Académique Documents
Professionnel Documents
Culture Documents
PIIS170121631634525X Dilaa 3
PIIS170121631634525X Dilaa 3
Transféré par
keysayTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
PIIS170121631634525X Dilaa 3
PIIS170121631634525X Dilaa 3
Transféré par
keysayDroits d'auteur :
Formats disponibles
OBSTETRICS
OBSTETRICS
Diagnosis of Premature Rupture of Membranes:
Inspiration From the Past and Insights for the
Future
Amira El-Messidi, MD, FRCSC, RDMS,1 Alan Cameron, MD, FRCOG, FRCP (Glas)2
1
Division of Maternal-Fetal Medicine, Department of Obstetrics and Gynecology, Royal Victoria Hospital, McGill University, Montreal QC
2
Fetal Medicine, Department of Obstetrics and Gynaecology, The Queen Mother’s Hospital, Glasgow, Scotland
Abstract en anglais. Ces articles ont été analysés et les résultats ont été
résumés en fonction du test diagnostic évalué.
Objective: To review the diagnostic methods described to confirm
premature rupture of membranes during pregnancy, and to assess Conclusion : La reconnaissance de l’importance de la confirmation
their effectiveness in establishing the diagnosis. de la rupture des membranes chorioamniotiques et de ses
difficultés est omniprésente dans les publications passés et
Data Sources and Extraction: The medical literature was searched présentes du domaine de l’obstétrique. La subjectivité, la faible
to identify all relevant studies and reviews on methods for diagnosis sensibilité et les premières techniques diagnostiques visant la
of membrane rupture published in English up to January 31, 2009. confirmation de la rupture des membranes ont donné lieu à des
Medline and the Cochrane databases were searched, and percées techniques faisant appel à des marqueurs biochimiques.
reference lists in identified articles were also examined. Articles Aucun de ces tests biochimiques ne s’est démarqué, et ce, malgré
not available through journals’ online editions were retrieved by le fait que des techniques novatrices faisant appel à des
manual search. marqueurs placentaires (comme l’alpha-microglobuline-1
placentaire) puissent fournir une future solution au problème
Study Selection: We identified 71 original studies and reviews on
que pose le diagnostic de la rupture des membranes
diagnostic methods of chorioamniotic membrane rupture published
chorioamniotique.
in English. These articles were reviewed and results were
summarized based on the diagnostic test assessed. J Obstet Gynaecol Can 2010;32(6):561–569
Conclusion: Recognition of the importance of and difficulties in
confirmation of rupture of the chorioamniotic membranes pervades INTRODUCTION
past and present obstetric publications. The subjectivity and poor
sensitivity of early diagnostic techniques for confirmation of remature rupture of membranes may occur at term or
ruptured membranes sparked technical advancements using
biochemical markers. None of these biochemical tests have
P immediately preceding labour, or it may be an unex-
gained popularity, although novel techniques involving placental pected complication during the preterm period, when it is
markers such as placental alpha microglobulin-1 may provide a
future solution to the problem of diagnosing chorioamniotic referred to as preterm premature rupture of membranes.
membrane rupture.
Chorioamniotic membrane rupture may have several
underlying causes, although in many cases PROM and
Résumé
PPROM will not have recognized etiologies. The
Objectif : Analyser les méthodes diagnostiques décrites pour pathophysiology leading to PROM at term has been shown
confirmer la rupture prématurée des membranes pendant la
grossesse, ainsi qu’afin d’en évaluer l’efficacité pour ce qui est to be different from the pathophysiology leading to PPROM.
de l’établissement du diagnostic. At term, weakening of the membranes may result from
Sources et extraction des données : Des recherches ont été physiologic changes combined with shearing forces induced
menées dans la littérature médicale en vue d’identifier toutes by contractions.1–4 Generalized weakness of the membranes
les études et analyses pertinentes portant sur les méthodes de
procéder au diagnostic de la rupture des membranes qui ont été
has been more difficult to identify with prematurely ruptured
publiées en anglais jusqu’au 31 janvier 2009. Des recherches membranes.5 PPROM may result from a focal deficit rather
ont aussi été menées dans Medline et les bases de données than a generalized weakness of the membranes.6
Cochrane, et les listes de références des articles identifiés ont
également été examinées. Les articles n’étant pas disponibles Term PROM complicates approximately 8% of pregnancies.7
par l’intermédiaire des éditions électroniques des revues
spécialisées ont été récupérés par recherche manuelle.
Among these, approximately 50% of affected women will
begin labour spontaneously within 12 hours, 70% within 24
Sélection des études : Nous avons identifié 71 études et analyses
originales portant sur les méthodes permettant de diagnostiquer hours, 85% within 48 hours, and 95% within 72 hours.7–9
la rupture des membranes chorioamniotiques qui ont été publiées Fetal morbidities associated with term PROM include
JUNE JOGC JUIN 2010 l 561
OBSTETRICS
ascending infection and in utero cord compression.7 Mater- examination is negative or inconclusive; they subsequently
nal risks of term PROM include chorioamnionitis and return with clearly identifiable rupture of the membranes.
postpartum febrile morbidity.7,9 Whether these cases represent preliminary minimal
Preterm PROM, a complication of 2% to 20% of all transudation of fluid across weakened membranes or minimal
deliveries,10 is a known important contributor to maternal leakage around a firmly applied fetal presenting part cannot
and perinatal morbidity and perinatal mortality. Latency in be determined. In approximately 20% to 25% of cases,
PPROM, defined as the interval between PROM and birth,7 rupture of membranes is not grossly apparent.10,19 A patient’s
is known to be inversely related to gestational age at rupture, history may suggest membrane rupture, but test results are
and is also related to a multitude of other factors, including non-confirmatory, creating an obstetrical dilemma. Early
number of fetuses,11 severity of oligohydramnios,12 and accurate diagnosis of membrane rupture would allow for
myometrial thickness,13 and the existence of maternal or gestational age-specific interventions to optimize perinatal
obstetrical complications. The major cause of perinatal outcome and minimize serious complications.20 Therefore,
morbidity and mortality associated with PPROM is the search for an ideal test to diagnose membrane rupture
prematurity.7 Morbidities related to prematurity include definitively with no delay continues.
