Académique Documents
Professionnel Documents
Culture Documents
Acls Review 2015
Transféré par
Patricia0 évaluation0% ont trouvé ce document utile (0 vote)
22 vues26 pagesACLS Review
Copyright
© © All Rights Reserved
Formats disponibles
PPT, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentACLS Review
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PPT, PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
22 vues26 pagesAcls Review 2015
Transféré par
PatriciaACLS Review
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PPT, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 26
Who goes to the code
• Interns, senior residents, AIs, and 3rd year
medical students on Long Call on wards and in
MICU
• DACR/VACR/NACR
• Anesthesia team
• Respiratory Therapists
• Critical care nurses (from MICU/CICU)
• Critical care pharmacist (sometimes)
Who runs the code?
• First resident on the scene, or
DACR/VACR/NACR
• The leader of the code assigns roles and
responsibilities to the other residents and
interns available
Roles during the code
• Stabilizing/managing airway
• Line for chest compressions
• Recording timing of events
• Managing code cart/ Medication administration
• Checking labs and past medical history, telemetry
• Obtaining emergency access
• Thinking through Hs and Ts
• Calling the patient’s family
Code Blue
You are the Naff intern on call, working on notes
in the Naff team room. Code Blue is called for
a patient on Lakeside 20. Your senior is MIA.
You run down the hall and are the first on the
scene. What do you do?
Scenario 1
• You feel a thready femoral pulse, the patient
feels tachycardic
• Automatic blood pressure cuff is not reading
• Patient is agonal breathing, not responding to
verbal or painful stimuli
• The nurses look to you and say “Doctor, what
do we do?”
• On arrival, you do a quick initial assessment while
assessing his responsiveness and vital signs and
immediately instruct someone to begin
compressions.
• While compressions are occurring you ask the
nurse to apply pads and electrodes to the patient
to analyze the rhythm.
• In addition, you ask that oxygen be applied to the
patient
• You ask about any complaints the patient may
have had and find that minutes ago he was
complaining of chest pain, palpitations, and
dizziness.
• Being a very keen intern, you recognize this may
be Acute Coronary Syndrome causing arrest.
Cardiac Arrest, 4 rhythms
• As you pause during compressions you analyze the
rhythm… the patient is in Ventricular Fibrillation
• The DACR runs into the room, you notify him/her of
the patient’s rhythm and
• ANALYZE.. CLEAR…SHOCK DELIVERED
• Resume CPR! Wait to reanalyze the rhythm after the
next round of CPR
• The patient receives a dose of Epinephrine in addition
to another shock and has conversion to sinus rhythm.
He has ROSC. His vitals begin to improve and he is
rushed to the Cardiac Catherization Lab.
• Nice Work!
High quality CPR is key
• Rate approx 100/min
• Compression depth >2
inches (5cm) in adults
• Allow complete chest
recoil after each
compression
• Minimize interruptions
• Rotate every 2 minutes
Scenario 2
• One of your many pagers on Intern Nightfloat
goes off.
• “There’s a Code White on your patient in
Lakeside 55 her heart rate is a little low and
she’s feeling dizzy”
• You ask the nurse to get a full set of vitals as
you head towards the patient’s room.
• As you’re headed over you hear the overhead
announcement “CODE BLUE, CODE BLUE,
CODE BLUE..LAKESIDE 55”
• You arrive at the patient’s room and the nurse
informs you that the patient’s HR was 60-70’s
during the day but suddenly decreased from 48
to 35bpm.
• Current vitals: HR 35bpm, SBP 70/DBP is
undetectable RR 16/min, and O2 saturation 93%.
• The patient was initially complaining of
lightheadedness but now is more lethargic.
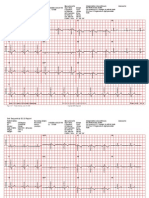
• You take a look at the EKG that was obtained.
• You request oxygen be applied to the patient and
the pads for transcutaneous pacing be applied.
• Just as you are doing so, additional help arrives
and your Nightfloat senior assists you.
• Atropine is obtained from the crashcart and the
patient is bolused 0.5mg.
• The patient’s HR slightly improves to 49bpm but
he remains somewhat confused and lethargic.
