Académique Documents
Professionnel Documents
Culture Documents
KERATOPLASTY
Transféré par
Sri RamDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
KERATOPLASTY
Transféré par
Sri RamDroits d'auteur :
Formats disponibles
An eye bank is an organization which obtains,evaluates and distributes eyes from humanitarian minded citizens for use in corneal
transplantation, research and education To ensure patient safety,the donated eyes are evaluated under strict medical standards All donated eyes not suitable for corneal transplantation are used for valuable research and education
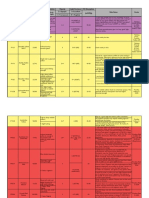
EBAA has developed extensive criteria for screening donor corneas to avoid transmissable infections and other conditions.Contraindicatons include Death of unknown cause Unknown CNS disease or certain infections (eg. Creutzfeldt-Jacob disease,SSPE,Progressive multifocal leukoencephalopathy,congenital rubella,rabies,Reye syndrome,active viral encephalitis,encephalitis of unknown origin)
Active septicemia Social ,clinical or laboratory evidence suggestive of HIV infecton,syphilis, or active viral hepatitis) Leukemias or active disseminated lymphomas Active bacterial or fungal endocarditis Active ocular or intraocular inflammation such as iritis,scleritis, conjunctivitis,choroiditis
Intrinsic malignanciessuch as malignant anterior segment tumors,adenocarcinoma in the eye of primary or metastatic origin,and retinoblastoma Congenital or acquired eye disorders that would preclude successful surgical outcome: any central donor corneal scar or pterygium involving the central 8mm clear zone(optical area of the donor button), keratoconus, keratoglobus, or Fuchs dystrophy
Prior refractive coneal surgery such as radial keratotomy(RK), PRK, LASIK, and lamellar inserts,although for use in endothelial keratoplasty such as DSAEK, refractive laser surgery may not disqualify a donor. Hepatitis B surface antigen- positive donors, hepatitis C seropositive donors.
Corneas from patients with prior intraocular surgery (cataract, IOL implants, glaucoma filtration) may be accepted if endothelial adequacy is documented by specular microscopy Other factors to be considered includes slit lamp appearance of donor tissue specular microscopic data( endothelial cell counts <2000 cells/mm2 are not used)
Death to preservation time(optimal range <12-18 hrs) Tissue storage time prior to keratoplasty Donor age Most eye banks establish a lower age limit of 24 months and an upper age limit of 70 years
The McCarey-Kaufman tissue transport medium developed in the early 1970s significantly reduced endothelial cell attrition, allowing corneal buttons to be safely transplanted after being stored for up to 4 days at 4C. Most commonly used preservative medium is Optisol-GS(Bausch & Lomb, Irvine,CA) which includes 2.5%chondroitin sulphate, 1% dextran, ascorbic acid, vitamin B 12, and the antibiotics gentamycin and streptomycin.
Corneal transplantation refers to surgical replacement of a full-thickness or lamellar portion of the host cornea with that of a donor eye. Allograft-if the donor is another person Autograft-use of donor tissue from the same or fellow eye
Complete eye examination,including a detailed social history to help determine the patients compliance postoperatively. Ocular surface problems-dry eyes,trichiasis,exposure,blepharitis,and rosacea must be recognized and treated Pre existing glaucoma or ocular inflammation should be controlled.
Active keratitis or uveitis is treated and the eye should be quiet for several months prior to surgery. FFA and OCT can be helpful in detecting retinal problems-CME and ARMD Poor prognostic factors-deep corneal vascularization,ocular surface disease, active anterior segment inflammation,peripheral corneal thinning,previous graft failures, poor compliance and increased IOP.
Indications- any stromal or endothelial corneal pathology Intraoperative complicationsdamage to the lens or iris from the trephine,scissors or other instruments irregular trephination poor graft centration on the host bed excessive bleeding-iris and the wound edge
Intra operative complicationschoroidal hemorrhage and effusion iris incarceration in the wound damage to the donor endothelium during transplantation and handling
More complex than cataract surgery Long term success of a PK depends on the quality of the postop care as much as on the performance of the operative technique Topical antibiotics,tapering topical corticosteroids.
