Académique Documents
Professionnel Documents
Culture Documents
Tuberculosis
Transféré par
Alna Shelah Ibañez0 évaluation0% ont trouvé ce document utile (0 vote)
14 vues58 pagesCopyright
© © All Rights Reserved
Formats disponibles
PPTX, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PPTX, PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
14 vues58 pagesTuberculosis
Transféré par
Alna Shelah IbañezDroits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PPTX, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 58
Classification Definition
Presumptive TB A patient who presents with
symptoms or signs (radiologic
findings) suggestive of TB
(replaces the term TB suspect or
TB symptomatic).
Bacteriologically confirmed A patient from whom a
case of TB biological specimen is positive
by smear microscopy, culture or
WHO-approved rapid diagnostic
test (such as Xpert® MTB/RIF).
Classification Definition
New Case A patient who never had
treatmentfor TB or who has
taken anti – TB medications for
less than < 1 month
Retreatment case Patient who has received
1month or more of anti-
TBdrugs in the past
(excluding prophylaxis or
treatment for latent TB
infection), further classifed by
the outcome of most recent
course of treatment
Relapse patient has previously been treated
for TB, declared cured or treatment
completed at the end of most
recent course of treatment, and is
now diagnosed with a recurrent
episode of TB (either a true relapse
or a new episode of TB caused by
reinfection
Treatment after failure patient has previously been treated
for TB and declared treatment
failed at the end of most recent
course of treatment
Treatment after lost to follow- Patient has previously been
up (TALF) treated for TB, declared lost to
follow-up at the end of most
recent course of treatment
(previously known as Return
After Default)
Previous Treatment Outcome Patient has previously been
Unknown (PTOU) treated for TB but outcome after
their most recent course of
treatment is unknown or
undocumented
Other Patients who do not into any of
the categories listed above
ANATOMIC BACTERIOLOGIC DEFINITION OF TERMS
SITE STATUS
Pulmonary Bacteriologically Smear A patient with at
(PTB) Confirmed positive least one (1)
sputum
specimen
positive for AFB,
with or without
radiologic
abnormalities
consistent with
active TB
ANATOMIC BACTERIOLOGIC DEFINITION OF TERMS
SITE STATUS
Pulmonary Bacteriologically Culture A patient with
(PTB) Confirmed positive positive sputum
culture for MTB
complex, with or
without
radiographic
abnormalities
consistent with
active TB
ANATOMIC BACTERIOLOGIC DEFINITION OF TERMS
SITE STATUS
Pulmonary Bacteriologically Rapid A patient with
(PTB) Confirmed diagnostic sputum positive
test for MTB complex
positive using rapid
diagnostic
modalities such as
Xpert® MTB/
Rif, with or without
radiographic
abnormalities
consistent with
active TB
ANATOMIC BACTERIOLOGIC DEFINITION OF TERMS
SITE STATUS
Pulmonary Clinically Diagnosed A patient with 2 sputum
(PTB) specimens negative for AFB or
MTB, smear not done due to
specified conditions but with
radiographic abnormalities
consistent with active TB, and
there has been no response to
empiric antibiotics and/or
symptomatic medications, and
who has been decided to have
TB disease requiring full course
of anti-TB chemotherapy
DIAGNOSTICS EXPECTED FINDINGS
SPUTUM MICROSCOPY At least 2 sputum specimens
FOR AFB should be sent
Sputum Collection:
• spot – spot one hour apart
•Or early morning
specimens
Sputum TB Culture Primarily recommended for
patients at risk for drug
resistance
DIAGNOSTICS EXPECTED FINDINGS
Sputum TB Culture It is recommended in the
following smear positive
patients:
•All of cases of retreatment
•All cases of Treatment Failure
•All other cases of smear postive
patients suspected to have one
or multi drug resistant TB
•All household contacts of
patients with MDR-TB
•In patients with HIV
DIAGNOSTICS EXPECTED FINDINGS
Chest Radiograph Recommended for patients
suspected to have PTB
whose sputum smears are
negative
Rapid Diagnostic Test Gene rapid testing for
( Xpert MTB/Rif Assay) presence of M. Tuberculosis
and Rifampicin resistance
CATEGORY TB PATIENTS ALTERNATIVE TB
TREATMENT
INITIAL CONT.