• Transcutaneous pacing is started with a target HR
of 60bpm. She begins to wake up and her BP
improves to 110/57.
• EP is consulted and the patient receives a
transvenous and ultimately an implanted
pacemaker.
Last Scenario
• You are on Hellerstein waiting to sign out at
630 pm on a Sunday when you’re paged about
a patient with past hx of SVT here for CP now
has a HR of 160.
• BP 125/80, narrow complex tachycardia as
below
• After attempting vagal maneuvers
(unsuccessful) you give adenosine 6mg IV
push, and then 12 mg IV push
• Now the patient develops severe chest pain,
He 220, BP not obtainable, pulse weak. The
patient begins losing consciousness. What do
you do next?
• Synchronized cardioversion is unsuccessful.
Patient now is pulseless and unconscious.
What next? Time to shock! (unsynchronized
120-200 J)
Synchronized vs unsynchronized
cardioversion
Synchronized Unsynchronized
Low energy shock High energy shock
delivers shock w/ peak delivers as soon as
of QRS shock button is pushed
Indications: unstable A Indications: pulseless
fib, A flutter, SVT VT/VF
If shock occurs on t-wave,
high likelihood of VF
• After 5 cycles of CPR, the rhythm check
suggests a second shock. Now with 200 J.
Which medications should you be giving?
• Epinephrine 1mg IV q3min and/or vasopressin
40 U IV to replace first or second epi dose
• Amiodarone after 3rd shock in pulseless VT
(300 mg IV x1, then consider 150 mg IV x1
• SROC! The patient was intubated by
anesthesia at the scene, and is not responding
to verbal commands. Patient transported to
CICU. What post cardiac arrest intervention
would this patient benefit from?
What Is ACLS?
• ACLS guidelines first published 1974 by AHA, most
recent update 2010
• A series of interventions for urgent treatment of
cardiac arrest, stroke, and life threatening medical
emergencies
• Several algorithms for VF/Pulseless VT, Bradycardia,
Suspected Stroke
• An essential part of using the algorithm correctly is to
search for and correct potentially reversible causes of
arrest
• Performing high quality CPR, identifying arrhythmias
and understanding the pharmacology behind key drugs
are central to ACLS.
H’s and T’s
Treatable causes of cardiac arrest
• Hypoxia • Thrombosis
• Hypovolemia (pulmonary)
• Hydrogen ion (acidosis) • Thrombosis (coronary)
• Hypokalemia • Tamponade
• Hyperkalemia • Tension pneumothorax
• Hypothermia • Toxins
Things to discuss with patients
• All patients admitted to the hospital should be
asked about their code status
• It’s important to discuss the morbidity
associated with ACLS
• Statistics regarding survival after arrest
• Adverse outcomes of CPR and Advanced
Airway Support
Vous aimerez peut-être aussi
- ACLS Review Guide for Cardiac Arrest Scenarios and TreatmentDocument29 pagesACLS Review Guide for Cardiac Arrest Scenarios and TreatmentJB Reyes100% (2)
- Cardiac Arrest - BLS-ACLS - Dr. KhaledDocument93 pagesCardiac Arrest - BLS-ACLS - Dr. Khaledrony ghoshPas encore d'évaluation
- Bls (Basic Life Support) & Acls (Advanced Care Life Support) : PresenterDocument135 pagesBls (Basic Life Support) & Acls (Advanced Care Life Support) : PresenterbernarduswidodoPas encore d'évaluation
- Bls (Basic Life Support) & Acls (Advanced Care Life Support) : PresenterDocument135 pagesBls (Basic Life Support) & Acls (Advanced Care Life Support) : PresenterbernarduswidodoPas encore d'évaluation
- Reviewer 2Document15 pagesReviewer 2chaSeph100% (2)