Wound leak Flat chamber Glaucoma Endophthalmitis Persistent epithelial defect Recurrent primary disease Primary graft failure Graft rejection Corneal astigmatism
Early recognition is the key to survival of an affected corneal graft Occurs in four clinical forms Epithelial rejection Subepithelial rejection Stromal rejection Endothelial rejection Treatment-topical corticosteroidsdexamethasone 0.1% or prednisolone 1%
Full-thickness tissue eliminates interfacerelated visual problems
Difficult to determine anterior corneal curvature,leading to significant refractive error Post operative astigmatism Ocular surface disease or neurotrophic cornea leads to prolonged healing or persistent epithelial defect
2 types Superficial Anterior Lamellar Keratoplasty(SALK) Deep Anterior Lamellar Keratoplasty(DALK)
INDICATIONS- Superficial stromal dystrophies and degenerations Salzmann nodular degeneration Scars,trauma,dermoids infections Poor microkeratome dissection Corneal perforation
Postoperative complications- loss of donor lenticule Advantages- selective removal of pathologic tissue more rapid visual rehabilitation Reduced risk of graft rejection Disadvantages-irregular surface,interface vascularization
INDICATIONSKeratoconus Infections Corneal stromal dystrophies not involving endothelium Corneal ectasia secondary to LASIK
Intraoperative complicationsCorneal perforation requiring transition to PK Descemets membrane splitting Postoperative complicationsopacification and vascularization of interface, allograft rejection, inflammatory necrosis of the graft
ADVANTAGES- Tectonically stronger wound than in PK Early removal of sutures Less dependence on topical corticosteroids Minimal requirements for donor tissue DISADVANTAGES- Irregular interface
In this procedure, descemets membrane and endothelium are stripped in the host eye (descemetorhexis),producing a smooth posterior stromal bed in the host. INDICATIONS- Endothelial dystrophy Pseudophakic bullous keratopathy ICE syndrome Failed corneal grafts
Poor microkeratome dissection of donor tissue Inability to strip descemets tissue Loss of orientation of tissue Poor centration of trephination,leading to a thick edge and possible epithelial growth Intaocular hemorrhage Excessive manipulation of tissue , leading to cell loss
Pupillary block Dislocation of lenticule Primary graft failure Epithelial ingrowth
Rapid visual rehabilitation Independent of ocular surface wound healing Stable corneal curvature for triple procedures Tectonically strong Eliminates suture related problems
Significant stromal haze,subepithelial fibrosis, or epithelial irregularity may require second procedure Possible higher rate of endothelial cell loss
Vous aimerez peut-être aussi
- Posterior Polar Cataract Management: My Approach: 2022, #1D'EverandPosterior Polar Cataract Management: My Approach: 2022, #1Pas encore d'évaluation
- Jurnal KeratoplastyDocument58 pagesJurnal KeratoplastyFadli LatamaPas encore d'évaluation
- Penetrating KeratoplastyDocument35 pagesPenetrating KeratoplastyAnumeha JindalPas encore d'évaluation
- Keratoplasty: By: Esmaeil Hashemi MC: 410a Dept. of OphthalmologyDocument43 pagesKeratoplasty: By: Esmaeil Hashemi MC: 410a Dept. of OphthalmologyEsmaeil HashemiPas encore d'évaluation
- CATARACTDocument25 pagesCATARACTDea NabilaPas encore d'évaluation
- Pseudophakic BullousDocument6 pagesPseudophakic BullousanglingPas encore d'évaluation
- Pars Plana VitrectomyDocument6 pagesPars Plana VitrectomyAndreas OctavianoPas encore d'évaluation
