Académique Documents
Professionnel Documents
Culture Documents
Respiratory Failure (KK 2a)
Transféré par
IlaJako Stefanatic0 évaluation0% ont trouvé ce document utile (0 vote)
308 vues29 pagesThis document discusses respiratory failure, which occurs when one or both of the gas exchange systems (air entering the lungs or oxygen entering the blood from the lungs) is inadequate. There are two main types - hypoxemic respiratory failure, where oxygenation is inadequate, and hypercapnic respiratory failure, where ventilation is inadequate and carbon dioxide levels rise. Causes can include issues with the airways, lungs, chest wall, nervous system or muscles. Diagnosis involves blood gas analysis and other tests. Treatment focuses on addressing the underlying cause, providing oxygen therapy, mobilizing secretions, mechanical ventilation if needed, medications, nutrition support, and careful nursing care of patients on ventilators to prevent complications.
Description originale:
respiratory
Titre original
Respiratory Failure (Kk 2a)
Copyright
© © All Rights Reserved
Formats disponibles
PPTX, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentThis document discusses respiratory failure, which occurs when one or both of the gas exchange systems (air entering the lungs or oxygen entering the blood from the lungs) is inadequate. There are two main types - hypoxemic respiratory failure, where oxygenation is inadequate, and hypercapnic respiratory failure, where ventilation is inadequate and carbon dioxide levels rise. Causes can include issues with the airways, lungs, chest wall, nervous system or muscles. Diagnosis involves blood gas analysis and other tests. Treatment focuses on addressing the underlying cause, providing oxygen therapy, mobilizing secretions, mechanical ventilation if needed, medications, nutrition support, and careful nursing care of patients on ventilators to prevent complications.
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PPTX, PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
308 vues29 pagesRespiratory Failure (KK 2a)
Transféré par
IlaJako StefanaticThis document discusses respiratory failure, which occurs when one or both of the gas exchange systems (air entering the lungs or oxygen entering the blood from the lungs) is inadequate. There are two main types - hypoxemic respiratory failure, where oxygenation is inadequate, and hypercapnic respiratory failure, where ventilation is inadequate and carbon dioxide levels rise. Causes can include issues with the airways, lungs, chest wall, nervous system or muscles. Diagnosis involves blood gas analysis and other tests. Treatment focuses on addressing the underlying cause, providing oxygen therapy, mobilizing secretions, mechanical ventilation if needed, medications, nutrition support, and careful nursing care of patients on ventilators to prevent complications.
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PPTX, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 29
Respiratory Failure
Siswoyo & Wantiyah
Resp Failure:one or both exchanging systems
is inadequate (air to lung or lung to blood)
Blood Supply to Lung
Respiratory Failure
Not a disease process, sign of severe dysfunction
Predisposing Factors:
Airways/alveoli
CNS
Chest wall
Neuromuscular
Commonly defined in terms of ABGs:
PO2 of less than 60 mmHg
PCO2 greater than 45 mmHg
Arterial pH of less than 7.35