- Theme 1 1Document97 pagesTheme 1 1lela ndociPas encore d'évaluation
- Emed - Special Resuscitation Situations (Doc Vito)Document55 pagesEmed - Special Resuscitation Situations (Doc Vito)Princess Cate MercadoPas encore d'évaluation
- Special Resuscitation Situations: Stroke, Hypothermia, Anaphylaxis, Drowning, Trauma, PregnancyDocument55 pagesSpecial Resuscitation Situations: Stroke, Hypothermia, Anaphylaxis, Drowning, Trauma, PregnancyPrincess Cate MercadoPas encore d'évaluation
- Cardioplumonary RDocument40 pagesCardioplumonary RABREHAM BUKULOPas encore d'évaluation
- Ncm106 Week 15 IcuDocument15 pagesNcm106 Week 15 IcuMichelle MallarePas encore d'évaluation
- Basic Life SupportDocument24 pagesBasic Life SupporthelmismutPas encore d'évaluation
- 5 Shock PPT EnglishDocument77 pages5 Shock PPT EnglishKessi VikaneswariPas encore d'évaluation
- Cardiac ArrestDocument40 pagesCardiac ArrestApriliani Nur Puspita SariPas encore d'évaluation
- New HematologyOncology FAE2016Document108 pagesNew HematologyOncology FAE2016omarPas encore d'évaluation
- Samuel Case 1B KGDDocument63 pagesSamuel Case 1B KGDSamuel Sebastian SirapanjiPas encore d'évaluation
- Algorithm For Helping With Cardiac ArrestDocument52 pagesAlgorithm For Helping With Cardiac ArrestOlga GoryachevaPas encore d'évaluation
- BLS and ACLS Case ScenariosDocument35 pagesBLS and ACLS Case ScenariosrajPas encore d'évaluation
- Lectii ScoalaDocument43 pagesLectii ScoalaGaudiMateiPas encore d'évaluation
- Ekg QuestionsDocument18 pagesEkg QuestionsEvidence Chaibva100% (1)
- Chapter 72. Case StudiesDocument40 pagesChapter 72. Case Studiesstawberry shortcake100% (1)
- IU Health ACLS Study GuideDocument8 pagesIU Health ACLS Study Guideeng78inePas encore d'évaluation
- Arrhythmia, Pericardial and Myocardial Diseases (Dr Praveen) 2Document44 pagesArrhythmia, Pericardial and Myocardial Diseases (Dr Praveen) 2hashini1997nisansalaPas encore d'évaluation
- Principles of CPR and CARDIAC MASSAGEDocument34 pagesPrinciples of CPR and CARDIAC MASSAGEBharat BhushanPas encore d'évaluation
- Virtual Clinical Prep For Cardiopulmonary ArrestDocument1 pageVirtual Clinical Prep For Cardiopulmonary ArrestBridgette RandolphPas encore d'évaluation
- Hemodynamic Unstable Patient Following ArrhythmiaDocument30 pagesHemodynamic Unstable Patient Following Arrhythmialew chin hongPas encore d'évaluation
- Advanced Cardiac Life SupportDocument44 pagesAdvanced Cardiac Life Supporthafidh_hanifuddinPas encore d'évaluation
- Shock & Fluid Therapy KSKBDocument55 pagesShock & Fluid Therapy KSKBArnold Daniel100% (1)
- Advanced Cardiovascular Life Support (Acls)Document45 pagesAdvanced Cardiovascular Life Support (Acls)Erinne DefrianiPas encore d'évaluation
- Advanced Life Support in Perspective: - Chain of SurvivalDocument34 pagesAdvanced Life Support in Perspective: - Chain of SurvivalManju PriyaPas encore d'évaluation
- ACLS Pulmonary Edema and Stroke AlgorithmsDocument34 pagesACLS Pulmonary Edema and Stroke AlgorithmsMuhammad SafaatPas encore d'évaluation
- Immediate life supportDocument63 pagesImmediate life supportmatrixkhalifa9955Pas encore d'évaluation
- Cardiovascular Problems of The Adult ClientDocument16 pagesCardiovascular Problems of The Adult ClientMarylle AntonioPas encore d'évaluation
- Electrophysiology Study and Cardiac AblationDocument29 pagesElectrophysiology Study and Cardiac AblationBat ManPas encore d'évaluation
