Académique Documents
Professionnel Documents
Culture Documents
Bronchiectasis
Transféré par
Mujeeb Afzal0 évaluation0% ont trouvé ce document utile (0 vote)
177 vues36 pagesBronchiectasis presentation of pathogenesis and clinical features and management
Copyright
© © All Rights Reserved
Formats disponibles
PPTX, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentBronchiectasis presentation of pathogenesis and clinical features and management
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PPTX, PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
177 vues36 pagesBronchiectasis
Transféré par
Mujeeb AfzalBronchiectasis presentation of pathogenesis and clinical features and management
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PPTX, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 36
BRONCHIECTASIS
Broncos- Airways; Ectasia -Dilation
Defn: “It refers to an abnormal irreversible airway
dilation that involves the lung in either a focal or a
diffuse manner”.
Etiology: it can arise from infectious or noninfectious
causes
Based on pattern of lung involvement
a) Focal Brochiectasis
b) Diffuse Brochiectasis
PATTERN OF LUNG ETIOLOGY
INVOVEMENT
Focal Mechanical Bronchial Obstruction
1. Foreign Body
2. Endobrochial Growth (Tumor Mass, Endobrochial TB)
3. Extrinsic compression Of bronchus By Lymph node or
Tumor
Diffuse 1. Post Infective Bronchial Damage (Bacterial and Viral
Pneumonias - Pertussis, Measles, Aspiration
Pneumonia
2. Immune Deficiency (Hypogammaglobulinemia,HIV,
bronchiolitis Obliterans After Lung Transplantation)
3. Genetic causes (cystic fibrosis, Kartagener's syndrome
, α1- AT deficiency)
4. Immunological Overresponse (ABPA, Post Lung
Transplant
PATTERN OF LUNG ETIOLOGY
INVOVEMENT
Diffuse 5. Autoimmune or rheumatologic causes (Rheumatoid
Arthritis, Sjögren's syndrome, inflammatory bowel
disease)
6. Tractional Bronchiectasis ( Post Radiation Fibrosis,
Idiopathic Pulmonary Fibrosis)
Pathogenesis
Primary Necrotising pneumonia due to S. Aureaus, K.
Pneumoniae and P. Aerogenosa – destruction of bronchial
wall - Bronchiectasis
Necrotizing anerobic Pneumonias secondary to aspiration
or bronchial obstruction – Parenchymal destruction and
Bronchiectasis
Vicious Cycle Hypothesis:
Environmental insult often on a backround of Genetic
Susceptibility (Ex: Impaired Mucociliary clearence)
Resulting in persistance of Microbes in the sinobronchial
tree and Microbial colonisation chronic inflamation in
bronnchi Bronchiectasis
Pathogic process in right midle
lobe Mycobacterium infection
Infection causes enlargement of peribronchial Lymph
nodes resulting obstruction.
The obstruction results in brochiectasis that persists
when the nodes return to normal size.
Clinical features
Cough with Mucupurulent Sputum Production
(Purulent, Tenacious, frequently worse in the morning
– having accumulated during recumbency in sleep)
Hemoptysis (may vary from blood streaks to Large clot
Dyspnea
Features of Acute exacerbation – Increasing cough,
dyspnea, volume of sputum production, fever
hemoptysis, chest pain
Halitosis
Clubbing and hypertrophic pulmonary
osteoarthropathy
On auscultation – early & mid inspiratory crepitation
as well as diffuse ronchi and prolonged expiration ,
Bronchial breath sound may be heared in severe cases
or in complicating pneumonia
Treatment
Controlling infection
Reducing inflammation
Improving bronchial hygiene
Control of infection
1. Since infection plays major role in the causation and
progression of bronchiectasis – reducing microbial load
and associated inflammatory mediators remains
cornerstone of therapy.
2. Antibiotics are directed at commonly isolated pathogens
– H. influenzae, S. pneumonia & P. Aerogenosa
3. Oral /IV Fluroquinolones 10- 14 days
4. Oral /IV penicillin or cephalosporin
5. Administration of antipseudomonal antibiotics
6. Administration of antibiotic aerosols (Tobramycin 300
mg nebulized 2 times daily against pseudomonas)
Other aerosolized antibiotics – aztreonam, colistin,
gentamycin
5. Bronchial hygiene
Chest percussion & postural drainage – facilitate
mucus clearance
6. Mucus clearance
– maintenance of hydration (oral/ IV) – prevent
inspissated sputum retention,
7. Humidification of Inhaled Air or Oxygen as an
adjunct to chest physical therapy
8. Use of nebulized normal or Hypertonic saline and
acetylcysteine
9. Bronchodilator ;
Beta agonist , Anticholinergics, or theophyllines
10. Anti- inflammatory: ICS (Fluticasone)
Surgery: in selected cases surgical resection of most
severely affected segment, Bleeding segment, or areas
of harboring resistant tuberculosis or atypical
mycobacteria may confer significant benefit,
Lung transplantation – In advanced cases
Vaccination : vaccination against S.pneumonia and H.
