Académique Documents
Professionnel Documents
Culture Documents
Peripheral Nerve Blocks in The Management of Postoperative Pain: Challenges and Opportunities
Transféré par
inha0 évaluation0% ont trouvé ce document utile (0 vote)
6 vues18 pagesJURNAL Blok saraf perifer dalam manajemen nyeri pasca operasi: tantangan dan peluang
Titre original
PERIPHERAL NERVE BLOCKS IN THE MANAGEMENT OF POSTOPERATIVE PAIN: CHALLENGES AND OPPORTUNITIES
Copyright
© © All Rights Reserved
Formats disponibles
PPTX, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentJURNAL Blok saraf perifer dalam manajemen nyeri pasca operasi: tantangan dan peluang
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PPTX, PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
6 vues18 pagesPeripheral Nerve Blocks in The Management of Postoperative Pain: Challenges and Opportunities
Transféré par
inhaJURNAL Blok saraf perifer dalam manajemen nyeri pasca operasi: tantangan dan peluang
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PPTX, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 18
Diyah S Kurnia
105505420017
Dibawakan dalam rangka tugas kepaniteraan klinik bagian Ilmu Bedah)
FAKULTAS KEDOKTERAN
UNIVERSITAS MUHAMMADIYAH MAKASSAR
2019
Abstract
Peripheral nerve blocks (PNBs) are increasingly used
as a component of multimodal analgesia and may be
administered as a single injection (sPNB0 or
continuous infusion via a perineural cathteter
(cPNB). We undertook a qualititative review
focusing on sPNB and cPNB with regard to benefits,
risks, and opportunities for optimizing patient care.
Abstract
Meta-analyses of randomized controlled trials have
shown superior pain control and reductions in
opioid consumption in patients receiving PNB
compared with those receiving in- travenous opioids
in a variety of upper and lower extremity surgical
procedures. cPNB has also been asso- ciated with a
reduction in time to discharge readiness compared
with sPNB
1. Introduction
Multimodal analgesia refers to the use of
combinations of analgesics acting via different
mechanisms and thus taking ad- vantage of additive
or synergistic activity while minimizing adverse
events with larger doses of a single analgesic
The benefits of PNBs are numerous and include improve-
ment in clinical, economic, and humanistic outcomes
Table 1 Benefits of PNB as a component of
multimodal post-operative anagesia regimen
Improvement in postoperative pain control and reduction in the
use of opioids [2-7]
• Reduction in hospital length of stay [10,11]
• Prevention of hospital readmissions [16]
• Reduction in postoperative nausea and vomiting [2]
• Faster movement to phase 2 recovery and/or postanesthesia
care unit bypass [13]
• Earlier participation in physical therapy [10]
• Improved patient satisfaction [2]
PNBs are now a common component of analgesia for
both upper extremity (eg, brachial plexus block
using intersca- lene, supra- or infraclavicular, and
axillary nerve approaches) [14] and lower extremity
(eg, lumbar plexus, femoral, sciatic, and popliteal
sciatic blocks, among others) procedures [15].
Technical advances include the use of ultrasound-
guided nee- dle placement and the movement from
the use of single injec- tions of local anesthetic
(single-shot PNB [sPNB]) to continuous infusion
administered using a perineural catheter (continuous
PNB [cPNB]).
The objective of this article is to review the recent
literature on sPNB and cPNB as a component of
multimodal postopera- tive analgesia, highlighting
benefits, risks, and opportunities for optimizing
patient care. A search of the literature was per-
formed using PubMed, including citations published
up to March 2015.
2. Clinical efficacy of PNB
2.1. PNB vs opioids
The efficacy of sPNB in improving short-term pain
control has been shown in a number of upper and lower
extremity sur- gical procedures. In a Cochrane review of
randomized trials in patients undergoing major knee
surgery,
In a sys- tematic review of 13 randomized trials
comparing FNB to sham or placebo blocks in patients
undergoing ACL surgery, Mall and Wright [17] found
that pain relief was greater with FNB in only 5 trials and
that opioid-related nausea and seda- tion occurred less
frequently in the FNB group in only 1 trial.