- CCU Clinical GuidelinesDocument63 pagesCCU Clinical GuidelinesHAMMYER ALROKHAMIPas encore d'évaluation
- CPR 2014 SeminarDocument43 pagesCPR 2014 SeminarMinale MenberuPas encore d'évaluation
- June 2014 Questions Returned From Candidates - Thank You: Long Case 1Document14 pagesJune 2014 Questions Returned From Candidates - Thank You: Long Case 1karan270Pas encore d'évaluation
- ACLSDocument61 pagesACLSmgthida935100% (1)
- NeuroemDocument51 pagesNeuroemJameston BostrePas encore d'évaluation
- Acls 30-10-23Document63 pagesAcls 30-10-23lakshmiPas encore d'évaluation
- Basics of AnesthesiaDocument34 pagesBasics of Anesthesianicolinna2000yahoo.comPas encore d'évaluation
- Medically ComprmisedDocument73 pagesMedically Comprmisedhaitham192002Pas encore d'évaluation
- Advanced Cardiac Life SupportDocument50 pagesAdvanced Cardiac Life SupportBalemlay HailuPas encore d'évaluation
- SCAI Shock Classification DeckDocument22 pagesSCAI Shock Classification DeckJimmy JimmyPas encore d'évaluation
- Emergency medical care test questionsDocument28 pagesEmergency medical care test questionsshilpa sekhar278Pas encore d'évaluation
- Code Blue Simulation GuideDocument13 pagesCode Blue Simulation GuideStephanie LiauPas encore d'évaluation
- Dvanced Ardiovascular Ife Upport: A C L SDocument10 pagesDvanced Ardiovascular Ife Upport: A C L SErica Jane100% (1)
- Post Intubation HypotensionDocument37 pagesPost Intubation Hypotensionfifa_0304535100% (1)
- Advanced Cardiac Life SupportDocument42 pagesAdvanced Cardiac Life SupportDennis MiritiPas encore d'évaluation
- Early Warning ScoresDocument14 pagesEarly Warning ScoresmuchtarPas encore d'évaluation
- ACLS SubhankarDocument87 pagesACLS SubhankarMarc Andreo MalalaPas encore d'évaluation
- Pacing NTI 2015Document35 pagesPacing NTI 2015wastionPas encore d'évaluation
- Cardiology NotesDocument13 pagesCardiology NotesFreeNursingNotes78% (9)
- Low BP / fast pulse: Causes and management of shockDocument64 pagesLow BP / fast pulse: Causes and management of shockRachelMokPas encore d'évaluation
- Management of Cardiac ArrestDocument40 pagesManagement of Cardiac ArrestMark Francis NaniaPas encore d'évaluation
- Acls Cheat Sheet PDFDocument3 pagesAcls Cheat Sheet PDFDarren Dawkins100% (4)
- Ventricular Arrhythmias EP Overview MedtronicDocument44 pagesVentricular Arrhythmias EP Overview Medtronicinu_upPas encore d'évaluation
- Coronary Artery DiseaseDocument32 pagesCoronary Artery DiseasecjissamPas encore d'évaluation
- Basic Dysrhythmias: Scott Prewitt, RN, MSN, APRN-BCDocument42 pagesBasic Dysrhythmias: Scott Prewitt, RN, MSN, APRN-BCtuffie85Pas encore d'évaluation
- Advance Cardiac Life Support: Short, Sweet and to the PointD'EverandAdvance Cardiac Life Support: Short, Sweet and to the PointÉvaluation : 3 sur 5 étoiles3/5 (2)
- Universal PrecautionDocument48 pagesUniversal PrecautionThirugnanaThiru100% (1)
- HPV Screening AlgorithmsDocument6 pagesHPV Screening AlgorithmsPatriciaPas encore d'évaluation
- HPV Screening AlgorithmsDocument6 pagesHPV Screening AlgorithmsPatriciaPas encore d'évaluation
- Infection Control Session 2013Document86 pagesInfection Control Session 2013PatriciaPas encore d'évaluation
- Who Aids 2 PDFDocument15 pagesWho Aids 2 PDFPatriciaPas encore d'évaluation
- Improving Patient Safety, Safety CultureDocument325 pagesImproving Patient Safety, Safety Cultureo.atik100% (2)