Influenza
Vous aimerez peut-être aussi
- Lung Abscess Bronchoectasis PleurisynDocument19 pagesLung Abscess Bronchoectasis Pleurisynmarco luenaPas encore d'évaluation
- Lung AbscessDocument40 pagesLung AbscessAmmad JavedPas encore d'évaluation
- Chronic Obstructive Pulmonary Disease: Olivia Faye J Listanco IM Resident January 21, 2016Document52 pagesChronic Obstructive Pulmonary Disease: Olivia Faye J Listanco IM Resident January 21, 2016FayeListancoPas encore d'évaluation
- Acute Respiratory Distress Syndrome (Ards)Document12 pagesAcute Respiratory Distress Syndrome (Ards)Vin Grace Tiqui - GuzmanPas encore d'évaluation
- Respi SystemDocument6 pagesRespi SystemKalichandren ArumugamPas encore d'évaluation
- Bronchiectasis OkDocument60 pagesBronchiectasis OkImmanuelPas encore d'évaluation
- Pneumonia: Key FactsDocument28 pagesPneumonia: Key FactsAri Widiastuti NiPutuPas encore d'évaluation
- Pediatric Cardio-Respiratory AssessmentDocument9 pagesPediatric Cardio-Respiratory AssessmentRicky SpideyPas encore d'évaluation
- Lung AbscessDocument25 pagesLung AbscessIskandar HasanPas encore d'évaluation
- Mechanical Ventilation - ModesDocument40 pagesMechanical Ventilation - ModesabdallahPas encore d'évaluation
- Lung AbscessDocument27 pagesLung AbscessMalueth Angui100% (1)
- Diarrhea: Persistent If 2-4 Weeks, and Chronic If 4 Weeks in DurationDocument12 pagesDiarrhea: Persistent If 2-4 Weeks, and Chronic If 4 Weeks in DurationAnonymous IWRTYznDZnPas encore d'évaluation
- Airway Clearance Physiology Pharmacology Techniques and Practice PDFDocument5 pagesAirway Clearance Physiology Pharmacology Techniques and Practice PDFPaoly PalmaPas encore d'évaluation
- Respiratory Failure (Aan) PDFDocument19 pagesRespiratory Failure (Aan) PDFYudionoPas encore d'évaluation
- PneumoniaDocument71 pagesPneumoniafrancis00090100% (1)
- Case Study - PneumoniaDocument15 pagesCase Study - PneumoniaArgenic BernzPas encore d'évaluation
- Pneumonia: Submitted To:Ms Lisette Cruz Submitted By: Ms. Mely Rose AbanadorDocument26 pagesPneumonia: Submitted To:Ms Lisette Cruz Submitted By: Ms. Mely Rose AbanadorJoyce Catherine Buquing UysecoPas encore d'évaluation
- Review ArdsDocument25 pagesReview ArdsAdel HamadaPas encore d'évaluation
- COPD HarrisonsDocument45 pagesCOPD HarrisonsNogra CarlPas encore d'évaluation
- Rsexm 170207141549Document72 pagesRsexm 170207141549gpete321Pas encore d'évaluation
- Lung Abscess Handout PDFDocument3 pagesLung Abscess Handout PDFTansanee MalivalayaPas encore d'évaluation
- Anaesthesia For Patients With COPD: University College of Medical Sciences & GTB Hospital, DelhiDocument76 pagesAnaesthesia For Patients With COPD: University College of Medical Sciences & GTB Hospital, DelhiRINI100% (1)
- 42 Respiratory Insufficiency-Pathophysiology, Diagnosis, Oxygen TherapyDocument73 pages42 Respiratory Insufficiency-Pathophysiology, Diagnosis, Oxygen TherapyLaila AcehPas encore d'évaluation
- Cardiopulmonary ResuscitationDocument18 pagesCardiopulmonary ResuscitationNdor BariboloPas encore d'évaluation
- Cerebrovascular Accident/Stroke: Rodney R. Reyes, RNDocument51 pagesCerebrovascular Accident/Stroke: Rodney R. Reyes, RNRodney ReyesPas encore d'évaluation
- Medical Surgical Nursing 4 BulletsDocument5 pagesMedical Surgical Nursing 4 BulletsQueen ElizabethPas encore d'évaluation
- Pulmonary SystemDocument75 pagesPulmonary Systemangeles_robert_71Pas encore d'évaluation
- Pulmonary PathoPhysiologyDocument45 pagesPulmonary PathoPhysiologySuliman Garalleh100% (1)
- Lung Protective Mechanical Ventilation StrategiesDocument4 pagesLung Protective Mechanical Ventilation StrategiesAnne Julia AgustinPas encore d'évaluation