2.2. cPNB vs sPNB
Administration of local anesthetics via continuous
infusion allows for a duration of analgesia
significantly longer than that of a single injection. In
a pooled analysis of 21 studies compar- ing cPNB to
sPNB for postoperative analgesia, worst visual
analogue scale pain scores and pain at rest were
significantly lower in patients receiving cPNB on
postoperative days 0, 1, and 2 but not day 3 [19].
Opioid consumption was also signif- icantly reduced
in the cPNB group on days 1 and 2
3. Risks and limitations of
PNB
Potential risks of PNB, regardless of technique or
block lo- cation, include vascular puncture and
bleeding, nerve damage, and local anesthetic
systemic toxicity
Neurologic complications are of particular concern
because the duration of symptoms can extend for
weeks or months after surgery
Signs and symptoms of LAST are dose dependent
and range from metallic taste, tinnitus, and perioral
numbness to seizure, cardiac arrest, and death
3.1. Single-shot PNB
As such, sPNB is best suited for surgi- cal procedures
in which postoperative pain is not expected to ex-
ceed 12-24 hours in duration; otherwise, patients are
at risk for significant rebound pain after discharge
Thus, alternative methods of overcoming these
limitations for surgical procedures with pain
persisting past the first postoperative day are
required
3.2. Continuous PNB
The incidence of cPNB complications is highly dependent
on the insertion technique and block location, and thus, it
is difficult to make generalizations across studies. Minor
compli- cations include catheter dislodgement,
obstruction, and fluid leakage at the catheter site [46].
Rates of catheter dislodgment in studies of volunteers
engaging in activities of daily living were as high as 25%
[47]. One study found that 2 of the 9 pa- tients with
dislodged interscalene catheters were readmitted to the
hospital, with the remaining 7 patients experiencing no
sig- nificant pain [42].
Table 2 Infection-related complications of
continuous PNB
Complication Incidence from Notes
observational studies
Colonization 6%-69% Most common
Inflammation 3%-9.6% organisms are
Infection 0%-3% coaguase-negative
Staphylococcus; others
include gram-negative
bacilli, including
Eschericia coli and
Enterococcus, and S
aureus.
4. Opportunities
The ideal PNB technique would have a duration of action
sufficient to provide pain relief for the most intense
period of postoperative pain but not result in a dense
motor block that could be unpleasant to the patient or
lead to safety issues such as falls. Moreover, the risk of
infection, neurologic complica- tions, bleeding, and LAST
should be minimized to the extent possible. The technique
should be easy to perform and thus in- dependent of the
technical skill of the anesthesiologist and with minimal
chance of failed procedures. Finally, the ideal PNB
technique should be convenient for patients and easy to
manage in the postoperative period.
Acknowledgments
Preparation of this manuscript was sponsored by
Pacira Pharmaceuticals, Inc.
Vous aimerez peut-être aussi
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Anesth MCQDocument810 pagesAnesth MCQJescel-Anne Janea MagatPas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Varicose Vein and Its Homeopathic Cure - DR Bashir Mahmud ElliasDocument8 pagesVaricose Vein and Its Homeopathic Cure - DR Bashir Mahmud ElliasBashir Mahmud Ellias100% (2)
- Nd:YAG Laser Capsulotomy OverviewDocument5 pagesNd:YAG Laser Capsulotomy OverviewinhaPas encore d'évaluation