Classification of Respiratory Failure
Hypoxemic Respiratory Failure
Oxygenation failure- inadequate O2 transfer
between alveoli & pulmonary capillary bed
PaO2 60 mm Hg or less on 60 % O2
Inadequate O2 saturation of hemoglobin
Causes tissue hypoxia > Metabolic acidosis; cell
death; decreased CO; impaired renal function
Common causes: disorders that interfere with O2
transfer into the blood- respiratory or cardiac
system
Hypoxemic Respiratory Failure
Mechanisms that may lead to Hypoxemia:
1. Mismatch ventilation & perfusion (V/Q mismatch)
V/Q: Volume blood perfusing lungs each minute
Each ml of air for each ml of blood
1:1= V/Q ratio of 1
Causes of V/Q mismatch:
Ventilation portion blocked (secretions in
airway/alveoli, airway/alveolar collapse, decreased
movement chest/ventilation)
Perfusion portion blocked (pulmonary embolus)
Hypoxemic Respiratory Failure
Range of ventilation to perfusion (V/Q relationship)
A. Absolute shunt, no
ventilation fluid in alveoli
B. Ventilation partially
compromised- secretions
C. Normal lung unit
D. Perfusion partially
compromised by emboli
obstructing blood flow
E. Dead space: no
perfusion- obstruction of
pulmonary capillary
Hypoxemic Respiratory Failure
Mechanisms that may lead to Hypoxemia:
2. Shunt- Extreme V/Q mismatch
Occurs when blood
leaves heart without gas
exchange
Types:
1. anatomic shunt: O2
blood does not pass
through lungs
2. intrapulmonary shunt-
alveoli fill with fluid
Treatment: Mechanical
ventilation to force O2
into lungs; treat cause
Hypoxemic Respiratory Failure
Mechanisms may lead to Hypoxemia:
3. Diffusion limitations
Alveoli membrane
thickened or destroyed
Gas exchange across
alveolar-capillary
membrane cant occur
Classic sign: hypoxemia
present during exercise,
not at rest
Treat the cause such as
pulmonary fibrosis;
ARDS
Hypoxemic Respiratory Failure
Mechanisms may lead to Hypoxemia:
Clinical manifestations of hypoxemia
Specific: Respiratory:
Nonspecific: Cerebral, cardiac, other
Treatment: treat cause, O2 and mechanical
ventilation
Hypercapnic Respiratory Failure
Ventatory failure: Inability of the respiratory system to
ventilate out sufficient CO2 to maintain normal PaCO2
PaCO2 greater than 45 mm Hg, Arterial pH less than 7.35
PCO2 rises rapidly and respiratory acidosis develops,
PO2 drops more slowly
Common causes include disorders that compromise lung
ventilation and CO2 removal (airways/alveoli, CNS, chest
wall, neuromuscular)
Clinical manifestations: specific respiratory, nonspecific
of cerebral, cardiac, neuromuscular
Treatment: adeq O2, airway, meds, treat underlying cause,
nutrition
Collaborative Care for Respiratory Failure:
Diagnostic tests
History/physical assessment
Pulse oximetry
ABG analysis
Chest X-ray
CBC, sputum/blood cultures, electrolytes
EKG
Urinalysis
V/Q scan- if pulmonary embolism suspected
Hemodynamic monitor/pulmonary function tests
Collaborative care for Respiratory Failure
Respiratory Therapy
Main treatment- correct underlying cause & restore
adequate gas exchange in lung
Oxygen Therapy (Maintain PaO2 at least 60 mm Hg,
SaO2 90%)
Mobilization of secretions
Effective coughing & positioning
Hydration & humidification
Chest physical therapy
Airway suctioning
Positive pressure ventilation
Noninvasive positive pressure ventilation
Intubation with mechanical ventilation
Collaborative Care for
Respiratory Failure cont
Drug Therapy
Relief bronchospasm; reduce airway inflam and