PHASE PHASE
I New case ( 2 HRZE 4 HR / 4
Bacteriologically/ HRE
clinically
diagnosed)
IA New Extra 2 HRZE 10 hr
Pulmonary TB
CATEGORY TB PATIENTS ALTERNATIVE TB
TREATMENT
INITIAL CONT.
PHASE PHASE
II Previously Treated 2 HRZES AND 5 HRE
drug TB 1 HRZE
•Relapse
•Treatment Failure
•Treatment after loss
to follow up
•Previous Treatment
Outcome Unknown
•Other
CATEGORY TB PATIENTS ALTERNATIVE TB
TREATMENT
INITIAL CONT.
PHASE PHASE
IIA ExtraPulmonary 2 HRZE AND 9 HRE
previously treated, 1 HRZE
drug susceptableTB
Minor adverse reactions
• Gastrointestinal intolerance
• Mild or localized skin reactions
• Orange/red-colored urine
• Pain at the injection site
• Burning sensation in the feet due to peripheral
neuropathy
• Arthralgia due to hyperuricemia
• Flu-like symptoms (fever, muscle pains, in
ammation of the respiratory tract)
Major adverse reactions
• Severe skin rash due to hypersensitivity
• Jaundice due to hepatitis
• Impairment of visual acuity and color vision
due to optic neuritis • Hearing impairment,
ringing of the ears, dizziness due to damage of
the eighth cranial nerve
• Oliguria or albuminuria due to renal disorder •
Psychosis and convulsion
• Thrombocytopenia, anemia, shock
Clinically diagnosed and bacteriologically-con
rmed cases treated with rst-line drugs: DO at
least one sputum smear microscopy at the
end of the intensive phase of treatment (end
of 2 months for new cases and end of 3
months for retreatment cases)
New patients - if the specimen obtained at
the end of 2 months is smear-positive, repeat
DSSM at the end of the third month.
New and Retreatment patients - if the
specimen obtained at the end of third month
is still smear-positive, do Xpert®MTB/Rif,
sputum culture and DST.
Clinically diagnosed cases whose sputum
smears are negative at end of intensive phase
need no further sputum monitoring.
Sputum specimen at end of 5 and 6 months
should be obtained for all new smear positive
TB patients. If results are positive, do culture
and DST
Patients found to be harboring a drug-
resistant strain at any point during treatment
should be referred to a PMDT center.
All PTB and EPTB patients should also be
monitored clinically. Body weight is a useful
progress indicator that should be monitored
and medication doses adjusted according to
weight
Rapid diagnostic tests (such as Interferon
Gamma Release Assay, Xpert® MTB/Rif,
Antiphopholipid Antibody tests) are NOT
recommended for monitoring treatment
response pending further studies.
CXR is NOT a substitute for microbiological
monitoring. It may be used in monitoring
complications, identifying co-existing
conditions.
Patients who are bacteriologically-con rmed
and do not have risk factors for drug-
resistance are considered non-infectious
when they have received at least 14 daily
doses of treatment with sputum conversion
and clinical improvement.
Patients who are clinically diagnosed and do
not have risk factors for drug-resistance are
considered non-infectious when they have
received at least 5 daily doses of treatment
with clinical improvement.