- Oxygen Therapy and Devices LectureDocument16 pagesOxygen Therapy and Devices LectureRegina Garrard100% (1)
- Lung SoundsDocument24 pagesLung SoundsAswinPas encore d'évaluation
- Endotracheal Tube Intubation: Vikas Sahu M.SC - Nursing (Prev.) BIMR College of Nursing GwaliorDocument39 pagesEndotracheal Tube Intubation: Vikas Sahu M.SC - Nursing (Prev.) BIMR College of Nursing Gwaliorvikas232372100% (1)
- PneumotoraxDocument39 pagesPneumotoraxnicusoorPas encore d'évaluation
- Assessment On RSDocument13 pagesAssessment On RSavinash dhameriyaPas encore d'évaluation
- Chest Injuries: DR Rodwell Gundo Medical/Surgical Nursing DepartmentDocument47 pagesChest Injuries: DR Rodwell Gundo Medical/Surgical Nursing Departmentpaul kaundaPas encore d'évaluation
- Empyema 171013100219Document23 pagesEmpyema 171013100219Mahmoud Abdel MoneimPas encore d'évaluation
- Approach To The Patient With DyspneaDocument22 pagesApproach To The Patient With DyspneaLuis Gerardo Alcalá GonzálezPas encore d'évaluation
- Dyspnea: Ahammed Naseem Roll No: 3 Second Year BSC Nursing Al-Mas College of NursingDocument19 pagesDyspnea: Ahammed Naseem Roll No: 3 Second Year BSC Nursing Al-Mas College of NursingNaseem Bin YoosafPas encore d'évaluation
- Cardiopulmonary Cerebral ResuscitationDocument17 pagesCardiopulmonary Cerebral ResuscitationrizalPas encore d'évaluation
- Bronchitis 170709131740Document28 pagesBronchitis 170709131740Viji MPas encore d'évaluation
- Congenital Heart DiseaseDocument45 pagesCongenital Heart DiseaseBrandedlovers OnlineshopPas encore d'évaluation
- Woman With PneumoniaDocument9 pagesWoman With PneumoniaNohaira SADANGPas encore d'évaluation
- Anatomo-Physiological Peculiarities of The Respiratory System. Percussion of The Lungs.Document40 pagesAnatomo-Physiological Peculiarities of The Respiratory System. Percussion of The Lungs.Hetvi PatelPas encore d'évaluation
- COPDDocument55 pagesCOPDRetno Lies SetiyowatiPas encore d'évaluation
- Lung AbsesDocument48 pagesLung AbsesAvhindAvhindPas encore d'évaluation
- EXERCISE - (Respiratory System)Document3 pagesEXERCISE - (Respiratory System)Schizophrenic RakibPas encore d'évaluation
- Respiratory Problems and ManagementDocument24 pagesRespiratory Problems and Managementaymona2000Pas encore d'évaluation
- Pneumonia: DefinitionDocument5 pagesPneumonia: DefinitionhemaanandhyPas encore d'évaluation
- Lung AuscultationDocument62 pagesLung AuscultationOlea CroitorPas encore d'évaluation
- Drugs in ObstetricsDocument95 pagesDrugs in ObstetricsPriya jPas encore d'évaluation
- Chest InjuriesDocument19 pagesChest InjuriesAbdi Kumala100% (1)
- Physiotherapy Management in Icu Patients: Dr.S.Ramachandran MPTDocument37 pagesPhysiotherapy Management in Icu Patients: Dr.S.Ramachandran MPTvaishnaviPas encore d'évaluation
- Acute Respiratory FailureDocument25 pagesAcute Respiratory FailureDyah Putri0% (1)
- Respiratory DiseasesDocument11 pagesRespiratory DiseasesMichael Angelo SeñaPas encore d'évaluation
- Lung Abscess: Presented byDocument36 pagesLung Abscess: Presented byPalanki Gopal100% (1)
- DR Muhammed AslamDocument56 pagesDR Muhammed AslamSef NengkoPas encore d'évaluation
- Handout AtelectasisDocument14 pagesHandout AtelectasisSasha IfahmyPas encore d'évaluation
- Suppurative Lung Diseases: DR Faisal Moidunny Mammu Department of PaediatricsDocument39 pagesSuppurative Lung Diseases: DR Faisal Moidunny Mammu Department of PaediatricsFaisal MoidunnyPas encore d'évaluation
- BronchiectasisDocument71 pagesBronchiectasisvijay1234568883Pas encore d'évaluation
- PneumoniaDocument79 pagesPneumoniaEjiro OnoroPas encore d'évaluation