- Paediatric Cleaning Toys Games and Play Equipment On The Paediatric WardDocument8 pagesPaediatric Cleaning Toys Games and Play Equipment On The Paediatric WarddidikPas encore d'évaluation
- Patient Satisfaction and Benefts of Music Therapy Services To Manage Stress and Pain in The Hospital Emergency DepartmentDocument25 pagesPatient Satisfaction and Benefts of Music Therapy Services To Manage Stress and Pain in The Hospital Emergency DepartmentBapak Sunaryo SPBU100% (1)
- Parkinson in Adult NICE Guideline 2017Document30 pagesParkinson in Adult NICE Guideline 2017yustikaPas encore d'évaluation
- Washing raw chicken increases risk of food poisoningDocument3 pagesWashing raw chicken increases risk of food poisoningsecretPas encore d'évaluation
- Breast Mass GuideDocument20 pagesBreast Mass GuideFabian Ramirez HincapiéPas encore d'évaluation
- OB MedsDocument19 pagesOB Medsohsnapitslei100% (2)
- ImdrfDocument30 pagesImdrfborrellanoPas encore d'évaluation
- KELOMPOK 1 - RS2 - PRAKTIK BAHASA INGGRIS DetailDocument12 pagesKELOMPOK 1 - RS2 - PRAKTIK BAHASA INGGRIS Detailseren agathaPas encore d'évaluation
- Transitional Care: DR - Vinoli.S.G Professor HOD Medical Surgical Nursing Dept Universal College of Nursing BangaloreDocument15 pagesTransitional Care: DR - Vinoli.S.G Professor HOD Medical Surgical Nursing Dept Universal College of Nursing BangalorevinoliPas encore d'évaluation
- Attachments For Removable Partial Dentures Prostho 6Document10 pagesAttachments For Removable Partial Dentures Prostho 6Melika DPas encore d'évaluation
- Warning Letters - Jubilant Generics Limited 3 - 6 - 19 PDFDocument4 pagesWarning Letters - Jubilant Generics Limited 3 - 6 - 19 PDFsudheerPas encore d'évaluation
- Universal ECG Sample ReportsDocument6 pagesUniversal ECG Sample ReportsHemant Soni100% (1)
- Assignment Topic: Nursing Records and Reports Subject: Nursing Managemnt Date of Submission: 27Document21 pagesAssignment Topic: Nursing Records and Reports Subject: Nursing Managemnt Date of Submission: 27Priyanjali Saini100% (3)
- ATROVENTDocument25 pagesATROVENTNúñez AlejandroPas encore d'évaluation
- Advocacy PaperDocument3 pagesAdvocacy Paperapi-485309966Pas encore d'évaluation
- NCP EpilepsyDocument1 pageNCP EpilepsyManpreet ToorPas encore d'évaluation
- Master ResumeDocument3 pagesMaster ResumeJeanie WalkerPas encore d'évaluation
- Bahan Local FlapDocument72 pagesBahan Local FlapChandrawati PramanaPas encore d'évaluation
- WRHA Compensation Disclosure 2015Document336 pagesWRHA Compensation Disclosure 2015Tessa VanderhartPas encore d'évaluation
- Stroke LectureDocument48 pagesStroke Lecturebereket gashu67% (6)
- Sports Injury Assessment PDFDocument43 pagesSports Injury Assessment PDFPatricia Andrea Acevedo ArancibiaPas encore d'évaluation
- ADC Part 1 - TG Keynotes II v1.0 PDFDocument17 pagesADC Part 1 - TG Keynotes II v1.0 PDFDrSaif Ullah KhanPas encore d'évaluation
- Case Discussion Hanging - LatestDocument27 pagesCase Discussion Hanging - LatestSukrutha Sahu Jaya0% (1)
- Surgical Case Study: CranioplastyDocument50 pagesSurgical Case Study: Cranioplastyrhia casinillo100% (8)
- Doctors Nurses Overcome Workplace HierarchiesDocument6 pagesDoctors Nurses Overcome Workplace HierarchiesAndres CarreraPas encore d'évaluation
- CGHS Empaneled HospitalsDocument61 pagesCGHS Empaneled HospitalsAshutosh SaxenaPas encore d'évaluation
- Aplastic AnemiaDocument7 pagesAplastic Anemianeil052288% (8)
- APSIC BrochureDocument2 pagesAPSIC BrochurekindyPas encore d'évaluation