respiratory distress syndrome, necrotizing enterocolitis, Although initial studies may be encouraging, diagnostic
interventricular hemorrhage, cerebral palsy, and sepsis.7 techniques are usually found subsequently to be limited by
Other complications include in utero umbilical cord com- inaccuracies from false positives and false negatives with
pression, cord prolapse and fetal distress, fetal poorer sensitivities and specificities than originally anticipated.
malpresentation, placental abruption, chorioamnionitis The ideal test should be simple, rapid, inexpensive, and
with subsequent endometritis, and risk of operative delivery non-invasive. Optimally, the accuracy of the test should not
from this multitude of factors.7 Maternal sepsis is a rare but be hampered by the presence of blood, semen, infected
life-threatening complication reported in nearly 1% of cases.7 urine, or other contaminants. An accurate biochemical marker
For over 70 years, there has been controversy among health for membrane rupture should have a high concentration in
care professionals about the optimal approach to clinical the amniotic fluid, a low concentration in maternal blood,
assessment and diagnosis of prematurely ruptured membranes. and an extremely low background concentration in
In most cases, membrane rupture can be confirmed by doc- cervicovaginal discharge with intact membranes.10
umenting amniotic fluid leakage from the cervical os with We sought to review the diagnostic methods currently used
visualization of pooling in the posterior vaginal fornix.14 to confirm premature rupture of membranes and to assess
However, the diagnosis of PROM is difficult if there is a their effectiveness in establishing the diagnosis.
slow fluid leak or any bleeding, or when the classic “gush of fluid”
does not occur.15 In addition, the relatively small amount of METHODS
amniotic fluid present early in gestation further challenges
the diagnosis of ruptured membranes.16 Ladfors et al.17 We searched Medline and the Cochrane databases for all
showed that even later in pregnancy (after 34 weeks), speculum relevant studies and reviews published in English on
examination for visualization of amniotic fluid carries a accuracies of diagnostic methods for the diagnosis of rupture
12% false negative rate when no fluid is seen. In 1951, of the membranes up to January 31, 2009. Key words used
Schumann18 described the “two sac” theory of membrane for the Medline search were “premature rupture of membranes,”
rupture: he stated that amniotic fluid can dissect between “amniotic fluid,” “diagnosis,” and “tests.” Articles not
the two layers of membranes and produce a bulge that ruptures available online were retrieved by manual search. We found
into the vagina, leaving one intact layer with remaining fluid no Cochrane reviews of diagnostic methods of PROM, as
enclosed and appearing to rupture at a later time. In such discussed in this report. The studies identified showed evidence
cases, women give a history of fluid leakage, and tests for from levels II-2, II-3, and III, according to ranking of The
leakage should be positive, although membranes appear clin- Canadian Task Force on Preventive Health Care.21,22
ically to be intact at delivery. Occasionally, women present
MICROSCOPIC FETAL CELL IDENTIFICATION
with a history suspicious for membrane rupture, but clinical
A literature review by Friedman et al.23 described the first
microscopic technique for identification of fetal particles in
ABBREVIATIONS amniotic fluid, developed by Philipp et al in 1929 and
AFI amniotic fluid index published in the German literature. In this technique, fetal
PAMG-1 placental alpha-microglobulin-1 lanugo hairs were identified in amniotic fluid. This was presumed
PROM premature rupture of membranes to be incontrovertible evidence of membrane rupture when
PPROM preterm premature rupture of membranes identified in vaginal secretions. However, because of the
562 l JUNE JOGC JUIN 2010
Diagnosis of Premature Rupture of Membranes: Inspiration From the Past and Insights for the Future
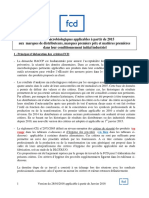
Accuracy of diagnostic tests for PROM
Discriminatory Patients, n SN, % SP, % FN, % FP, %
concentration Sampling Mean Mean Mean Mean Mean
Test used for diagnosis Mean (range) site (range) (range) (range) (range) (range)
Fetal cells (bromthymol N/A Vagina 239 90.2 98.4 7.5 1.7
blue)34,36 (176–239) (85.7–94.7) (97.4–99.3) (0.6–14.3) (0.7–2.6)
pH 19,23,31,39,40,46,54,55,57,59,62 ³ 6.5 Vagina 125 90.2 79.3 12.4 28.2
(6.0–7.0)35,36,55,57,59 (46–250) (81.3–100.0) (16.0–100.0) (0–33.3) (0–100.0)
Fetal cells (Masson stains) 24 N/A Vagina 275 94.2 99.0 5.8 1.0
Fetal cells (Papanicolaou N/A Vagina 75 92.8 92.7 4.3 7.4
stain)23,28 (50–100) (92.0-93.5) (91.3–94.0) (2.0–6.5) (6.0–8.7)
Fetal cells (Pinacyanol N/A Vagina 150 88.3 95.4 11.7 3.7
stain)23,30,31 (100–250) (71.0–98.7) (91.7–98.8) (1.3–29) (1.2–8.3)
Fetal cells (Acridene N/A Vagina 200 75.5 90 24.6 10.0
orange stain)23,32 (100–300) (61.2–89.7) (87.3–92.7) (10.3–38.8) (7.3–12.7)
Fetal cells (Nile N/A Vagina 106 89.5 98.6 10.6 1.5
blue sulphate)23,33 (100–111) (80.7–98.2) (97.1–100.0) (1.8–19.3) (0–2.9)
Crystallization23,37,38-40,43,54,74 N/A Vagina 198 90.8 95.3 4.4 4.7
(51–509) (62.0-98.5) (88.2–100.0) (1.2–12.9) (0.0–11.8)
History alone23 N/A N/A 100 90.3 88.4 9.7 11.6
23
History + pH + crystalization N/A Vagina 100 90.8 95.6 9.2 4.4
History + pH + Nile Blue stain23 N/A Vagina 100 87.1 92.7 12.9 7.3
History + Crystallization + Nile N/A Vagina 100 87.1 95.6 12.9 4.4
Blue stain23
History + ultrasound + N/A N/A 83 85.1 78.6 11.1 21.4
crytallization74
pH + Crystallization + Nile N/A Vagina 100 90.8 95.6 9.2 4.4
Blue stain23
AmnioInjection Evans blue N/A Amnio- 18 100.0 100.0 0.0 0
T–182447 centesis
DAO19,58,67 22.5 µU/L19, 67 Vagina 168 88.9 98.3 8.5 1.7
(100–272) (83.0–100.0) (95.0–100.0) (0–17.0) (0–5.0)
3.32 log glucose + log fructose49 17.7279 N/A 215 98.9 96.0 7.7 2.6
continued
scant amounts of fetal lanugo hair in amniotic fluid and the whom the integrity of the chorioamniotic membrane could
fact that such hair was present in amniotic fluid only later in not be determined by visualization of fluid on speculum
pregnancy, this method never gained popularity. As this examination. Fetal cell staining with pinacyanole to identify
study was not published in the English language, statistical vernix caseosa cells in such cases showed high accuracy
data are not shown in the Table. rates (97%), similar to those in earlier studies among
Subsequent diagnostic tests were based on cytologic patients with clinically confirmed membrane rupture.
