goal of initial dosing of ethosuximide is to compute the
best dose possible for the patient given their set of disease
states and conditions that influence ethosuximide
pharmacokinetics and the epileptic disorder being treated. In
order to do this, pharmacokinetic parameters for the patient
will be estimated using average parameters measured in other
patients with similar disease state and condition profiles
(CLEARANCE ESTIMATE, VOLUME OF DISTRIBUTION ESTIMATE,
HALF-LIFE AND ELIMINATION RATE CONSTANT ESTIMATE,
SELECTION OF APPROPRIATE PHARMACOKINETIC MODEL AND
EQUATIONS).
Ethosuximide follows a one-compartment pharmacokinetic model.
When oral therapy is required, ethosuximide has good
bioavailability (F = 1), and once or twice dosing provides a relatively
smooth serum concentration/time curve that emulates an
intravenous infusion. Because of this, a very simple pharmacokinetic
equation that computes the average ethosuximide steady-state
serum concentration (Css in g/mL = mg/L) is widely used and
allows maintenance dosage calculation: Css = [F(D/)] / Cl or D = (Css
Cl ) / F, where F is the bioavailability fraction for the oral dosage
form (F = 1 for oral ethosuximide products), D is the dose of
ethosuximide in milligrams, Cl is ethosuximide clearance in liters per
hour, and is the dosage interval in hours.
Vous aimerez peut-être aussi
- Paracetamol Drug StudyDocument33 pagesParacetamol Drug Studycgmartelino.sbcmPas encore d'évaluation
- Montelukast SodiumDocument10 pagesMontelukast SodiumikhasilPas encore d'évaluation
- Mepivacaine 3%Document6 pagesMepivacaine 3%Victor KurniawanPas encore d'évaluation
- Pharmacokinetics of Anti-Epileptic Drugs and Their Clinical SignificanceDocument12 pagesPharmacokinetics of Anti-Epileptic Drugs and Their Clinical Significancerozina mulatPas encore d'évaluation
- Opiod AnalgesicsDocument13 pagesOpiod Analgesicschebetnaomi945Pas encore d'évaluation
- DMARD'sDocument9 pagesDMARD'sterencedszaPas encore d'évaluation
- PharmDocument67 pagesPharmElisabeth Permatasari SidabutarPas encore d'évaluation
- Sem3 - Pharmacotherapy Pearls For Emergency Neurological Life SupportDocument26 pagesSem3 - Pharmacotherapy Pearls For Emergency Neurological Life SupportOlga Manco GuzmánPas encore d'évaluation
- Clinical Pharmacokinetics Therapeutic Drug MonitoringDocument41 pagesClinical Pharmacokinetics Therapeutic Drug MonitoringTrifena Prisca MossePas encore d'évaluation
- EtopexDocument11 pagesEtopexMohammed HaiderPas encore d'évaluation
- Farmacoterapia en Soporte NeurológicoDocument26 pagesFarmacoterapia en Soporte NeurológicoIvan Mauricio Palma BarraganPas encore d'évaluation
- Drug StudyDocument11 pagesDrug StudyKaloy KamaoPas encore d'évaluation
- Analysis of Dose Response Relationship: by Lee Eun JinDocument63 pagesAnalysis of Dose Response Relationship: by Lee Eun JinSunil100% (1)
- Pharmacology 1Document32 pagesPharmacology 1jekeri bekeriPas encore d'évaluation
- Anesthesia For Patients With Renal DiseaseDocument4 pagesAnesthesia For Patients With Renal DiseasejoninhabPas encore d'évaluation
- Drugs Coronary Ward IIDocument7 pagesDrugs Coronary Ward IITimothy Joy VercelesPas encore d'évaluation
- Furosemide Tables:: Pharmacokinetics Bioavailability Peak Plasma Level Plasma Half-Life Active Metabolites EliminationDocument4 pagesFurosemide Tables:: Pharmacokinetics Bioavailability Peak Plasma Level Plasma Half-Life Active Metabolites Eliminationmole_fkPas encore d'évaluation
- 01 - Pharmacotherapy Pearls For Emergency Neurological Life Support PDFDocument26 pages01 - Pharmacotherapy Pearls For Emergency Neurological Life Support PDFawinsyPas encore d'évaluation
- Solu CortefDocument4 pagesSolu CortefOliver BagarinaoPas encore d'évaluation
- Nausea Vomiting - DhitaDocument78 pagesNausea Vomiting - DhitawePas encore d'évaluation
- MoexiprilDocument23 pagesMoexiprilYeyenJaejoongPas encore d'évaluation