• Mono-resistant TB - resistance to one frst-
line anti-TB drug only
• Polydrug-resistant TB - resistance to more
than one frst-line anti-TB drug, other than
both Isoniazid and Rifampicin
• Multidrug-resistant TB (MDR-TB) -
resistance to at least both Isoniazid and
Rifampicin
Extensively drug-resistant TB (XDR-TB) -
multidrug-resistant TB plus resistance to any
fuoroquinolone and at least one of three
secondline injectable drugs (Capreomycin,
Kanamycin and Amikacin)
Rifampicin-resistant TB (RR-TB) - resistance
to Rifampicin detected using Xpert® MTB/Rif
test or conventional DST, with or without
resistance to other anti-TB drugs. It includes
any resistance to Rifampicin, whether mono-
resistance, multidrug resistance, polydrug
resistance or extensive drug resistance
Results when a person has been infected with
a drug-resistant TB strain. Transmission of
drug-resistant TB occurs in the same way as
transmission of drug-susceptible TB. High
prevalence of drug resistant TB in the
community increases the risk of drug-
resistant TB exposure in the community.
Results from inadequate, incomplete or poor
treatment quality that allows the selection of
mutant resistant strains.
If drug-susceptible TB is treated with a
regimen exclusively based on a single
effective TB medicine, there is a risk that
bacteria with drug-resistant mutations will be
selected and multiply further during the
course of treatment, eventually becoming
the dominant strain.
Presumptive drug-resistant tuberculosis (DR-
TB) refers to persons at high risk in developing
DR-TB. They include any of the following new
and re-treatment cases:
1. All retreatment cases – relapse, treatment
failure, treatmentafter lost to follow-up (TALF),
previous treatment outcome unknown (PTOU)
2. New cases who are:
a. Non-converter of Category I - new TB cases
who remain
sputum smear-positive at the end of third
month of treatment;
b. Contacts of confirmed DR-TB cases -
persons who shared enclosed space, such as
the household, a social gathering place,
workplace or facility, for extended periods
within the day with the confirmed index DR-
TB case during the three(3) months before
initiation of the current DR-TB treatment;
c. People living with HIV (PLHIV) with signs
and symptoms of TB - persons living with HIV
with radiologic findings suggestive of TB
and/or any of the four symptoms: cough,
fever, weight loss, night sweats
Assessment of likelihood of drug resistance
based on history of prior treatment and
exposure to a DR-TB case should be
undertaken for all patients.
Conventional (phenotypic) Drug
Susceptibility Testing (DST) on culture
isolates.
° The Lowenstein Jensen method remains the
gold standard for the diagnosis of DR-TB,
preferably in quality-assured DST centers
identified by the National TB Program.
Genotypic DST, endorsed by WHO, namely:
° Xpert® MTB/Rif
° Line Probe Assay (LPA)
Xpert® MTB/Rif should be used as the initial
diagnostic test in presumptive DR-TB.
All DR-TB patients should be managed under
programmatic setting.
Management of DR-TB involves the use of
second line drugs that are more expensive, less
effective and more toxic for at least 18 months.
Management outside the proper framework will
only lead to further drug resistance.
Immediate referral to the nearest PMDT
Treatment Center or Satellite Treatment Center
is mandatory.
Inhibits bacterial replication by blocking their
DNA replication pathway
Divided into 2 groups:
Older group: Ciprofloxacin, norfloxacin,
and ofloxacin
Newer group: Gemifloxacin, levofloxacin,
and moxifloxacin
MOA:
Inhibit bacterial replication by blocking their DNA
replication pathway.
Adults with rifampicin resistant or multi drug
resistant TB should always receive a second
line injectable agent as part of their regimen,
unless there is an important reason for not
doing so.
The choice of which of the three standard
agents to use, amikacin, capreomycin or
kanamycin.
MOA:
Irreversibly binds to 30S subunit of bacterial
ribosomes; blocks recognition step in protein
synthesis; causes growth inhibition. For gram-
negative bacterial coverage of infections resistant
to gentamicin and tobramycin
Adverse effects need to be carefully
monitored for while using second line
injectable agents. Hearing loss and
nephrotoxicity are among the most frequent
and most severe.
Ethionamide (or prothionamide) cycloserine
(or terizidone) linezolid and cclofazimine.
Group C agents are included to bring the total
of effective second line TB medicines in the
core regimen to at least four during the
intensive phase of the regimen.