inspection for fetal squamous cells in the vagina. Interest in Although fetal cell staining techniques were considered
cytologic diagnosis was based on the noted absence of stain rapid, simple, and durable, concerns about inaccuracies
within the cytoplasm and nucleus of vernix caseosa cells emerged. Contamination from the powder on examination
compared with vaginal squamous cells.24 Investigators gloves gave false positive results as anuclear granules
searched for fetal cells in vaginal fluid using diverse stains mimicked fetal cells,31 and hypercornified vaginal cells also
including Masson stain,24 Sudan III to demonstrate fetal fat simulated anucleate fetal cells.32 False negatives resulted
particles,25–27 Papanicolaou stain,28,29 pinacyanole stain,30,31 from the subjectivity of inspection, having insufficient
acridene orange stain,32 and Nile blue sulphate stain.33 cellular material,32 or after a prolonged time interval from
Recognizing the challenge to diagnose PROM in clinically membrane rupture. Accuracy rates appear to diminish with
equivocal cases, Averette et al.30 studied 100 patients in increased duration between presumed membrane rupture
JUNE JOGC JUIN 2010 l 563
OBSTETRICS
Table continued
Discriminatory
concentration Patients, n SN, % SP, % FN, % FP, %
Mean Sampling Mean Mean Mean Mean Mean
Test used for diagnosis (range) site (range) (range) (range) (range) (range)
Prolactin RIA50,51,52 3mU/mL,59 Vagina 57 88.0 85.0 68.0 15.0
2ng/mL,51 (20–100) (76.0–100.0)51,52 (70.0–100.0)51,52 (0–30.0)51,52
20.2µIU/mL52
AFP (RIA)60,67,76,77,80 53.3 µg/L Vagina 122 80.6 91.9 5.4 8.1
(2-125) (52–312) (17.6–100.0), (80.0–97.4), (0.0–16.0), (2.6–20.0),
NR60 NR60 NR60 NR60
AFP (RIA)57,58,59 77.5 µg/L Cervix 89 92.0 86.9 8.0 13.2
(30-125) (46–131) (84.0–100.0) (85.7–88.0) (0–16.0) (12.0–14.3)
human placental lactogen 31 ng/mL Vagina 52 NR NR NR NR
(hPL) RIA51
fFN monoclonal assay 50 ng/mL Vagina 160 93.6 65.7 13.1 17.0
(ROM check)58,59,63,64,65 (54–406) (90.0–98.2) (26.8–97.0) (3.0–25.0) (6.0–28.0)
fFN monoclonal assay 25 ng/mL Vagina 46 87.5 92.9 11.9 7.1
(ROM check)59
IGFBP-1 immunoenzyme 35 µg/L Vagina, 130 84.9 92.8 14.7 7.3
(PromTest)19, 46, 65,71,72,73,74 (3-100) cervix72 (54–174) (74.4–100.0) (71.4–98.2) (0–39.2) (1.8–28.6)
IGFBP-1 dipstick 400 µg/L Amniocentesis 20 NR NR NR NR
(ActimPROM)10
Lactate68 ³4.5 mmol/L Vagina 200 86 92 92 87
b hCG (ELCIA) 52,60,61,62
46.4 mIU/mL Vagina 137 83.9 89.5 9.1 10.5
(100–188) (68.0–100.0) (84.2–95.0) (0.0–25.0) (5.0–16.0)
Ultrasound amniotic < 80 mm N/A 151 94.0 91.0 6.2 9.0
fluid index46
Creatinine concentration 0.36 mg/dL Vagina 114 100.0 100.0 0.0 0.0
assay69,70 (88–139)
Urea concentration70 12 mg/dL Vagina 139 100.0 100.0 0.0 0
PAMG-1 5 ng/mL Vagina 194 98.8 93.8 1.2 6.3
(AmniSure™)76,77 (184–203) (98.7–98.9) (87.5–100.0) (1.1–1.3) (0.0–12.5)
PAMG-1 (AmniSure™)10 5 ng/mL Amniocentesis 20 NR NR NR NR
AmnioSense™ pH> 5.2 N/A 69 99.2 70.0 0.85 30.0
absorbent pad15,78 (34–103) (98.3–100.0) (65.0–75.0) (0–1.7) (25.0–35.0)
Legend: SN: sensitivity; SP: specificity; FN: false negative; FP: false positive; DAO: diamine oxidase; IGFBP-1: insulin growth factor binding protein-1;
PAMG-1: placental alpha microglobulin-1; bhCG: beta subunit human chorionic gonadotropin; fFN: fetal fibronectin; AFP: alpha fetoprotein; RIA: radioimmunoassay;
NR: not reported; N/A: not applicable
and diagnostic testing. Early authors including King34 and LITMUS PAPER AND pH TESTING
Bourgeois24 reported 57% and 81.8% accuracy rates
respectively, beyond the initial 24-hour period of membrane Litmus paper testing began development at approximately
rupture. This was later confirmed by others, and shorter the same time as fetal cell staining methods. Because of the
intervals to testing were shown to affect rates of diagnostic difference in pH of vaginal secretions (4.5 to 5.5) and
accuracy.23 amniotic fluid (7.0 to 7.5), it was rightly assumed that the
pH of vaginal secretions would rise when contaminated by
escaping amniotic fluid.35 This assumption prompted pre-
As novel methods were developed, older cytologic techniques liminary experiments with bromthymol blue dye and, later,
began losing popularity, because they were time-consuming, nitrazine applicators. Although similar in principle to
required trained cytologists, were ineffective before 32 weeks’ bromthymol blue, a reported advantage of nitrazine is the
gestation, and provided an uncertain diagnosis of membrane complete change in colour of the applicator when exposed
rupture.29 to amniotic fluid in vaginal secretions.36 Impregnated with
564 l JUNE JOGC JUIN 2010
Diagnosis of Premature Rupture of Membranes: Inspiration From the Past and Insights for the Future
sodium-dinitro-phenylozonapthol-disulphonate, nitrazine Indeed, these authors showed a precipitous increase in error
paper showed promising early results in detecting membrane rate when the time interval between membrane rupture and
rupture, with accuracies of 100%35 and 98.9%36 in clinically sampling exceeded two hours.23 False negative tests were
ruptured cases, and similarly high rates of accuracy among more commonly associated with prolonged rupture. None
intact cases. This preliminary high optimism regarding of the traditional procedures proved entirely satisfactory in