- Pharmacology HESI Study Guide 2013Document16 pagesPharmacology HESI Study Guide 2013naijababy89100% (12)
- Bioavailability and Bioequivalence. Therapeutic Drug MonitoringDocument3 pagesBioavailability and Bioequivalence. Therapeutic Drug MonitoringJoel MathewPas encore d'évaluation
- Document 1Document4 pagesDocument 1kamaluPas encore d'évaluation
- البراسيتول في استرالياDocument11 pagesالبراسيتول في استراليازيد محمدPas encore d'évaluation
- Drug StudyDocument6 pagesDrug StudyMarielle Denise Tagtag BugtongPas encore d'évaluation
- Drug Interactions: MSC Tid 1 Nyakundi BM April 21 2010Document43 pagesDrug Interactions: MSC Tid 1 Nyakundi BM April 21 2010MONALISA MISTRIPas encore d'évaluation
- Nursing Diagnosing (PDAR)Document4 pagesNursing Diagnosing (PDAR)dakiePas encore d'évaluation
- Ospolot 200 MG, Film-Coated Tablets: Summary of Product Characteristics (SPC)Document7 pagesOspolot 200 MG, Film-Coated Tablets: Summary of Product Characteristics (SPC)ddandan_2Pas encore d'évaluation
- #06-Cholinoceptor-Activating-Cholinesterase-Inh-Drugs - v2Document66 pages#06-Cholinoceptor-Activating-Cholinesterase-Inh-Drugs - v2tasnemaldaherPas encore d'évaluation
- PharmacologyDocument116 pagesPharmacologyvarghesePas encore d'évaluation
- Pharmacodynamics (Agonists: Mechanisms of Drug Actions)Document36 pagesPharmacodynamics (Agonists: Mechanisms of Drug Actions)Wajid HusseinPas encore d'évaluation
- Test Farma En-Ro, Ro-EnDocument3 pagesTest Farma En-Ro, Ro-EnIuliaUngurPas encore d'évaluation
- Notes 1Document24 pagesNotes 1coosa liquorsPas encore d'évaluation
- AtropineDocument13 pagesAtropineMostafa HassanPas encore d'évaluation
- EPIRUBICIN Ferron PharmaceuticalsDocument7 pagesEPIRUBICIN Ferron PharmaceuticalsHep PutPas encore d'évaluation
- Drug StudyDocument3 pagesDrug StudyGail SantosPas encore d'évaluation
- Abnormal Laboratory Results: Therapeutic Drug Monitoring: Which Drugs, Why, When AndhowtodoitDocument3 pagesAbnormal Laboratory Results: Therapeutic Drug Monitoring: Which Drugs, Why, When AndhowtodoitvlkñpPas encore d'évaluation
- PHARM ATI ReviewDocument76 pagesPHARM ATI Reviewth233100% (1)
- AntiepilepticsDocument13 pagesAntiepilepticstbuyinza21apPas encore d'évaluation
- Anti-Seizure Medications: by Dawit S. (R3)Document53 pagesAnti-Seizure Medications: by Dawit S. (R3)ጉራማይሌ TubePas encore d'évaluation
- Etoposide Consumer InformationDocument13 pagesEtoposide Consumer InformationEdson KarundengPas encore d'évaluation
- Hepatic Encephalopathy: DR Sadath HussainDocument32 pagesHepatic Encephalopathy: DR Sadath Hussain966342Pas encore d'évaluation
- Preoperative PremedicationsDocument90 pagesPreoperative PremedicationsMorad SatariPas encore d'évaluation
- New Zealand Data Sheet: ActionsDocument17 pagesNew Zealand Data Sheet: Actionsheri siswanto nur sidikPas encore d'évaluation
- AEDand LiverdiseaseDocument22 pagesAEDand LiverdiseaseEmir SmailbegovićPas encore d'évaluation
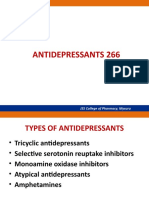
- Antidepressants 266: JSS College of Pharmacy, MysuruDocument68 pagesAntidepressants 266: JSS College of Pharmacy, MysurucrissPas encore d'évaluation
- Montair LC TabletsDocument9 pagesMontair LC Tabletskurutala100% (1)
- Analgesic: Mefenamic AcidDocument5 pagesAnalgesic: Mefenamic Acidmegazhang94Pas encore d'évaluation
- Febuxostat (Uloric), A New Treatment Option For Gout: Carmela Avena-Woods Olga Hilas Author Information Go ToDocument9 pagesFebuxostat (Uloric), A New Treatment Option For Gout: Carmela Avena-Woods Olga Hilas Author Information Go ToAnadi GuptaPas encore d'évaluation
- N C by Dr. Mohamed Baraka: Ausea AND Vomiting Onstipation AND DiarrheaDocument72 pagesN C by Dr. Mohamed Baraka: Ausea AND Vomiting Onstipation AND DiarrheaIbrahim Mahmoud AliPas encore d'évaluation
- Rational Drug Use in Hepatobiliary Disorders UdayanaDocument27 pagesRational Drug Use in Hepatobiliary Disorders UdayanaDhan RamadhanPas encore d'évaluation
