Académique Documents
Professionnel Documents
Culture Documents
PA 644 - M2 - Insomnia
Transféré par
kat0 évaluation0% ont trouvé ce document utile (0 vote)
17 vues27 pagesTitre original
PA 644 - M2 - Insomnia.pptx
Copyright
© © All Rights Reserved
Formats disponibles
PPTX, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PPTX, PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
17 vues27 pagesPA 644 - M2 - Insomnia
Transféré par
katDroits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PPTX, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 27
Pharmacotherapy of Insomnia
Gretchen L. Johnson, PharmD, BCPS
Insomnia
• Defined as difficulty falling asleep, difficulty
maintaining sleep or experiencing nonrestorative
sleep.
• Most common complaint in general medical
practice
• 40% of pts with chronic insomnia have a psych
diagnosis (depression, anxiety, substance abuse)
• 10-20% self-medicate with OTC meds or alcohol
Insomnia
• Three types of Insomnia
– Transient- lasting 2-3 nights (Ex. jetlag)
– Short-term- lasting < 3 months (Ex. situational)
– Chronic- lasting > 3 months
Common Causes of Insomnia
• Situational
– Work or financial stress, major life events,
interpersonal conflicts, jet lag or shift work
• Medical
– Cardiac: angina, arrhythmias, HF
– Respiratory: asthma, sleep apnea
– Chronic pain
– Endocrine: DM, hyperthyroidism
– GI: GERD, ulcers
– Neurologic: delirium, Parkinson’s, Seizures, RLS
– Pregnancy
Common Causes of Insomnia
• Psychiatric
– Mood disorders: depression, mania
– Anxiety disorders: GAD, OCD
– Substance abuse: alcohol, sedative-hypnotic withdrawal
• Drug-induced Insomnia
– Anticonvulsants
– Central adrenergic blockers
– Stimulants
– SSRIs, Bupropion
– Steroids
– Diuretics
Determining Management
• Determine if transient, short-term, or chronic
• Assess onset, duration and frequency of sx
• Assess effect on daytime functioning
• Assess for underlying causes
• Assess sleep hygiene
• Assess stress
Nonpharmacologic Treatment
• Cognitive behavioral therapy
– May be more effective than drugs in > 55yo
– Stimulus control, good sleep hygiene, cognitive
therapy, relaxation therapy
• Table 72-2 Stimulus Control and Sleep
Hygienehttp://accesspharmacy.mhmedical.co
m.suproxy.su.edu/ViewLarge.aspx?figid=1341
28156&gbosContainerID=0&gbosid=0
OTC options
• Antihistamines
– Diphenhydramine (Tylenol PM, Sominex)
– Doxylamine (Unisom)
• Herbal meds
– Melatonin
– Valerian
– Kava Kava
Nonprescription Treatments
• Antihistamines
– Watch for anticholinergic side effects- esp.
problematic in elderly
– Tolerance develops to sedative effects after 1 week
– Diphenhydramine- Pregnancy Category B; Lactation-
may dry up milk
• Herbals
– Little if any evidence of efficacy
• Melatonin may be helpful in jet lag
• Hepatotoxicity reported with Kava Kava and Valerian root
Prescription Treatments
• Benzodiapezines (BZDs)
– Temazepam (Restoril)
– Flurazepam (Dalmane)
– Triazolam (Halcion)
– Estazolam(Prosom)
– Quazepam (Doral)
• Non-BZD GABA-A agonists- “Z- hypnotics”
– Zolpidem (Ambien)
– Zaleplon (Sonata)
– Eszopiclone (Lunesta)
Prescription Treatments (cont’d)
• Melatonin receptor agonist
– Ramelteon (Rozerem)
• Sedating antidepresants
– Amitriptyline (Elavil)
– Doxepin (Silenor)
– Trazodone (Deseryl)
– Mirtazepine (Remeron)
Benzodiazepines
• MOA: GABA-A receptor agonists
• Controlled subtance
Drug Onset Duration T 1/2
Triazolam 30 min 2-4 hrs 2-5 hrs
Temazepam 60-120 min 8-10 hrs 9-12 hrs
Estazolam 60-120 min 8-10 hrs 10-20 hrs
Quazepam 30-60 min 8-10 hrs 40 hrs
Flurazepam 30-60 min 8-20 hrs 40-150 hrs
• Effective in dec. time to fall asleep and inc. total