nitrazine testing decreased by the 1960s,31,37 because of false isolation, but combinations of any three of the following
positive results from vaginal infections, blood, semen, alka- produced a diagnostic accuracy of 93.1%23:
line urine or alkaline antiseptics, and false negatives in cases
1. a positive history,
of minimal leakage from chronic membrane rupture or
“high leak” of the membranes.15 2. a positive nitrazine test,
3. fluid crystallization, or
AMNIOTIC FLUID CRYSTALLIZATION
4. Nile blue sulphate staining.
Amniotic fluid crystallization, created primarily by the
sodium chloride and protein content, began to dominate ULTRASOUND ASSESSMENT OF
cytologic stains, with reported accuracies in clinically AMNIOTIC FLUID VOLUME
ruptured cases ranging from 73.0% to 98.5%.26,27,32,37–40
Screening for arborization provided an accuracy of 97.8% In the late 20th century, it was theorized that the
compared with 87.3% for litmus paper testing.37 Interest- sonographic identification of oligohydramnios would
ingly, Tricomi et al.37 suggested that fluid for examination develop after membrane rupture,44 thereby facilitating diag-
should be aspirated from the vagina no further than 3 cm nosis and subsequent management. Manning et al.45 initially
from the introitus to avoid contamination and false positive described a technique for measuring by ultrasound the
ferning results from cervical mucus lying in the posterior deepest vertical pool of amniotic fluid in patients with
fornix. Initial optimism with low false negative rates intrauterine growth restriction. This method was later used
changed as missed diagnoses in the presence of blood, to assess membrane rupture; it was shown that ultrasound
meconium, or heavy leukorrhea became recognized.23 False quantification of the deepest amniotic fluid pocket is of
positive results were subsequently attributed to fingerprints, poor quality in confirming membrane rupture.44 No signifi-
semen, or cervical mucus.23,41,42 cant difference was found in the mean depth of amniotic
fluid pocket between 100 patients with confirmed term
In most ferning specimens tested in early studies,23,26,37–40 PROM and 51 patients with intact membranes.44
sensitivity and specificity analyses were performed on Oligohydramnios may not be detected in patients with
women in labour, in whom there was certainty about the confirmed PROM, possibly because drainage may become
diagnosis of membrane rupture.43 In most clinical situa- intermittent or even stop once the presenting part descends
tions, however, the test is intended for patients who have and acts as a plug, preventing further drainage.44 Robson et
equivocal rupture. De Haan et al.43 showed that the modest al. suggested that a significant amount of amniotic fluid
diagnostic reliability of the fern test compared with earlier needs to drain rapidly and continuously for
published data is at least partly due to differences in study oligohydramnios to occur, especially because the fluid is
populations (i.e., whether the women were in labour or replaced to varying degrees by the fetus.44 Erdemoglu et
not). These authors showed false positive and false negative al.46 showed that a reduction in the four-quadrant AFI
rates of 11.8% and 2.0%, respectively, in labouring women below 80 mm did not reliably identify cases of suspected
tested for amniotic fluid crystallization, compared with membrane rupture by history with negative visualization of
rates of 21.2.% and 40.6%, respectively, in women not in fluid by speculum examination. The measurement of AFI
labour.43 Thus, the result of the fern test became viewed as offers no advantage over measurement of a single vertical
supportive rather than conclusive for non-labouring pocket of fluid in cases where ultrasound is used to evaluate
women with non-specific vaginal fluid loss. possible membrane rupture.
COMBINATION OF DIAGNOSTIC TESTS INTRA-AMNIOTIC DYE INJECTION
Many early studies either tested one method for diagnosis By 1970, amniocentesis with injection of dye to confirm
of membrane rupture or compared two methods. Friedman amniotic membrane rupture had become a commonplace
et al.23 were the first to test individual methods as well as dif- procedure; it was thought to be safe and had high patient
ferent combinations of tests, which more commonly acceptability rates.47 Prior to amniocentesis, intravenous
reflects true clinical practice. They also attempted to corre- injection of radioisotope was performed for placental local-
late the time of testing with the time of presumed rupture. ization, and the amnio-injection was performed under local
JUNE JOGC JUIN 2010 l 565
OBSTETRICS
anaesthesia. Interestingly, the two reported disadvantages testing complexity, and low test sensitivities in cases of
of the procedure at that time were related to difficulty in equivocal rupture.
diagnosis in the presence of meconium-stained fluid and
the possibility of neonatal skin staining for 48 hours after PLACENTAL ALPHA-MICROGLOBULIN-1
dye injection.47 Several types of stains have been used for
amnio-injections, with safety hazards reported only for Initially isolated in Moscow in 1975,75 PAMG-1 has under-
methylene blue (see below). gone recent evaluation for diagnostic testing in PPROM.