- A Collaborative Retrospective Study On The Efficacy and Safety of Intravitreal Dexamethasone Implant (Ozurdex) in Patients With Diabetic Macular EdemaDocument17 pagesA Collaborative Retrospective Study On The Efficacy and Safety of Intravitreal Dexamethasone Implant (Ozurdex) in Patients With Diabetic Macular EdemaJosé Díaz OficialPas encore d'évaluation
- Episkleritis Dan SkleritisDocument41 pagesEpiskleritis Dan SkleritisSuryana AdityaPas encore d'évaluation
- Lacrimal System: Www. MD .LyDocument19 pagesLacrimal System: Www. MD .Lyعبدالسلام ميلاد درباشPas encore d'évaluation
- Bullous Keratopathy PRDocument12 pagesBullous Keratopathy PRshevinesaPas encore d'évaluation
- A Review of Anti-Vegf Agents For Proliferative Diabetic RetinopathyDocument7 pagesA Review of Anti-Vegf Agents For Proliferative Diabetic RetinopathyIJAR JOURNALPas encore d'évaluation
- Morphologic Alterations On Posterior Iris-Claw Intraocular Lenses After Traumatic DisenclavationDocument5 pagesMorphologic Alterations On Posterior Iris-Claw Intraocular Lenses After Traumatic DisenclavationYanjinlkham Kh100% (1)
- Atlas of Retinal OCTDocument211 pagesAtlas of Retinal OCTVianka García LópezPas encore d'évaluation
- Proforma For Thesis of Master of Suregry (Ophthalmology) Deen Dayal Upadhyaya University, Gorakhpur U.PDocument18 pagesProforma For Thesis of Master of Suregry (Ophthalmology) Deen Dayal Upadhyaya University, Gorakhpur U.PSumit Kumar GuptaPas encore d'évaluation
- Ocular EmergDocument61 pagesOcular EmergKBR RS UNHAS100% (1)
- 19 Rationale of Retinal Detachment ManagementDocument87 pages19 Rationale of Retinal Detachment ManagementvajasaPas encore d'évaluation
- Crao PosterDocument1 pageCrao PosterNataShini RajaRatnamPas encore d'évaluation
- 42fundus AngiographyDocument28 pages42fundus AngiographyHitesh SharmaPas encore d'évaluation
- DacryocystorhinostomyDocument3 pagesDacryocystorhinostomyNarla SusheelPas encore d'évaluation
- Nov Dec2010Document42 pagesNov Dec2010Mr.ZeddPas encore d'évaluation
- Periorbital and Orbital CellulitisDocument51 pagesPeriorbital and Orbital CellulitisJoanne BlancoPas encore d'évaluation
- Penetrating Keratoplasty StepsDocument57 pagesPenetrating Keratoplasty StepsVishwajeetPas encore d'évaluation
- Eye Docs Pharmacology & TherapeuticsDocument72 pagesEye Docs Pharmacology & TherapeuticsMuhammed Abdulmajeed100% (1)
- Correlation of Retinal Structural Alteration With Retinal Sensitivity Loss: A Prospective StudyDocument26 pagesCorrelation of Retinal Structural Alteration With Retinal Sensitivity Loss: A Prospective StudyAbhishek KothariPas encore d'évaluation
- Original Article Factors Related To Filtration-Bleb Morphology After Ex-PRESS SurgeryDocument9 pagesOriginal Article Factors Related To Filtration-Bleb Morphology After Ex-PRESS SurgeryJordi RipollPas encore d'évaluation
- Managing Complications in Glaucoma SurgeryDocument121 pagesManaging Complications in Glaucoma Surgeryshetya_8212Pas encore d'évaluation
- Anisman Acute Vision LossDocument68 pagesAnisman Acute Vision Lossarnol3090Pas encore d'évaluation
- Ptosis Definition of Eyelid Ptosis: Abnormally Low Position of The Upper Eyelid Margin Caused by PoorDocument6 pagesPtosis Definition of Eyelid Ptosis: Abnormally Low Position of The Upper Eyelid Margin Caused by PoortiamaharaniPas encore d'évaluation
- Cataract Surgery in Retina PatientsDocument21 pagesCataract Surgery in Retina PatientsAnonymous 4OnqyBErPas encore d'évaluation
- Chapter 23 Indications and Contradictions For Contact Lens Wear PDFDocument16 pagesChapter 23 Indications and Contradictions For Contact Lens Wear PDFfakenamePas encore d'évaluation
- Vitreous SubstitutesDocument17 pagesVitreous SubstitutesAnumeha JindalPas encore d'évaluation
- Retinal Drawing A Lost Art of MedicineDocument3 pagesRetinal Drawing A Lost Art of MedicinekavyaPas encore d'évaluation