sleep time
Benzodiazepines
• Do not use in:
– Pregnancy
– Substance abuse
– Untreated sleep apnea
• Avoid use with alcohol and other CNS
depressants
• Caution with driving or operating heavy
machinery
Benzodiazepines
• ADRs: daytime sedation, psychomotor incoordination, decreased
concentration and mental alertness, cognitive deficits, respiratory
depression
• ADRs are dose-related- use lowest effective dose
• Tolerance can develop
• Scheduled substance
– Can be habit forming
• Rebound insomnia can occur with abrupt DC
• Anterograde amnesia, an impairment of memory and recall of
events occurring after the dose is taken, can occur
• Can accumulate in the elderly
– Avoid BZDs with long t1/2- flurazepam and quazepam
– Inc. risk of falls and hip fracture
• Pregnancy Category X- cleft pallette, resp. depression
• Breastfeeding- not recommended
Non-BZD GABA-A agonists
• Zolpidem (Ambien)
• Zaleplon (Sonata)
• Eszopiclone (Lunesta)
• MOA: selective GABA-A receptor agonist
subtype 1
• Controlled substance
Non-BZD GABA-A agonists
• Zolpidem
– Formulations available: IR (Ambien), CR (Ambien CR), lingual
spray (Zolpimist), SL (Edular, Intermezzo)
Product Onset Duration
Zolpidem IR,Edular SL, 30 min 6 hours
Zolpimist
Zolpidem CR 30 min >6 hours
Intermezzo SL 30 min 4-6 hours
– Useful to initiate and maintain sleep; some residual effects
• Intermezzo for middle of the night wakenings- Need 4 hours of sleep left
Non-BZD GABA-A agonists
• Zaleplon (Sonata)
– Onset: 30 min Duration: 2 hours
– Useful to initiate sleep; Can take in middle of night but need 4
hr left in bed; Not for maintaining sleep unless redosed
– Least likely to cause next-day impairment or anterograde
amnesia
• Eszopiclone (Lunesta)
– Onset: 45 min Duration = 5-8 hr
– Useful to initiate sleep and maintain sleep
– No evidence of tolerance after 6 months of use
– ADR: unpleasant/metallic taste (20-33% incidence)
Zolpidem Dosing Change 2013
• FDA Recommends Lower Dose
• Reason:
– Morning blood levels in some pt (females) may be
high enough to impair activities requiring alertness –
driving
– Highest risk with ER forms and women eliminate the
drug more slowly than men
• Use 5mg vs. 10mg for IR; Use 6.25mg vs. 12.5mg
for CR
• Intermezzo (no change) already at a lower dosage
(11/2011)
Eszopiclone Dosing Change 2014
• FDA recommended lower dose
• Reason
– 3mg dose can impair driving ability, coordination,
and memory for over 11 hours
• Start with 1mg for all pts
– Do not exceed 2mg for elderly and 3mg for young
pts
Non-BZD GABA-A agonists
• High fat/heavy meal can delay absorption – delays onset
• CYP3A4 inhibitors can increase plasma levels
• Hepatic impairment may require lower doses
• Side effects:
– Headache
– Dizziness
– GI: nausea, dyspepsia
– Anterograde amnesia (high dose zolpidem)
• Withdrawal reactions uncommon but reported
• Pregnancy Category C; Breastfeeding: zolpidem compatible
BZD and Non-BZD GABA-A agonists
• FDA Labeling Changes
• Caution
– Anaphylaxis, facial angioedema
– Complex sleep behaviors- engaging in these activites while
not fully awake and with no recollection afterwards
• Sleep driving
• Sleep eating
• Phone calls
• Risk increased with concurrent alcohol use and doses above
maximum recommended
Ramelteon (Rozerem)
• Selective MT1 and MT2 receptor agonist
• Onset: 30 min T1/2= 1-2.6 hours
• Effective for dec. time to fall asleep
• Not effective for maintaining sleep
• ADRs: HA, dizziness, somnolence
• Not a controlled substance
– May be an option in substance abuse pts
• Pregnancy Category C; Breastfeeding- unknown
Sedating Antidepressants