This 34kDa placental glycoprotein is abundant in amniotic
Although ultrasonographically guided transabdominal fluid (2000–25 000 ng/mL), with much lower concentra-
instillation of indigo carmine dye (1 mL of dye in 9 mL of tions in maternal blood (5–25 ng/mL).20 The protein is
sterile normal saline) and observation for fluid passage present in negligible amounts in cervicovaginal secretions
transvaginally is designated an “unequivocal” diagnostic with intact membranes (0.05–0.2ng/mL).76 The 1000- to
method for confirmation of membrane rupture,14 this inva- 10 000-fold difference in concentration between amniotic
sive test carries increased maternal and fetal risk. Inherent fluid and cervicovaginal secretions stimulated interest in a
risks of intra-amniotic dye injection include trauma, bleeding, PAMG-1 immunoassay. Marketed as AmniSure (AmniSure
infection, and preterm labour.48 While strengthening International, Cambridge, MA), the assay’s minimum detec-
diagnostic certainty, a “negative dye test” may occur if the tion threshold for PAMG-1 is 5 ng/mL, sufficient for 99%
membranes seal after previous amniotic fluid leakage. accuracy with minimal false negatives. PAMG-1 can be
detected with as little as 0.25 µL of amniotic fluid in 1 mL of
GLUCOSE AND FRUCTOSE MEASUREMENTS vaginal secretions.76 In the presence of blood or vaginitis,
Gorodeski et al.49 examined the difference between the background level of PAMG-1 can occasionally reach a
amniotic fluid and cervicovaginal mucus in their concentra- maximum of 3 ng/mL.76 False-positive results with use of
tions of solutes. During pregnancy, glucose and fructose are the AmniSure assay seem very unlikely, although these may
present in high concentrations in cervical mucus, with appear with increased use.77 Further, assay of PAMG-1
reported means of 240 mg/100 mL and 30.4 mg/100 mL, appears to be reliable over a wide range of gestational ages
respectively.49 Amniotic fluid concentrations are noticeably (11 to 42 weeks), and proved superior to conventional com-
lower, with mean concentrations of 39 mg/100 mL and bined clinical tests involving visualization of fluid pooling in
3.3mg/100 mL, respectively. Gorodeski et al.49 showed that the posterior fornix, arborization, and nitrazine testing.77
low values of glucose and fructose are found in amniotic This test is currently available in Europe and was recently
fluid aspirated in a true case of membrane rupture. Best approved by the Food and Drug Administration for use in
results are obtained with a calculated linear sum of the values the United States. AmniSure is a novel rapid, non-invasive
(3.32 log glucose + log fructose). These authors reported no bedside test that may be very helpful in diagnosis of difficult
confounding by meconium or vaginal discharge. cases without visible leakage. Further studies are needed to
This technique is fairly impractical in testing for membrane assess the reliability of the test according to the time from
rupture, and further studies have not expanded upon differ- membrane rupture.
ential carbohydrate gradients.
NON-INVASIVE ABSORBENT PAD
MODERN METHODS
Efforts to be able to confirm chorioamniotic membrane
Because of the limitations of available testing methods, rupture with minute amounts of amniotic fluid have
investigators have sought alternative markers in vaginal recently led to the development of the absorbent pad,
amniotic fluid, such as prolactin50–52, alpha-fetoprotein,51–59 AmnioSense. This 12 ´ 4 cm pad has a central strip that
b-subunit of human chorionic gonadotropin,52,60–62 fetal changes colour on contact with fluid with a pH > 5.2.15,78
fibronectin,58,59,63–66 diamine oxidase,19,58,67 lactate,68 After contact with urine, the strip reverts to its original col-
creatinine,69,70 urea,70 and insulin growth factor binding our when dry. This is due to the detachment of conju-
protein-1, previously called placental protein gate-based nitrazine molecules by the urine ammonium
12.10,19,46,65,66,71–74 Interest in assessment of these markers ions.15 AmnioSense has undergone cytotoxicity and skin
stems from their high concentrations in amniotic fluid com- irritation and sensitization testing, and it complies with the
pared with normal vaginal secretions, but all require special US Pharmacopoeia Guidelines.15 In a study of 34 women
laboratory equipment and training.14 Although these markers presenting with suspected membrane rupture, the
are useful for patients with intact membranes or unequivocal AmnioSense pad initially showed 100% sensitivity; overall
membrane rupture, they remain unpopular due to cost, specificity was 75%, but when women with bacterial
566 l JUNE JOGC JUIN 2010
Diagnosis of Premature Rupture of Membranes: Inspiration From the Past and Insights for the Future
vaginosis or Trichomonas vaginalis were excluded from CONCLUSION
analysis, the specificity increased to 90%.15
Early techniques for establishing the diagnosis of ruptured
In a recent study, Mulhair et al.78 compared the reliability of membranes included fetal cell staining, vaginal pH determi-
the absorbent pad test with a standard of amniotic fluid nation and amniotic fluid crystallization. Criticism of such
pooling in the posterior fornix on speculum examination in methods emphasized subjectivity in interpretation, poor
a cohort of 139 women. They found a specificity of 65.0% sensitivity, and numerous confounding factors cross-reacting
and a sensitivity of 98.3% for the AmnioSense pad. The two with substances in the vaginal reservoir.