- 6 Urinary EliminationDocument5 pages6 Urinary EliminationkhautedamePas encore d'évaluation
- What Is Irritable Bowel Syndrome (IBS) ?Document12 pagesWhat Is Irritable Bowel Syndrome (IBS) ?inhaPas encore d'évaluation
- Bimbingan UKMPPD (UKDI) - THTDocument152 pagesBimbingan UKMPPD (UKDI) - THTAvicenna_MSC100% (7)
- Abnormal Labour: Perceptor: Dr. Nurul Islamy, M. Kes., Sp. OGDocument54 pagesAbnormal Labour: Perceptor: Dr. Nurul Islamy, M. Kes., Sp. OGramadhiena destia100% (1)
- Community Health Nursing PDFDocument25 pagesCommunity Health Nursing PDFCharles J B. Visaya80% (5)
- 5Document89 pages5inhaPas encore d'évaluation
- DIENCEPHALONDocument26 pagesDIENCEPHALONinhaPas encore d'évaluation
- Praktikum Jaringan SarafDocument34 pagesPraktikum Jaringan SarafinhaPas encore d'évaluation
- Homeostasis: How Negative and Positive Feedback Maintain Internal BalanceDocument25 pagesHomeostasis: How Negative and Positive Feedback Maintain Internal BalanceinhaPas encore d'évaluation
- Humoral Immune ResponsesDocument44 pagesHumoral Immune ResponsesinhaPas encore d'évaluation
- 04 - Transplantation Immunology s1 (Prof. Dr. Syarifuddin)Document18 pages04 - Transplantation Immunology s1 (Prof. Dr. Syarifuddin)Ririn AfriantoPas encore d'évaluation
- Homeostasis: How Negative and Positive Feedback Maintain Internal BalanceDocument25 pagesHomeostasis: How Negative and Positive Feedback Maintain Internal BalanceinhaPas encore d'évaluation
- Cell Physiology: Citra RosyidahDocument32 pagesCell Physiology: Citra RosyidahinhaPas encore d'évaluation
- Oxygen ToxicityDocument86 pagesOxygen Toxicityinha100% (1)
- Imunologi Tumor: Syarifuddin WahidDocument40 pagesImunologi Tumor: Syarifuddin WahidinhaPas encore d'évaluation
- Basic of DiagnosticDocument30 pagesBasic of DiagnosticTbm Fk UmiPas encore d'évaluation
- Effector Mecanism of Cell MediatedDocument32 pagesEffector Mecanism of Cell MediatedinhaPas encore d'évaluation
- Basic of DiagnosticengDocument30 pagesBasic of DiagnosticenginhaPas encore d'évaluation
- Kuliah Mata KorneaDocument37 pagesKuliah Mata KorneainhaPas encore d'évaluation
- Hypertensive Disorders in Pregnancy: Maisuri T. ChalidDocument44 pagesHypertensive Disorders in Pregnancy: Maisuri T. ChalidinhaPas encore d'évaluation
- Imunologi Tumor: Syarifuddin WahidDocument40 pagesImunologi Tumor: Syarifuddin WahidinhaPas encore d'évaluation
- Antigen Recognition in the Adaptive Immune System: A Review of Antibody and T Cell Receptor Mediated RecognitionDocument21 pagesAntigen Recognition in the Adaptive Immune System: A Review of Antibody and T Cell Receptor Mediated RecognitioninhaPas encore d'évaluation
- Dr. Agus... Nutrition-ImunologiDocument111 pagesDr. Agus... Nutrition-ImunologiinhaPas encore d'évaluation
- digestive+UG Biomedik IDocument64 pagesdigestive+UG Biomedik IinhaPas encore d'évaluation
- Basic of DiagnosticDocument30 pagesBasic of DiagnosticTbm Fk UmiPas encore d'évaluation
- StrabismusDocument56 pagesStrabismusinhaPas encore d'évaluation
- Prof, DR, DR Rukiah Sawal SPM (K)Document37 pagesProf, DR, DR Rukiah Sawal SPM (K)inhaPas encore d'évaluation
- Dr. Agus... Nutrition-ImunologiDocument111 pagesDr. Agus... Nutrition-ImunologiinhaPas encore d'évaluation
- Painful Shoulder Injury Case ReportDocument17 pagesPainful Shoulder Injury Case ReportinhaPas encore d'évaluation
- Wina Beach: Hotel & RestaurantDocument2 pagesWina Beach: Hotel & RestaurantinhaPas encore d'évaluation
- By: Andi Trisnawaty LeaderDocument28 pagesBy: Andi Trisnawaty LeaderinhaPas encore d'évaluation