• Alternatives for pt who cannot take BZD or if concommitant
depression
• Improve sleep in depression with stimulating SSRI or bupropion
– Mostly see Trazodone used
• Doses used for insomnia are not effective for treating depression
• Amitriptyline 10-50mg Qhs; Doxepin (Silenor®) 3-6mg Qhs
– Disadvantages
• Anticholinergic side effects, adrenergic blockade (orthostatic
hypotension), cardiac conduction problems, daytime
sedation
• Trazodone 25-150mg QHS
– Watch for orthostatic hypotension, priapism
• Mirtazapine 7.5 – 30mg QHS
– Watch for daytime sedation, weight gain
Suvorexant(Belsomra)
• New class of sleep agent
• MOA: orexin receptor antagonist
– Orexins are involved with promoting wakefulness
so antagonising their effect would cause sedation
• Schedule IV
• Same precautions about combining with
alcohol and other sedating drugs and risk for
impairment in driving and other activities the
next day
Treatment of Insomnia
• Stepwise approach to select hypnotic
– ? Type of insomnia
• Difficulty initiating sleep
• Difficulty maintaining sleep/early morning awakening
– ? Duration
– ? Etiologies
• Sleep apnea, psychiatric/medical issues
– ? Sleep habits
– Substance abuse history
Select agents based on symptoms, kinetic and ADR
profile
Clinical Practice Guideline
General Treatment Approach
1. Short-intermediate acting BZD, Non-BZD RA or ramelteon
Ex. Zolpidem, eszoplicone, zaleplon, temazepam
2. Alternate short-intermediate acting BZD, Non-BZD RA or
ramelteon
3. Sedating antidepressant
Ex. Amitriptyline, trazodone, doxepin, mirtazepine
4. Combined BzRA or ramelteon + sedating antidepressant
5. Other sedating agents- with appropriate comorbid
conditions
Ex. Quetiapine, gabapentin
Journal of Clinical Sleep Medicine, Vol. 4, No. 5, 2008
Algorithm
Adapted and Used With Permission from Mitsi Lizer, Pharm.D.
Hypnotic Selection
DFA DMS MNA
Ramelteon, Zolpidem, Zaleplon
triazolam, Eszopiclone,
zaleplon, zolpidem Temazepam Intermezzo
DFA: Difficulty falling asleep; DMS: maintaining sleep: MNA: middle of the night awakening
Vous aimerez peut-être aussi
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Matary Surgical Anatomy 2013 AllTebFamily ComDocument320 pagesMatary Surgical Anatomy 2013 AllTebFamily Comkat100% (2)
- TRP Surgery Study GuideDocument27 pagesTRP Surgery Study GuidekatPas encore d'évaluation
- General Surgical InstrumentsDocument96 pagesGeneral Surgical Instrumentsviki28mb90% (29)
- Attia General Surgery Review ManualDocument158 pagesAttia General Surgery Review Manualbphage100% (2)
- Jim's Surgery NotecardsDocument20 pagesJim's Surgery NotecardsFabian Ramirez HincapiéPas encore d'évaluation
- Key Topics in General SurgeryDocument455 pagesKey Topics in General SurgeryAlbano Hall75% (16)
- Topnotch Surgery Reviewer PDFDocument81 pagesTopnotch Surgery Reviewer PDFkat0% (1)
- Midpoint Preceptor Evaluation of StudentDocument2 pagesMidpoint Preceptor Evaluation of StudentkatPas encore d'évaluation
- Matary Surgitoons General 2013Document155 pagesMatary Surgitoons General 2013Raouf Ra'fat Soliman100% (10)
- Head Toe Toe Chapter II - 3Document279 pagesHead Toe Toe Chapter II - 3Yonico Yudha Pranata100% (1)
- PA 644 - M2 LecturesDocument735 pagesPA 644 - M2 LectureskatPas encore d'évaluation
- Jim's Surgery Progress Note TemplateDocument1 pageJim's Surgery Progress Note TemplatekatPas encore d'évaluation
- USMLE PathognomicsDocument9 pagesUSMLE PathognomicsMatt McGlothlin94% (18)
- PANCE Prep Pearls Pulmonary Questions PDFDocument8 pagesPANCE Prep Pearls Pulmonary Questions PDFkatPas encore d'évaluation
- PA 644 - M2 LecturesDocument412 pagesPA 644 - M2 LectureskatPas encore d'évaluation