studies of the absorbent pad currently available15,78 suggest
The absence of a non-invasive “gold standard” for the diag-
that a negative AmnioSense result indicates intact
nosis of PROM has led to technically advanced biochemical
membranes in term and preterm gestations in 99% of cases.
markers. Despite improved diagnostic value in cases of
A positive result, however, suggests only a 70% chance of
unequivocal membrane rupture or intactness, biochemical
ruptured membranes, and thereby warrants confirmation or
markers lack the sensitivity and specificity required in
further investigations to identify infections (Table).15,78
equivocal cases. They have also not become popular, in
It remains unknown whether potential confounding part, because of cost and complexity in testing.
substances such as semen, blood, or meconium may be In the common clinical situation where a health care provider
distinguished from amniotic fluid by the AmnioSense pad encounters a patient with possible ruptured membranes,
test. As women with negative pad checks are unlikely to diagnostic accuracy is the key to successful management
have ruptured membranes, this would imply decreased and improved perinatal outcome. Nearly one quarter of
need for an uncomfortable and intrusive speculum patients do not present with overt clinical evidence of ruptured
examination. membranes. We believe that recent techniques involving
placental markers such as PAMG-1 and the AmnioSense
SAFETY
absorbent pad, with minute sampling required,
Safety data on diagnostic testing for rupture of non-invasiveness, rapidity of testing, and high accuracy
chorioamniotic membranes show potential adverse rates, may provide a solution to the clinical challenge of
neonatal effects related to intra-amniotic administration of diagnosing ruptured membranes.
methylene blue.79,80 Several cases of neonatal hemolytic
anemia and hyperbilirubinemia, including sepsis and REFERENCES
neonatal death, have been reported after intra-amniotic 1. Lavery JP, Miller CE, Knight RD. The effect of labor on the rheologic
injection of methylene blue.80 These cases involved injection response of chorioamniotic membranes. Obstet Gynecol 1982;60:87–92.
of 3.5 mL of 1% methylene blue solution, resulting in doses of 2. McLaren J, Taylor JD, Bell SC. Increased incidence of apoptosis in
30 to 5mg.80 Even at a lower dose of 10 mg, Cowett et al.79 non-labor affected cytotrophoblast cells in term fetal membranes overlying
the cervix. Hum Reprod 1999;14:895–900.
reported a case of hemolytic anemia and hyperbilirubinemia
3. El Khwad M, Stetzer B, Moore RM, Kumar D, Mercer B, Arikat S, et al.
requiring two exchange transfusions and phototherapy. Term human fetal membranes have a weak zone overlying the lower uterine
These adverse effects could not be attributed to other pole and cervix before onset of labor. Biol Reprod 2005;72:720–6.
causes of neonatal jaundice. The neonate’s skin was discol- 4. Moore RM, Mansour JM, Redline RW, Mercer BM, Moore JJ. The
oured for the first few days of life and methylene blue was physiology of fetal membrane rupture: insight gained from the
determination of physical properties. Placenta 2006;27:1037–51.
identified in the urine during the first day of life.
5. Al Zaid NS, Bou-Resali MN, Goldspink G. Bursting pressure and collagen
Intra-amniotic dye as a marker for confirmation of PROM content of fetal membranes and their relation to premature rupture of the
membranes. Br J Obstet Gynecol 1980;87:227–9.
also poses risk to the mother, including bleeding, infection,
and preterm labour.48 It is also an invasive test used to 6. Parry S, Strauss JF. Premature rupture of the fetal membranes.
N Engl J Med 1998; 338:663–70.
assess a common complaint.
7. American College of Obstetrics and Gynecology Practice Bulletin No. 80.
We were unable to identify any safety data related to the use Premature rupture of membranes. April 2007.
of vaginal swabs, either with or without use of a speculum, 8. Duff P. Premature rupture of the membranes in term patients. Semin
in screening for chorioamniotic membrane rupture. Potential Perinatol 1996;20:401–8.
risks of swabs might include ascending infection. A 9. Hannah ME, Ohlsson A, Farine D, Hewson SA, Hodnett ED, Myhr TL,
non-intrusive method, the AmnioSense absorbent pad, may et al. Induction of labour compared with expectant management for
prelabor rupture of the membranes at term–TERMPROM Study Group.
conceivably lead to negligible rates of infections and skin N Engl J Med 1996; 334:1005–10.
irritation. Neither of the two published studies testing
10. Chen FCK, Dudenhausen JW. Comparison of two rapid strip tests based on
absorbent pads15,78 report any complications from use of IGFBP-1 and PAMG-1 for the detection of amniotic fluid. Am J Perinatol
the product. 2008;25:243–6.
JUNE JOGC JUIN 2010 l 567
OBSTETRICS
11. Myles TD, Espinoza R, Meyer W, Bieniarz A. Preterm premature rupture 32. Kushner DH, Chang IW, Vercruysse JM. Fluorescence microscopy for
of membranes: comparison between twin and singleton gestations. J Matern determination of ruptured fetal membranes by vaginal smear. Obstet
Fetal Neonat Med 1997;6:159–63. Gynecol 1964;23:196–9.
12. Park JS, Yoon BH, Romero R, Moon JB, Oh SY, Kim JC, et al. The 33. Brosens I, Gordon H. The cytological diagnosis of ruptured membranes
relationship between oligohydramnios and the onset of preterm labor using Nile Blue Sulphate staining. J Obstet Gynaecol Br Commonw
in preterm premature rupture of membranes. Am J Obstet Gynecol 1965;72:342–6.
2001;184:459–62. 34. King AG. The determination of rupture of membranes. Am J Obstet
13. Buhimschi CS, Buhimschi IA, Norwitz ER, Sfakianaki AK, Hamar B, Gynecol 1935;30:860–2.
Copel JA, et al. Sonographic myometrial thickness predicts the latency 35. Baptisti A. Chemical test for determination of ruptured membranes.
interval of women with preterm premature rupture of the membranes Am J Obstet Gynecol 1938;35:688–90.
and oligohydramnios. Am J Obstet Gynecol 2005;193:762–70.