pulmonary congestion; treat pulmonary infections;
reduce anxiety, pain
Medical supportive therapy
Treat underlying cause
Nutritional therapy
Enteral; parenteral
Protein and energy stores
Collaborative Care: Artifical airways-
tracheostomy and endotracheal tubes
Endotracheal tube
Taping and inline suctioning of an
endotracheal tube
Exhaled C02 (ETC02) normal 35-45
Used when trying to wean
patient from a ventilator
Independent Lung Ventilation
Collaborative Care:
Mechanical Ventilation
Provide adeq gas
exchange
Criteria to put on vent
RR > 35-45
pCO2 >45
pO2 <50
Types- Positive, Neg
Types: Negative pressure ventilator
Types: Positive pressure mechanical
ventilation with endotracheal tube (PPV)
Complications/Nursing Care of
Positive Pressure Mechanical ventilation
Cardiovascular: decreased CO; inc intrathoracic pressure
Pulmonary: Barotrauma; Volutrauma; alveolar
hypoventilation/hyperventilation; ventilator-associated
pneumonia
Sodium and water imbalance
Neurological: impaired cerebral bl flow>IICP
Gastrointestional: stress ulcer/GI bleed; gas; constipation
Musculoskeletal: dec muscle tone; contractures; footdrop;
pressure ulcers from BR
Psychosocial: physical & emotional stress; fight vent
Other problems
when on mechanical ventilation
Machine disconnection or malfunction
Nutrition needs
Nursing assessment specific to
Respiratory Failure
Assess both airway and
lungs
Refer to hypoxic and
hypercapnic respiratory
failure symptoms
Data:
Subjective data
Objective data
Nursing Diagnoses
Impaired spontaneous ventilation
Impaired gas exchange r.t mismatch
perfusion-ventilation
Relevant Nursing Problems related to
Respiratory Failure
Prevention of acute respiratory failure
Nursing Care Plans
Gerontology considerations
Nursing Care Plans Mechanical ventilation
Suctioning procedure and oral care
29
Vous aimerez peut-être aussi
- Pulmonary PathophysiologyDocument146 pagesPulmonary PathophysiologySeeta NanooPas encore d'évaluation
- Shock, Sirs & ModsDocument37 pagesShock, Sirs & ModsambitioustamannaPas encore d'évaluation
- Uber Eats Business Model CanvasDocument1 pageUber Eats Business Model Canvass MishraPas encore d'évaluation
- Atelectasis, (Lung Collapse) A Simple Guide To The Condition, Diagnosis, Treatment And Related DiseasesD'EverandAtelectasis, (Lung Collapse) A Simple Guide To The Condition, Diagnosis, Treatment And Related DiseasesPas encore d'évaluation
- Denglish TestDocument139 pagesDenglish TestNabil HasanPas encore d'évaluation
- Acute Respiratory Failure LectureDocument53 pagesAcute Respiratory Failure Lectureprototypeallhell100% (2)
- Noninvasive VentilationDocument6 pagesNoninvasive VentilationEma MagfirahPas encore d'évaluation
- Literature ReviewDocument7 pagesLiterature Reviewapi-353923446Pas encore d'évaluation
- Introduction To Mechanical VentilationDocument5 pagesIntroduction To Mechanical VentilationHussam GujjarPas encore d'évaluation
- Patient History TemplateDocument2 pagesPatient History TemplateDr Shazana NazrinPas encore d'évaluation
- English ExercisesDocument2 pagesEnglish ExercisesLiceth HuertasPas encore d'évaluation
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsD'EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsPas encore d'évaluation
- Pediatric Cardio-Respiratory AssessmentDocument9 pagesPediatric Cardio-Respiratory AssessmentRicky SpideyPas encore d'évaluation
- Respiratory PhysiologyDocument16 pagesRespiratory PhysiologyYsabel Salvador DychincoPas encore d'évaluation