- Anesthesia in Hepatic DiseaseDocument3 pagesAnesthesia in Hepatic DiseaseRoxana SurliuPas encore d'évaluation
- Therapeutic Drug Monitoring-FinalDocument49 pagesTherapeutic Drug Monitoring-FinalSaiesh PhaldesaiPas encore d'évaluation
- Esofast (Esomeprazole)Document5 pagesEsofast (Esomeprazole)Asim Liaquat Khan100% (1)
- Anti Epileptic AgentsDocument64 pagesAnti Epileptic AgentsPrincess VanquirayPas encore d'évaluation
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesD'EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesÉvaluation : 4 sur 5 étoiles4/5 (2)
- Handbook of Drug Interaction and the Mechanism of InteractionD'EverandHandbook of Drug Interaction and the Mechanism of InteractionÉvaluation : 1 sur 5 étoiles1/5 (1)
- Serovar Australis: Leptospira Serovar Data SheetDocument1 pageSerovar Australis: Leptospira Serovar Data SheetfrankyPas encore d'évaluation
- PSAvs PsadDocument6 pagesPSAvs PsadRaga ManduaruPas encore d'évaluation
- Elias On 1983Document3 pagesElias On 1983JesusCordoba100% (2)
- Psiquiatria de Enlace Delirium TremensDocument14 pagesPsiquiatria de Enlace Delirium Tremensdiego isaac ramirez angaritaPas encore d'évaluation
- 766ue 2019-01Document101 pages766ue 2019-01Angelita Kstro D SilvaPas encore d'évaluation
- Smith Potencijalni ProstorDocument13 pagesSmith Potencijalni ProstorЈован Д. РадовановићPas encore d'évaluation
- KalanchoeDocument1 pageKalanchoeAnonymous iOYpj92Pas encore d'évaluation
- Renal Nursing ReviewerDocument8 pagesRenal Nursing ReviewerGeraldine Waje100% (2)
- MudrasDocument8 pagesMudrasKishore CheralaPas encore d'évaluation
- Burns Secret TestDocument2 pagesBurns Secret TestChin ChanPas encore d'évaluation
- Mwalya Wambua Final ProjectDocument49 pagesMwalya Wambua Final ProjectWILSON MACHARIAPas encore d'évaluation
- False Advertisement Gluten Free FoodDocument9 pagesFalse Advertisement Gluten Free FoodElenaPas encore d'évaluation
- USMLE Step 3 Sample Questions For The Test PDFDocument69 pagesUSMLE Step 3 Sample Questions For The Test PDFmarkPas encore d'évaluation
- Course NotesDocument125 pagesCourse Notesfuji_reihPas encore d'évaluation
- Capstone OutlineDocument3 pagesCapstone Outlineapi-395468231Pas encore d'évaluation
- Faith HealingDocument23 pagesFaith Healingcreamyfrappe0% (1)
- This Study Resource WasDocument3 pagesThis Study Resource WasCarlito AglipayPas encore d'évaluation
- Measurement ScalesDocument6 pagesMeasurement ScalesRohit PandeyPas encore d'évaluation
- The Impact of Tumor Biology On Cancer Treatment and Multidisciplinary Strategies - M. Molls, Et Al., (Springer, 2009) WWDocument363 pagesThe Impact of Tumor Biology On Cancer Treatment and Multidisciplinary Strategies - M. Molls, Et Al., (Springer, 2009) WWiuliPas encore d'évaluation
- Report of Mangalore VisitDocument6 pagesReport of Mangalore VisitAmal DominicPas encore d'évaluation
- Asperger Syndrome in ChildrenDocument8 pagesAsperger Syndrome in Childrenmaria_kazaPas encore d'évaluation
- Voluntary Blood DonationDocument8 pagesVoluntary Blood DonationJessa CanonigoPas encore d'évaluation
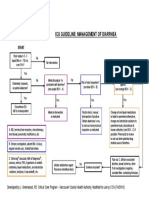
- Icu Guideline: Management of Diarrhea: StartDocument1 pageIcu Guideline: Management of Diarrhea: StartGracia VionaPas encore d'évaluation
- Art Theraphy AutismDocument2 pagesArt Theraphy AutismMatheaFiliPas encore d'évaluation
- Clark IndigestionDocument50 pagesClark IndigestionRaveendra MungaraPas encore d'évaluation
- Iso 10555-1 2013Document30 pagesIso 10555-1 2013Nick Ngo67% (3)
- Antibiotics Chart 1Document7 pagesAntibiotics Chart 1Vee MendPas encore d'évaluation
- Faber TestDocument8 pagesFaber TestHaura TsabitahPas encore d'évaluation
- DkaDocument32 pagesDkanathePas encore d'évaluation
- Analisis Berkaitan Penderaan Emosi Terhadap Kanak-Kanak Dari Sudut PerundanganDocument27 pagesAnalisis Berkaitan Penderaan Emosi Terhadap Kanak-Kanak Dari Sudut PerundanganJamuna BatumalaiPas encore d'évaluation