36. Abe T. Detection of rupture of fetal membranes with Nitrazine indicator.
14. Mercer BM. Preterm rupture of the membranes: diagnosis and management. Am J Obstet Gynecol 1940;39:400–4.
Clin Perinatol 2004;31:765–82.
37. Tricomi V, Hall JE, Bittar A, Chambers D. Arborization test for the
15. Bornstein J, Geva A, Solt I, Fait V, Schoenfeld A, Shoham HK, et al. detection of ruptured fetal membranes—clinical evaluation.
Nonintrusive diagnosis of premature ruptured amniotic membranes using Obstet Gynecol 1966;27:275–9.
a novel polymer. Am J Perinatol 2006;23:351–4.
38. Smith RW, Callagen DA. Amniotic fluid crystallization test for ruptured
16. Brace RA. Physiology of amniotic fluid volume regulation. membranes. Obstet Gynecol 1962;20:655–60.
Clin Obstet Gynecol 1997;40:280–9. 39. Kovacs D. Crystallization test for the diagnosis of ruptured membranes.
17. Ladfors L, Mattsson LA, Eriksson M, Fall O. Is a speculum examination Am J Obstet Gynecol 1962;83:1257.
sufficient for excluding the diagnosis of ruptured fetal membranes? 40. Ferron M, Bilodeau R. Amniotic fluid crystallization test for ruptured
Acta Obstet Gynecol Scand 1997;76:739–42. membranes. Can Med Assoc J 1963;89:1064–7.
18. Schuman W. Double sac with secondary rupture of the bag of waters during 41. Lodeiro JG, Hsieh KA, Byers JH, Feinstein SJ. The fingerprint, a
labor; a clinical entity, and its explanation from examination of the false-positive fern test. Obstet Gynecol 1989;73:873–4.
membranes. Am J Obstet Gynecol 1951;62:633–8.
42. McGregor JA. Johnson S. “Fig-leaf” ferning and positive nitrazine testing:
19. Gaucherand P, Salle B, Sergeant P, Guibaud S, Brun J, Bizollon CA, et al. semen, a cause of misdiagnosis of premature rupture of membranes
Comparative study of three vaginal markers of the premature rupture of [letter to the editor]. Am J Obstet Gynecol 1985;151:1142–3.
membranes—insulin like growth factor binding protein 1, diamine-oxidase,
43. de Haan HH, Offermans JPM, Smits F, Schouten HJA, Peeters LL. Value
pH. Acta Obstet Gynecol Scand 1997;76:536–40.
of the fern test to confirm or reject the diagnosis of ruptured membranes
20. Park JS, Lee SE, Norwitz ER. Non-invasive testing for rupture of the is modest in nonlaboring women presenting with non-specific vaginal fluid
fetal membranes. Touch Briefings: US Obstetrics and Gynecology 2007; loss. Am J Perinatol 1994;11:46–50.
Issue 1: 13–6. 44. Robson MS, Turner MJ, Stronge JM, O’Herlihy CO. Is amniotic fluid
21. Woolf SH, Battista RN, Anderson GM, Logan AG, Wang E. Assessing the quantitation of value in the diagnosis and conservative management of
clinical effectiveness of preventative maneuvers: analytic principles and prelabour membrane rupture at term? Br J Obstet Gynaecol 1990;97:324–8.
systemic methods in reviewing evidence and developing clinical practice 45. Manning FA, Hill FM, Platt LD. Qualitative amniotic fluid volume
recommendations. A report by the Canadian Task Force on the Periodic determination by ultrasound. Antepartum detection of intrauterine growth
Health Examination. J Clin Epidemiol 1990;43: 891–905. retardation. Am J Obstet Gynecol 1981;139:254–8.
22. Canadian Task Force on the Preventive Health Care. New grades for 46. Erdemoglu E, Mungan T. Significance of detecting insulin-like growth
recommendations from the Canadian Task Force on Preventive Health factor binding protein-1 in cervicovaginal secretions: comparison with
Care. CMAJ 2003;169:207–8. nitrazine test and amniotic fluid volume assessment. Acta Obstet Gynecol
Scan 2004;83:622–6.
23. Friedman ML, McElin TW. Diagnosis of ruptured fetal membranes. Clinical
study and review of the literature. Am J Obstet Gynecol 1969;104:544–50. 47. Atlay RD, Sutherst JR. Premature rupture of the fetal membranes confirmed
by intra-amniotic injection of dye (Evans blue T-1824). Am J Obstet
24. Bourgeois GA. The identification of fetal squames and the diagnosis of
Gynecol 1970;108:993–4.
ruptured membranes by vaginal smear. Am J Obstet Gynecol 1942;44:80–7.
48. Gibbs RS, Blanco JD. Premature Rupture of the membranes. Obstet
25. Von Numers C. A new method of diagnosis of rupture of the membranes. Gynecol 1982;60:671–9.
Acta Obstet Gynecol Scand 1936;16:249–60.
49. Gorodeski I, Paz M, Insler V, Fishel J. Diagnosis of rupture of the fetal
26. Paavola A. Methods based on the study of crystals and fat staining: use in membranes by glucose and fructose measurements. Obstet Gynecol
diagnosing rupture of membranes. Ann Chir Gynaecol Fenn 1958;47:22–8. 1979;53:611–6.
27. Volet B, Morier-Genoud J. The crystallization test in amniotic fluid. 50. Koninckx PR, Trappeniers H, Van Assche FA. Prolactin concentration
Gynaecologia 1960;149:151–61. in vaginal fluid: a new method for diagnosing ruptured membranes.
28. Goldfine S. The detection of ruptured membranes by vaginal smear. Br J Obstet Gynaecol 1981;88:607–10.
Am J Obstet Gynecol 1955;70:109–14. 51. Huber JF, Bischof P, Extermann P, Beguin F, Herrmann WL. Are vaginal
29. Hopman BC, Wargo JD, Werch SC. Cytology of vernix caseosa cells. fluid concentrations of prolactin, a-fetoprotein and human placental
Obstet Gynecol 1957;10:656–9. lactogen useful for diagnosing ruptured membranes? Br J Obstet Gynaecol
1983;90:1183–5.