- Foreign Body AspirationDocument3 pagesForeign Body AspirationAsiya ZaidiPas encore d'évaluation
- Worksheet Respiration CrosswordDocument2 pagesWorksheet Respiration CrosswordAcel PeñalozaPas encore d'évaluation
- Bronchial+asthma+questionnaire ApplicantDocument2 pagesBronchial+asthma+questionnaire ApplicantClaudine Limasa TabudlongPas encore d'évaluation
- Recentadvancesinthe Managementofacute Exacerbationsofchronic ObstructivepulmonarydiseaseDocument16 pagesRecentadvancesinthe Managementofacute Exacerbationsofchronic Obstructivepulmonarydiseaseadek07Pas encore d'évaluation
- Respiratory System Concept MapDocument1 pageRespiratory System Concept MapsamPas encore d'évaluation
- Waveform Pocket Guide BENNETTDocument31 pagesWaveform Pocket Guide BENNETTmeconioPas encore d'évaluation
- Faal Paru Dinamis: Jurnal RespirasiDocument8 pagesFaal Paru Dinamis: Jurnal RespirasiHafis HerdimanPas encore d'évaluation
- Nursing ManagementDocument16 pagesNursing ManagementNica Marie LumbaPas encore d'évaluation
- Lab 6 ReportDocument19 pagesLab 6 Reportapi-311215267100% (2)
- Ventilator Weaning and Spontaneous Breathing Trials An Educational Review 2016Document7 pagesVentilator Weaning and Spontaneous Breathing Trials An Educational Review 2016Tarran PhagooPas encore d'évaluation
- Pengaruh Variasi Tekanan Negatif Suction Endotracheal Tube (Ett) Terhadap Nilai Saturasi Oksigen (Spo)Document4 pagesPengaruh Variasi Tekanan Negatif Suction Endotracheal Tube (Ett) Terhadap Nilai Saturasi Oksigen (Spo)Amin KutbiPas encore d'évaluation
- Trauma ThoraksDocument35 pagesTrauma ThoraksmayaPas encore d'évaluation
- ICU One Pager NIPPVDocument1 pageICU One Pager NIPPVNicholas HelmstetterPas encore d'évaluation
- Test Bank Clinical Manifestations and Assessment of Respiratory Disease Mid PartDocument24 pagesTest Bank Clinical Manifestations and Assessment of Respiratory Disease Mid Partweekup035Pas encore d'évaluation
- Impaired Gas ExchangeDocument2 pagesImpaired Gas ExchangeHanya Bint PotawanPas encore d'évaluation
- PPOK Jurnal NewDocument8 pagesPPOK Jurnal NewjihanPas encore d'évaluation
- NCM 103 Final ExamDocument10 pagesNCM 103 Final ExamRichmond LacadenPas encore d'évaluation
- Contoh Leaflet BronkitisDocument2 pagesContoh Leaflet BronkitisVira Noor AzharPas encore d'évaluation
- Center For Physiotherapy and Rehabilitation Science Jamia Millia IslamiaDocument16 pagesCenter For Physiotherapy and Rehabilitation Science Jamia Millia IslamiaummiPas encore d'évaluation
- MCQ Asthma CopdDocument26 pagesMCQ Asthma Copdanisa930804Pas encore d'évaluation
- Babylog-Vn500 With HFODocument10 pagesBabylog-Vn500 With HFOABHINANDAN SHARMAPas encore d'évaluation
- Ncp-Ineffective Airway ClearanceDocument3 pagesNcp-Ineffective Airway Clearancelouanne0550% (2)
- Aquapor h300 Pi 9107502 en GBDocument8 pagesAquapor h300 Pi 9107502 en GBHaitham AlhomaidePas encore d'évaluation
- COPD LeafletDocument2 pagesCOPD LeafletAN KnEePas encore d'évaluation
- Jurnal Pursed Lips BreatingDocument6 pagesJurnal Pursed Lips BreatingLya RahmaPas encore d'évaluation
- SpirometryDocument11 pagesSpirometryTrandafirulNegruPas encore d'évaluation
- RT Skills ChecklistDocument3 pagesRT Skills ChecklistMond SantosPas encore d'évaluation
- Nebu&CPTDocument32 pagesNebu&CPTAbigail Bantayan100% (1)
- Critical Incidentsduring Perioperative Period Sept 2011Document106 pagesCritical Incidentsduring Perioperative Period Sept 2011wellawalalasithPas encore d'évaluation
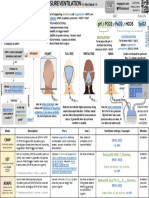
- Initial Ventilator SettingsDocument22 pagesInitial Ventilator Settingsandi wija indrawanPas encore d'évaluation