- Reimbursement Form: To Be Completed by The Treating PhysicianDocument2 pagesReimbursement Form: To Be Completed by The Treating PhysicianrthomsanPas encore d'évaluation
- Joni DialogDocument3 pagesJoni DialogJoni TriliwijayaPas encore d'évaluation
- BK3 Greatest FearDocument4 pagesBK3 Greatest FearMaxine TaeyeonPas encore d'évaluation
- Jessedith Ann R. Gamboa, RN: Khalidiyah Street, Abu Dhabi, U.A.E Cell No. 0567802473Document4 pagesJessedith Ann R. Gamboa, RN: Khalidiyah Street, Abu Dhabi, U.A.E Cell No. 0567802473Yasi HanifPas encore d'évaluation
- Part 1 Executive Summary PDFDocument21 pagesPart 1 Executive Summary PDFNurul RafahPas encore d'évaluation
- Versana Ultrasound - GE HealthcareDocument16 pagesVersana Ultrasound - GE HealthcareJuan Pablo RamirezPas encore d'évaluation
- Name:Putri Al Zahra Prodi:S1 Keperawatan Semester: 2: Tugas Individu B. InggrisDocument6 pagesName:Putri Al Zahra Prodi:S1 Keperawatan Semester: 2: Tugas Individu B. InggrisPutri Al ZahraPas encore d'évaluation
- Scope of Midwifery Practice Concept Analysis PDFDocument6 pagesScope of Midwifery Practice Concept Analysis PDFKunal MahajanPas encore d'évaluation
- TOG Evolution in Screening For Down SyndromeDocument7 pagesTOG Evolution in Screening For Down SyndromeMarPas encore d'évaluation
- Jurnal Patologi AnatomiDocument5 pagesJurnal Patologi Anatomiafiqzakieilhami11Pas encore d'évaluation
- Sde105 PDFDocument37 pagesSde105 PDFMahaManthraPas encore d'évaluation
- St. Victoria Hospital Nursing Service Ward DeptDocument50 pagesSt. Victoria Hospital Nursing Service Ward DeptPat MagpaliPas encore d'évaluation
- Unit 3 Hospital Staffs and Departments: Objectives: After The Lesson, Students Will Be Able ToDocument22 pagesUnit 3 Hospital Staffs and Departments: Objectives: After The Lesson, Students Will Be Able ToLinh TrầnPas encore d'évaluation
- MIDWIFERY AND OBSTETRICAL NURSING COURSE PLANDocument12 pagesMIDWIFERY AND OBSTETRICAL NURSING COURSE PLANAashmeen KaurPas encore d'évaluation
- Bayi Baru LahirDocument43 pagesBayi Baru LahirBRI KUPas encore d'évaluation
- Endoscopic Tumour Surgery - Current Limits and Future PossibilitiesDocument4 pagesEndoscopic Tumour Surgery - Current Limits and Future PossibilitiesIliasa IliasPas encore d'évaluation
- TOG 2007 983-87 Review Cardiac Disease in Pregnancy Part 2 AcquiredDocument5 pagesTOG 2007 983-87 Review Cardiac Disease in Pregnancy Part 2 Acquiredsaeed hasan saeedPas encore d'évaluation
- Basics in Laser Therapy and Laser Acupuncture: 32 International Congress On Veterinary AcupunctureDocument10 pagesBasics in Laser Therapy and Laser Acupuncture: 32 International Congress On Veterinary Acupuncturebob marleyPas encore d'évaluation
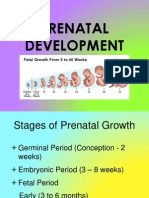
- Prenatal DevelopmentDocument23 pagesPrenatal DevelopmentCelestina TanPas encore d'évaluation
- Teacher Training on Menstrual HealthDocument12 pagesTeacher Training on Menstrual HealthJoseph ChakmaPas encore d'évaluation
- EMI. Khademi, ClarkDocument11 pagesEMI. Khademi, ClarkMaGe IsTePas encore d'évaluation
- Right Ventricular Function in Inferior Wall Myocardial Infarction: Case StudyDocument3 pagesRight Ventricular Function in Inferior Wall Myocardial Infarction: Case StudyIOSRjournalPas encore d'évaluation
- Hospital Pekan PresentationDocument25 pagesHospital Pekan PresentationImtiazPas encore d'évaluation
- Regional Anesthesia: Brachial Plexus BlockDocument77 pagesRegional Anesthesia: Brachial Plexus BlockTerefe AlemayehuPas encore d'évaluation
- You Exec - KPIs - 169 - BlueDocument14 pagesYou Exec - KPIs - 169 - BlueEssa SmjPas encore d'évaluation