MOA:
Binds to bacterial 23S rRNA of the 50S subunit to
prevent protein translation
Group D1 consists of pyrazinamide,
ethambutol and high dose isoniazid. These
agents are usually added to the core second
line medications unless the risks from
confirmed resistance, pill burden, intolerance
or drug drug interactions outweigh the
potential benefits.
Group D2 is made up
of bedaquiline and delamanid. These are
two new TB drugs. The previous
recommendations for their use haven’t
changed.
MOA:
specifically inhibits mycobacterial ATP (adenosine
5’-triphosphate) synthase, by binding to subunit c
of the enzyme that is essential for the generation
of energy in Mycobacterium tuberculosis
Group D3 consists of p-aminosalicylic acid
(PAS), imipenem-cilastatin, meropenem,
clavulanate and thioacetazone. These drugs
are only to be used when an MDR-TB
regimen with at least 5 effective drugs cannot
otherwise be composed.
MOA:
Inhibits cell-wall synthesis by binding to penicillin-
binding proteins; resistant to most beta-
lactamases
Vous aimerez peut-être aussi
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Pyloric Stenosis in AdultsDocument6 pagesPyloric Stenosis in AdultsAlna Shelah IbañezPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Vitamin C and Wound HealingDocument8 pagesVitamin C and Wound HealingAlna Shelah IbañezPas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Pancreatitis Severity ScoringDocument3 pagesPancreatitis Severity ScoringAlna Shelah IbañezPas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Anatomy Abdominal Wall ThorekDocument26 pagesAnatomy Abdominal Wall ThorekAlna Shelah IbañezPas encore d'évaluation
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Physiologic Monitoring of A Surgical PatientDocument41 pagesPhysiologic Monitoring of A Surgical PatientAlna Shelah IbañezPas encore d'évaluation
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Rabies: Prophylaxis If The Animal Can BeDocument1 pageRabies: Prophylaxis If The Animal Can BeAlna Shelah IbañezPas encore d'évaluation
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- ATA Thyroid PDFDocument133 pagesATA Thyroid PDFAlna Shelah IbañezPas encore d'évaluation
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
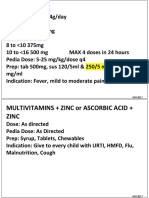
- Common RHU DrugsDocument56 pagesCommon RHU DrugsAlna Shelah IbañezPas encore d'évaluation
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- GS Must Knows1Document7 pagesGS Must Knows1Alna Shelah IbañezPas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- TuberculosisDocument4 pagesTuberculosisMjel Kezhia BarrietaPas encore d'évaluation
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Anti - Tubercular DrugsDocument88 pagesAnti - Tubercular DrugsEscitalopram 5mgPas encore d'évaluation
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Guideline TBDocument128 pagesGuideline TBChest X RayPas encore d'évaluation
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- My Co BacteriumDocument15 pagesMy Co BacteriumPatrickPas encore d'évaluation
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Manual: Federal Ministry of Health EthiopiaDocument196 pagesManual: Federal Ministry of Health Ethiopiaalfonso delgadoPas encore d'évaluation
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Multidrug-Resistant Tuberculosis: Agus Suharto BasukiDocument45 pagesMultidrug-Resistant Tuberculosis: Agus Suharto BasukidrhendraagusPas encore d'évaluation
- Definitions and Reporting Framework For Tuberculosis - 2013 RevisionDocument47 pagesDefinitions and Reporting Framework For Tuberculosis - 2013 RevisionDavien UtoyoPas encore d'évaluation
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Computational Biology and Chemistry: SciencedirectDocument9 pagesComputational Biology and Chemistry: SciencedirectFuckPas encore d'évaluation