- Adventitious Breath SoundsDocument1 pageAdventitious Breath SoundsEdwin Delos Reyes AbuPas encore d'évaluation
- NIPPVDocument35 pagesNIPPVAnusha VerghesePas encore d'évaluation
- Lung Pathology Flow ChartsDocument6 pagesLung Pathology Flow ChartsZagros MotamedPas encore d'évaluation
- Assessment of The Chest and LungsDocument46 pagesAssessment of The Chest and LungsSumathi GopinathPas encore d'évaluation
- Denso HP4Document87 pagesDenso HP4Abraham Janco Janco100% (2)
- Acute Respiratory Distress Syndrome (Ards)Document17 pagesAcute Respiratory Distress Syndrome (Ards)joyrena ochondra0% (1)
- Acute Respiratory Distress SyndromeDocument77 pagesAcute Respiratory Distress SyndromeAnnisa Dyah ChairiniPas encore d'évaluation
- Ards and RF FileDocument12 pagesArds and RF FileEdwin Delos Reyes Abu100% (1)
- Cpap and Bipap: "A CPAP A Day Helps Keep The ET Tube Away!"Document15 pagesCpap and Bipap: "A CPAP A Day Helps Keep The ET Tube Away!"Muhammad Tayyab MadniPas encore d'évaluation
- RespiratoryDocument161 pagesRespiratoryDanity_Anne_Ba_1326100% (1)
- PericarditisDocument29 pagesPericarditisPavin KumarPas encore d'évaluation
- Earthquake Lesson Plan 2022Document5 pagesEarthquake Lesson Plan 2022Maylyn Grace Dalumpines-Colon EbonaloPas encore d'évaluation
- Pneumonia: DefinitionDocument5 pagesPneumonia: DefinitionhemaanandhyPas encore d'évaluation
- Pulmonary: Ftplectures Pulmonary System Lecture NotesDocument34 pagesPulmonary: Ftplectures Pulmonary System Lecture NotesArif Setyawan100% (1)
- 8 Lung Auscultation Points and SoundsDocument11 pages8 Lung Auscultation Points and SoundsCHARIEMAE CA�AZARES100% (1)
- Breathing and Exchange of GasesDocument5 pagesBreathing and Exchange of Gaseslpc4944Pas encore d'évaluation
- Mechvent Review (Topnotcher)Document284 pagesMechvent Review (Topnotcher)Gleo Matthew100% (1)
- 1 CPG Asthma GuidelinesDocument19 pages1 CPG Asthma GuidelinesShofiyyatunnisa' WsPas encore d'évaluation
- Bronchiectasis: By: Karunesh KumarDocument21 pagesBronchiectasis: By: Karunesh KumarAnkan DeyPas encore d'évaluation
- Respiratory Distress in The NewbornDocument8 pagesRespiratory Distress in The Newbornandbpf6819Pas encore d'évaluation
- Fellowship 2nd Edition Book 2 - Inverse Fellowship (Playbooks)Document44 pagesFellowship 2nd Edition Book 2 - Inverse Fellowship (Playbooks)AlePas encore d'évaluation
- CRT Exam Review Guide Chapter 13Document23 pagesCRT Exam Review Guide Chapter 13Dharlyn MungcalPas encore d'évaluation
- Tachycardia Approach and ManagementDocument41 pagesTachycardia Approach and ManagementChadi Alraies100% (5)
- A Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsD'EverandA Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsPas encore d'évaluation
- CHEst TraumaDocument20 pagesCHEst TraumajeorjPas encore d'évaluation
- Lung Metabolism: Proteolysis and Antioproteolysis Biochemical Pharmacology Handling of Bioactive SubstancesD'EverandLung Metabolism: Proteolysis and Antioproteolysis Biochemical Pharmacology Handling of Bioactive SubstancesAlain JunodPas encore d'évaluation
- 20 Heirs of Alfredo Bautista VS LindoDocument3 pages20 Heirs of Alfredo Bautista VS LindoJerome LeañoPas encore d'évaluation
- Emcee Script For CompetitionDocument2 pagesEmcee Script For CompetitionArdini Izzati100% (3)
- Respiratory Therapist, NICU/ICUDocument5 pagesRespiratory Therapist, NICU/ICUapi-77517256Pas encore d'évaluation