- Prescriptions Examples PDFDocument2 pagesPrescriptions Examples PDFkat100% (1)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- DEAL12Document128 pagesDEAL12MutmainahPas encore d'évaluation
- Sop PKM TK - JambuDocument24 pagesSop PKM TK - JambuSilvia Rif'ahPas encore d'évaluation
- Modified From The List Produced by The Njardarson Group (The University of Arizona)Document1 pageModified From The List Produced by The Njardarson Group (The University of Arizona)Amihan100% (1)
- Label ObatDocument31 pagesLabel ObatAndiTenriBayangPas encore d'évaluation
- DDD 2017 SectiiDocument14 pagesDDD 2017 SectiinicoletagenovevaPas encore d'évaluation
- Rs Pena 98: Jl. Pemuda Pengasinan N0.36 Kec Gn. Sindur Bogor Telp: (021) 7587 4401,-FaxDocument60 pagesRs Pena 98: Jl. Pemuda Pengasinan N0.36 Kec Gn. Sindur Bogor Telp: (021) 7587 4401,-Faxrichard fernandoPas encore d'évaluation
- Anxiolytics & Hypnotics Drugs: Chapter FiveDocument21 pagesAnxiolytics & Hypnotics Drugs: Chapter FiveabrihamPas encore d'évaluation
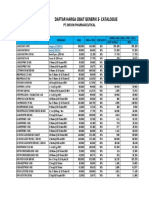
- Daftar Harga Ogb Divisi Jaguar: Per-1 Maret 2020Document1 pageDaftar Harga Ogb Divisi Jaguar: Per-1 Maret 2020AsmorowatiPas encore d'évaluation
- Siap Print Untuk SimulasiDocument3 pagesSiap Print Untuk SimulasiRossa patria NandaPas encore d'évaluation
- Api List of SLDocument2 pagesApi List of SLpopoPas encore d'évaluation
- ProductosDocument4 pagesProductoscloris gilPas encore d'évaluation
- Daftar Harga E-Catalogue Infion GenerikDocument1 pageDaftar Harga E-Catalogue Infion GenerikInstalasi FarmasiPas encore d'évaluation
- Updated List of Drugs and Medicines For Maximum Retail Price (MRP)Document10 pagesUpdated List of Drugs and Medicines For Maximum Retail Price (MRP)dhonnaPas encore d'évaluation
- Daftar Obat ProlanisDocument18 pagesDaftar Obat ProlanisMas EmPas encore d'évaluation
- 4173laporan BTK 26-31 Desember 2017Document128 pages4173laporan BTK 26-31 Desember 2017tandun nlmPas encore d'évaluation
- Aldi Aryanto SPESIALITE OBAT KARDIOVASKULERDocument5 pagesAldi Aryanto SPESIALITE OBAT KARDIOVASKULERAldi AryantoPas encore d'évaluation
- Lista TAB 01.02.2018Document40 pagesLista TAB 01.02.2018Botezatu VilusaPas encore d'évaluation
- Antiviral Drug: Classification and Mechanism of ActionDocument1 pageAntiviral Drug: Classification and Mechanism of ActionNikita sharmaPas encore d'évaluation
- GN BN Part IDocument2 pagesGN BN Part ICarla Flor LosiñadaPas encore d'évaluation
- Bahan Dri KhemedDocument7 pagesBahan Dri KhemedgustiPas encore d'évaluation
- AnxiolyticsDocument8 pagesAnxiolyticsHengky_FandriPas encore d'évaluation
- Drug Prefixes and SuffixesDocument12 pagesDrug Prefixes and SuffixesKENNETH GENER JAMES SOMERA0% (1)
- SO lt.2Document180 pagesSO lt.2Armyta AgustinaPas encore d'évaluation
- Daftar Dosis Dan Sediaan Obat AnakDocument5 pagesDaftar Dosis Dan Sediaan Obat AnakAzwin Abdul JabbarPas encore d'évaluation
- Ofertas 170122Document27 pagesOfertas 170122VENTAS GIPas encore d'évaluation
- Anticholinergics Study Drug ListDocument1 pageAnticholinergics Study Drug ListDrima Edi100% (1)
- BASIC DefectaDocument7 pagesBASIC Defectaafifah klinikPas encore d'évaluation
- NO Produk Isi/Box HNA Kode Produk: Penawaran Harga Rs Harapan Keluarga Pt. Hexpharm Jaya 2021Document6 pagesNO Produk Isi/Box HNA Kode Produk: Penawaran Harga Rs Harapan Keluarga Pt. Hexpharm Jaya 2021YENNYPas encore d'évaluation
- PremedicationDocument9 pagesPremedicationdrhiwaomer100% (3)
- Atc DDD Tablet Buat Pa IjalDocument57 pagesAtc DDD Tablet Buat Pa IjalAriesta PerwitasariPas encore d'évaluation