- Phaco NightmaresDocument13 pagesPhaco NightmaresNiloy BasakPas encore d'évaluation
- Plasma Blade in OphthalmologyDocument6 pagesPlasma Blade in Ophthalmologyfunda007100% (1)
- Cataract SurgeryDocument2 pagesCataract SurgeryndrabramsPas encore d'évaluation
- Management of CRAODocument3 pagesManagement of CRAOvenniePas encore d'évaluation
- Hypertensi RetinopatiDocument32 pagesHypertensi RetinopatirifaiPas encore d'évaluation
- CNLDO JurnalDocument6 pagesCNLDO JurnalKhairul FitrahPas encore d'évaluation
- Quick Uveitis PDFDocument59 pagesQuick Uveitis PDFirinaPas encore d'évaluation
- 3 Piece IOL SCL FixDocument6 pages3 Piece IOL SCL FixTvrtka BenašićPas encore d'évaluation
- Corneoscleral T&S - PrinciplesDocument10 pagesCorneoscleral T&S - PrinciplesMuhammad SyamilPas encore d'évaluation
- Diseases of Retina: The 4th Affilitated Hospital of China Medical University Eye Hospital of China Medical UniversityDocument76 pagesDiseases of Retina: The 4th Affilitated Hospital of China Medical University Eye Hospital of China Medical UniversityIcha NathaniaPas encore d'évaluation
- Intraocular Gas TemponadDocument15 pagesIntraocular Gas TemponadLoay T. DweikPas encore d'évaluation
- Retinal Applications of Swept Source Optical Coherence Tomography (OCT) and Optical Coherence Tomography Angiography (OCTA)Document52 pagesRetinal Applications of Swept Source Optical Coherence Tomography (OCT) and Optical Coherence Tomography Angiography (OCTA)zhu zhuotingPas encore d'évaluation
- Chapter 11 Eye & Vision DisordersDocument72 pagesChapter 11 Eye & Vision DisordersMYLENE GRACE ELARCOSAPas encore d'évaluation
- PhacoemulsificationDocument54 pagesPhacoemulsificationIshita Kinra100% (1)
- Veno Occlusive Disease of RetinaDocument81 pagesVeno Occlusive Disease of RetinaPreetiPas encore d'évaluation
- Eye Docs UveitisDocument90 pagesEye Docs UveitisMuneeb ShahzadPas encore d'évaluation
- 30secondary GlaucomasDocument19 pages30secondary GlaucomasShari' Si WahyuPas encore d'évaluation
- Anesthesia Management of Ophthalmic Surgery in Geriatric Patients PDFDocument11 pagesAnesthesia Management of Ophthalmic Surgery in Geriatric Patients PDFtiaraleshaPas encore d'évaluation
- Applied Anatomy and Physiology of CorneaDocument116 pagesApplied Anatomy and Physiology of CorneaJoubertnassif100% (1)
- Advantages and Disadvantages of Aphakics Correction, Types of Aphakic Correction, Problems of Newly Corrected AphakicsDocument78 pagesAdvantages and Disadvantages of Aphakics Correction, Types of Aphakic Correction, Problems of Newly Corrected AphakicsTika100% (1)
- Oculomotor Nerve: Arista Prima NDocument7 pagesOculomotor Nerve: Arista Prima NArista Prima N100% (1)
- Understanding Visual Fields Part I Goldmann PerimeDocument11 pagesUnderstanding Visual Fields Part I Goldmann PerimeAngelaPas encore d'évaluation
- Corneal Ulcer: Prepared By: Renuka Shrestha Roll No: 29 PBBN 3rd Year SMTCDocument41 pagesCorneal Ulcer: Prepared By: Renuka Shrestha Roll No: 29 PBBN 3rd Year SMTCsushma shresthaPas encore d'évaluation
- International Council of Ophthalmology's Ophthalmology Surgical Competency Assessment Rubrics (ICO-OSCAR)Document4 pagesInternational Council of Ophthalmology's Ophthalmology Surgical Competency Assessment Rubrics (ICO-OSCAR)zaidoonys1Pas encore d'évaluation
- Diagram For Ophtal NoteDocument7 pagesDiagram For Ophtal NoteSiam Weng LoongPas encore d'évaluation
- RvoDocument43 pagesRvoOrchlon LkPas encore d'évaluation
- 2.4 Eye Disorders: 2.4.1 Refractive Errors (Myopia, Hyperopia, Presbyopia, Astigmatism)Document2 pages2.4 Eye Disorders: 2.4.1 Refractive Errors (Myopia, Hyperopia, Presbyopia, Astigmatism)Amry Irsyada YusufPas encore d'évaluation