- HLX 150Document44 pagesHLX 150menendez2050100% (1)
- Respiratory Diseases of NewbornDocument93 pagesRespiratory Diseases of NewbornTheva Thy100% (1)
- The Different Types of Respiratory Diseases Prevalent in KenyaDocument9 pagesThe Different Types of Respiratory Diseases Prevalent in KenyaKimberlyNekesaPas encore d'évaluation
- Critical Thinking in Respiratory Care Practice PDFDocument17 pagesCritical Thinking in Respiratory Care Practice PDFFernando MorenoPas encore d'évaluation
- Registered Respiratory TherapistDocument3 pagesRegistered Respiratory Therapistapi-76909521Pas encore d'évaluation
- Complications of General Anesthesia (Summary)Document19 pagesComplications of General Anesthesia (Summary)Hassan.shehri100% (2)
- Assessment of Respiratory Function Chpt.20Document32 pagesAssessment of Respiratory Function Chpt.20Maricar RosasPas encore d'évaluation
- Newborn EmergenciesDocument83 pagesNewborn EmergencieshwelpPas encore d'évaluation
- Respiratory Case StudiesDocument6 pagesRespiratory Case Studiesadom09Pas encore d'évaluation
- Extubation CriteriaDocument17 pagesExtubation CriteriaOliver TabagPas encore d'évaluation
- Atelectasis: Contraction Atelectasis (Or Cicatrization Atelectasis)Document10 pagesAtelectasis: Contraction Atelectasis (Or Cicatrization Atelectasis)Gan BangPas encore d'évaluation
- 03 Weaning, SBT and Weaning ParametersDocument48 pages03 Weaning, SBT and Weaning ParametersaryoPas encore d'évaluation
- Respiratory EmergenciesDocument34 pagesRespiratory EmergenciesRoshana MallawaarachchiPas encore d'évaluation
- Mechanical Ventilation and Intracranial PressureDocument30 pagesMechanical Ventilation and Intracranial PressureFlavius AnghelPas encore d'évaluation
- Lower Respiratory Tract InfectionDocument9 pagesLower Respiratory Tract InfectionNamrah AfzalPas encore d'évaluation
- Oxygenation and Oxygen TherapyDocument11 pagesOxygenation and Oxygen TherapyJenn77x1Pas encore d'évaluation
- Chronic Obstructive Pulmonary Disease: Olivia Faye J Listanco IM Resident January 21, 2016Document52 pagesChronic Obstructive Pulmonary Disease: Olivia Faye J Listanco IM Resident January 21, 2016FayeListancoPas encore d'évaluation
- Cardiovascular Pathology 1:: Blood VesselsDocument48 pagesCardiovascular Pathology 1:: Blood VesselsRaiver CadenPas encore d'évaluation
- Chest Trauma FinalDocument50 pagesChest Trauma FinalAsim Siddiq VinePas encore d'évaluation
- Mechanical Ventilation TherapyDocument17 pagesMechanical Ventilation TherapyFaizal FlPas encore d'évaluation
- HemiplegiaDocument17 pagesHemiplegiaStefany CelinePas encore d'évaluation
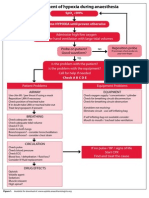
- Management of Hypoxia During AnaesthesiaDocument5 pagesManagement of Hypoxia During AnaesthesiaNurhafizahImfista100% (1)
- Laboratory Examinations: Allen's Test Normal Finding: Hand Quickly BecomesDocument9 pagesLaboratory Examinations: Allen's Test Normal Finding: Hand Quickly BecomesShane GumaponPas encore d'évaluation
- Cardiovascular Disorders 1Document44 pagesCardiovascular Disorders 1Nader Smadi100% (1)
- The Management of Acute Respiratory Distress SyndromeDocument48 pagesThe Management of Acute Respiratory Distress SyndromeLauraAlvarezMulettPas encore d'évaluation
- RT 220 B C AirwaystudyguideDocument25 pagesRT 220 B C Airwaystudyguiderpebdani0% (2)
- The Thorax and Lungs - BATESDocument4 pagesThe Thorax and Lungs - BATESsitalcoolk100% (2)