- Biology Project On TBDocument20 pagesBiology Project On TBAdnan Fazeel73% (15)
- Pott DiseaseDocument8 pagesPott DiseaseMuhammad IrwantoPas encore d'évaluation
- Webinar Presentation of DR Jose "Pepe" Caminero On Scientific Highlights of 47th Union World Conf On Lung Health in Liverpool UKDocument29 pagesWebinar Presentation of DR Jose "Pepe" Caminero On Scientific Highlights of 47th Union World Conf On Lung Health in Liverpool UKbobbyramakantPas encore d'évaluation
- Tuberculosis: WHO Global Tuberculosis Report 2014Document2 pagesTuberculosis: WHO Global Tuberculosis Report 2014blueicelandPas encore d'évaluation
- Derivados de Benzofurano y Sus Actividades Antituberculosas y AntibacterianasDocument11 pagesDerivados de Benzofurano y Sus Actividades Antituberculosas y AntibacterianasMario Suarez GiraldoPas encore d'évaluation
- Smita Mishra, Manisha Khatri, Varsha Mehra - Trials and Tribulations in Tuberculosis Research: Can Plant Based Drug(s) Be The Solution?Document15 pagesSmita Mishra, Manisha Khatri, Varsha Mehra - Trials and Tribulations in Tuberculosis Research: Can Plant Based Drug(s) Be The Solution?Smita MishraPas encore d'évaluation
- World Bank HIV/AIDS Program Development Project (II) in Nigeria, An Exploration of TB and TB/HIV OptionsDocument29 pagesWorld Bank HIV/AIDS Program Development Project (II) in Nigeria, An Exploration of TB and TB/HIV OptionsChukwu JanefrancesPas encore d'évaluation
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Impact of Target-Based Drug Design in Anti-Bacterial Drug Discovery For The Treatment of TuberculosisDocument40 pagesImpact of Target-Based Drug Design in Anti-Bacterial Drug Discovery For The Treatment of TuberculosisBhabani DasPas encore d'évaluation
- Research Proposal by Dr. Muhammad Abuzar Khan ShiraniDocument12 pagesResearch Proposal by Dr. Muhammad Abuzar Khan ShiraniDr.Abuzar ShiraniPas encore d'évaluation
- Antimycobacterials and AntiviralsDocument65 pagesAntimycobacterials and AntiviralsAndile MoloiPas encore d'évaluation
- Global TB Report 2017Document262 pagesGlobal TB Report 2017doc_next_doorPas encore d'évaluation
- MDR - TB FACTS AND CONCERNS BY Dr.T.V.Rao MDDocument33 pagesMDR - TB FACTS AND CONCERNS BY Dr.T.V.Rao MDtummalapalli venkateswara raoPas encore d'évaluation
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- National Tuberculosis Control Program Manual of Procedures 5th EditionDocument192 pagesNational Tuberculosis Control Program Manual of Procedures 5th EditionBlue Pielago100% (9)
- Prevalence, Types and Treatment of Tuberculosis: A ReviewDocument25 pagesPrevalence, Types and Treatment of Tuberculosis: A ReviewUMT JournalsPas encore d'évaluation
- RNTCPDocument46 pagesRNTCPdarshitkotadiya2553Pas encore d'évaluation
- Thesis Title DeferenceDocument37 pagesThesis Title Deferencemarlar khinPas encore d'évaluation
- Tuberculous EndocarditisDocument6 pagesTuberculous EndocarditisgioandregabPas encore d'évaluation
- Dhananjay Bokade Practice School 1Document16 pagesDhananjay Bokade Practice School 1Gayatri BokadePas encore d'évaluation
- PMDT Guidelines 2017 IndiaDocument200 pagesPMDT Guidelines 2017 IndiaNarendra AnnaladasuPas encore d'évaluation
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- What Is Multidrug-Resistant Tuberculosis (MDR-TB) ?Document63 pagesWhat Is Multidrug-Resistant Tuberculosis (MDR-TB) ?Birhanu AbebePas encore d'évaluation
- Johnlyn May A. Bongot Bsnursing 2B Nursing Care Plan (Pulmonary Tuberculosis)Document17 pagesJohnlyn May A. Bongot Bsnursing 2B Nursing Care Plan (Pulmonary Tuberculosis)johnlyn bongotPas encore d'évaluation
- Tuberculosis - Knowledge at AMBOSSDocument4 pagesTuberculosis - Knowledge at AMBOSSKC Dela RosaPas encore d'évaluation