- Unit3 Images&GraphicsDocument23 pagesUnit3 Images&GraphicsNec'x RosetePas encore d'évaluation
- Module 4 - 5 in TLE 7Document11 pagesModule 4 - 5 in TLE 7CBD COLLEGE INCPas encore d'évaluation
- A Comparison of The Effects of Orthokeratology Lens, Medcall Lens, and Ordinary Frame Glasses On The Accommodative Response in Myopic ChildrenDocument19 pagesA Comparison of The Effects of Orthokeratology Lens, Medcall Lens, and Ordinary Frame Glasses On The Accommodative Response in Myopic ChildrenAmanda CesaPas encore d'évaluation
- Photography RubricDocument1 pagePhotography Rubricsaralynn83Pas encore d'évaluation
- Catalogo MexicoDocument36 pagesCatalogo MexicoRafael V LopezPas encore d'évaluation
- HDR CFA Image RenderingDocument4 pagesHDR CFA Image RenderingJuanma FontPas encore d'évaluation
- Photoshop CS4 - MasteryDocument4 pagesPhotoshop CS4 - MasteryS Antoni De RotiPas encore d'évaluation
- Anatomy-Physiology of The Eye DNB Ophthalmology Theory DnbCentral - inDocument66 pagesAnatomy-Physiology of The Eye DNB Ophthalmology Theory DnbCentral - inporuPas encore d'évaluation
- Dental Clinic PowerPoint TemplatesDocument48 pagesDental Clinic PowerPoint TemplatesMedden MedenPas encore d'évaluation
- Coffee PowerPoint TemplatesDocument48 pagesCoffee PowerPoint TemplatesNanin Ashifaul UPas encore d'évaluation
- CME Camera OperationDocument42 pagesCME Camera OperationDenis LedentPas encore d'évaluation
- The Human Eye: Structure and Function: R M F. LDocument1 pageThe Human Eye: Structure and Function: R M F. LzodiacgeminyPas encore d'évaluation
- NCM104 MS2 - Course Unit 13 - Review of The Anatomy and Physiology of The Eyes & AssessmentDocument5 pagesNCM104 MS2 - Course Unit 13 - Review of The Anatomy and Physiology of The Eyes & AssessmentJordz PlaciPas encore d'évaluation
- Parafraseo (Parcial de Ingles)Document2 pagesParafraseo (Parcial de Ingles)Jamaal BarrierPas encore d'évaluation
- CH 5 - The Near Vision Complex, P. 85-100Document16 pagesCH 5 - The Near Vision Complex, P. 85-100ivethmarroquin100% (1)
- Color Index InformationDocument4 pagesColor Index InformationdamiendamPas encore d'évaluation
- Survey On Scene Classification ApproachesDocument6 pagesSurvey On Scene Classification Approacheslavanya anbazhaganPas encore d'évaluation
- Automatic Defect Detection and Classification of Ceramic TilesDocument7 pagesAutomatic Defect Detection and Classification of Ceramic TilesAayan ShahPas encore d'évaluation
- Splendor Card List With PicsDocument5 pagesSplendor Card List With Picskorkie100% (1)
- Eyes Lecture 1Document4 pagesEyes Lecture 1Rue Cheng MaPas encore d'évaluation
- Photostress TestDocument2 pagesPhotostress TestAnumeha JindalPas encore d'évaluation
- Large FormatDocument3 pagesLarge FormatEdward StapelPas encore d'évaluation
- Dip Lecture NotesDocument210 pagesDip Lecture NotesR Murugesan SIPas encore d'évaluation
- Bayer FilterDocument4 pagesBayer FilterMoji PiyapongPas encore d'évaluation
- Atlas HalftoneDocument36 pagesAtlas HalftoneRomeu NatalePas encore d'évaluation
- CCS2 Ebook Preview PDFDocument32 pagesCCS2 Ebook Preview PDFashutoshkumar5549Pas encore d'évaluation
- Moptim IRef Brochure enDocument3 pagesMoptim IRef Brochure enDiego A. Pérez CruzPas encore d'évaluation
- Early Photocoagulation For Diabetic Retinopathy: ETDRS Report Number 9Document20 pagesEarly Photocoagulation For Diabetic Retinopathy: ETDRS Report Number 9Bernardo RomeroPas encore d'évaluation
- Zoomlens Calibration With Zoom-And Focus-Related Intrinsic Parameters Applied To Bundle AdjustmentDocument11 pagesZoomlens Calibration With Zoom-And Focus-Related Intrinsic Parameters Applied To Bundle AdjustmentSalsabila AnandaPas encore d'évaluation