- Ginko Biloba1Document9 pagesGinko Biloba1IlaJako StefanaticPas encore d'évaluation
- Fat Embolism Syndrome After Femur Fracture Fixation: A Case ReportDocument8 pagesFat Embolism Syndrome After Femur Fracture Fixation: A Case ReportIlaJako StefanaticPas encore d'évaluation
- Jurnal HipertensiDocument7 pagesJurnal HipertensiIlaJako StefanaticPas encore d'évaluation
- Respira SiDocument80 pagesRespira SiIlaJako StefanaticPas encore d'évaluation
- Workplace Health Saf 2015 Darawad 9 17Document9 pagesWorkplace Health Saf 2015 Darawad 9 17IlaJako StefanaticPas encore d'évaluation
- Review Higginson PDFDocument4 pagesReview Higginson PDFSonalManePas encore d'évaluation
- Jurnal Seminar Kasus KK5ADocument14 pagesJurnal Seminar Kasus KK5AIlaJako StefanaticPas encore d'évaluation
- PoGo GymDef Cheat SheetDocument1 pagePoGo GymDef Cheat SheetFerni Panchito VillaPas encore d'évaluation
- Sen Çal KapımıDocument9 pagesSen Çal KapımıMa Gabriela Ojeda CasellaPas encore d'évaluation
- ReportDocument6 pagesReportLâmViênPas encore d'évaluation
- MAPEH Q4 ScriptDocument4 pagesMAPEH Q4 Scriptcharice maanoPas encore d'évaluation
- Learning Competencies: Table of SpecificationDocument2 pagesLearning Competencies: Table of Specificationyolanda renos0% (1)
- HCT Baniqued P.D.E. Paper1 Version3 FullpaperDocument8 pagesHCT Baniqued P.D.E. Paper1 Version3 FullpaperJoshua HernandezPas encore d'évaluation
- Checklist-Telephone - Mobile ExpenseDocument2 pagesChecklist-Telephone - Mobile ExpenseMichelle Domanacal UrsabiaPas encore d'évaluation
- Comparative Analysis of Motivation TheoriesDocument14 pagesComparative Analysis of Motivation TheoriesNomvelo MajolaPas encore d'évaluation
- Projects & Operations: IN: NE Power Systm ImprvmDocument5 pagesProjects & Operations: IN: NE Power Systm ImprvmGaurang PatelPas encore d'évaluation
- Zimbabwe National Code Ccorporate GovernanceDocument96 pagesZimbabwe National Code Ccorporate GovernanceHerbert NgwaraiPas encore d'évaluation
- Entrep Module 4 Q1 Week 4 1Document14 pagesEntrep Module 4 Q1 Week 4 1VirplerryPas encore d'évaluation
- Oral ComDocument2 pagesOral ComChristian OwlzPas encore d'évaluation
- The Spokesman Weekly Vol. 32 No. 39 May 30, 1983Document12 pagesThe Spokesman Weekly Vol. 32 No. 39 May 30, 1983SikhDigitalLibraryPas encore d'évaluation
- MAPEH 1 (4th Quarter)Document27 pagesMAPEH 1 (4th Quarter)JESSELLY VALESPas encore d'évaluation
- RLB Procuring For Value 18 July PDFDocument56 pagesRLB Procuring For Value 18 July PDFDaniel LixandruPas encore d'évaluation
- Rob Corry: People's Motion For Hearing To Determine Existence of Conflict-Free RepresentationDocument4 pagesRob Corry: People's Motion For Hearing To Determine Existence of Conflict-Free RepresentationMichael_Lee_RobertsPas encore d'évaluation
- Ealpha - Week 4 - Half A Day - ForeshadowingDocument2 pagesEalpha - Week 4 - Half A Day - ForeshadowingaalshehabPas encore d'évaluation
- Title: Speech of Corazon C. Aquino Before The US Congress: 3 Hours)Document3 pagesTitle: Speech of Corazon C. Aquino Before The US Congress: 3 Hours)Verna TrillanaPas encore d'évaluation
- Cooper - Formal Review of Karla Noles RaDocument6 pagesCooper - Formal Review of Karla Noles RaMark CooperPas encore d'évaluation
- Police Forces and The Administration of Justice in Tanzania.Document6 pagesPolice Forces and The Administration of Justice in Tanzania.Praygod Manase100% (2)