30. Averette HE, Hopman BC, Ferguson JH. Cytodiagnosis of ruptured fetal
52. Shahin M, Raslan H. Comparative study of three amniotic fluid markers
membranes. Am J Obstet Gynecol 1963;87:226–30.
in premature rupture of membranes: prolactin, beta subunit of human
31. Gall SA, Spellacy WN. Cyologic diagnosis of ruptured membranes. chorionic gonadotropin, and alpha-fetoprotein. Gynecol Obstet Invest
Obstet Gynecol 1964;24:732–5. 2007;63:195–9.
568 l JUNE JOGC JUIN 2010
Diagnosis of Premature Rupture of Membranes: Inspiration From the Past and Insights for the Future
53. Rochelson BL, Richardson DA, Macri JN. Rapid assay-possible application 66. Guibourdenche J, Luton D, Andre E, Noel M, Pourquet D. Rapid detection
in the diagnosis of premature rupture of the membranes. Obstet Gynecol of insulin-like growth factor-binding protein-1 and foetal fibronectin in
1983;62:414–8. cervico-vaginal secretions to diagnose premature membrane rupture. Ann
Clin Biochem 1999;36:388–9.
54. Rochelson BL, Rodke G, White R, Bracero L, Baker DA. A rapid
calorimetric AFP monoclonal antibody test for the diagnosis of preterm 67. Elmfors B, Tryding N. The diagnosis of ruptured fetal membranes by
rupture of the membranes. Obstet Gynecol 1987;69:163–5. measurement of the diamine oxidase (DAO) activity in vaginal fluid.
J Obstet Gynaecol Br Commonw 1974;81:361–2.
55. Hjertberg R, Belfrage P, Eneroth P. Latex agglutination test for 68. Wiberg-Itzel E, Cnattingius S, Nordstrom L. Lactate determination in
a-fetoprotein in the diagnosis of premature rupture of the amniotic vaginal fluids: a new method in the diagnosis of prelabour rupture of
membranes (PROM). Acta Obstet Gynecol Scand 1987;66:437–9. membranes. Br J Obstet Gynecol 2005;112:754–8.
56. Gaucherand P, Guibaud S, Rudigoz RC, Wong A. Diagnosis of premature 69. Gurbuz A, Karateke A, Kabaca C. Vaginal fluid creatinine in premature
rupture of the membranes by the identification of alpha-feto-protein in rupture of membranes. Int J Gynaecol Obstet 2004;85:270–1.
vaginal secretions. Acta Obstet Gynecol Scand 1994;73:456–9.
70. Kafali H, Oksuzler. Vaginal fluid urea and creatinine in diagnosis of
57. Kishida T, Yamada H, Negishi H, Sagawa T, Makinoda S, Fujimoto S. premature rupture of membranes. Arch Gynecol Obstet 2007;275:157–60.
Diagnosis of preterm rupture of the membranes using a newly developed 71. Lockwood CJ, Wein, R, Chien D, Ghidini A, Alvarez M, Berkowitz RL.
AFP monoclonal antibody test kit. Eur J Obstet Gynecol Reprod Biol Fetal membrane rupture is associated with the presence of insulin-like
1995;58:67–72. growth factor-binding protein-1 in vaginal secretions. Am J Obstet Gynecol
1994;171:146–50.
58. Gaucherand P. Guibaus S, Awada A, Rudigoz RC. Comparative study
of three amniotic fluid markers in premature rupture of membranes: 72. Rutanen EM, Karkkainen TH, Lehtovirta J, Uotila JT, Hinkula MK,
fetal fibronectin, alpha-fetoprotein, diamino-oxydase. Acta Obstet Hartikainem AL. Evaluation of a rapid strip test for insulin-like growth
Gynecol Scand 1995;74:118–21. factor binding protein-1 in the diagnosis of ruptured fetal membranes.
Clinic Chimica Acta 1996;253:91–101.
59. Kishida T, Yamada H, Negishi H, Sagawa T, Makinoda S, Fujimoto S.
73. Darj E, Lyrenas S. Insulin-like growth factor binding protein-1, a quick
Diagnosis of premature rupture of the membranes in preterm patients,
way to detect amniotic fluid. Acta Obstet Gynecol Scand 1998;77:295–7.
using an improved AFP kit: comparison with ROM-check and/or nitrazine
test. Eur J Obstet Gynecol Reprod Biol 1996;69:77–82. 74. Jeurgens-Borst AJCM, Bekkers RLM, Sporken JMJ, van den Berg PP.
Use of insulin like growth factor binding protein-1 in the diagnosis of
60. Kim YH, Park YW, Kwon HS, Kwon JA, Kim BJ. Vaginal fluid b-human ruptured fetal membranes. Eur J Obstet Gynecol Reprod Biol
chorionic gonadotropin level in the diagnosis of premature rupture of 2002;102:11–4.
membranes. Acta Obstet Gynecol Scand 2005;84:802–5.
75. Petrunin DD, Griaznova IM, Petrunina IuA, Tatarinov IuS.
61. Anai T, Tanaka Y, Hirota Y, Miyakawa I.Vaginal fluid hCG levels for Immunochemical identification of organ specific human placental
detecting premature rupture of membranes. Obstet Gynecol 1997;89:261–4. alpha-microglubulin and its concentration in amniotic fluid [article in
Russian]. Akush Ginekol (Mosk) 1977;1:64–5.
62. Esim, E, Turan C, Unal O, Dansuk R, Cengizglu B. Diagnosis of premature
76. Cousins LM, Smok D, Lovett SM, Poeltler DM. AmniSure placental alpha
rupture of membranes by identification of b-HCG in vaginal washing fluid.
microglobulin-1 rapid immunoassay versus standard diagnostic methods
Eur J Obstet Gynecol Reprod Biol 2003;107:37–40.
for detection of rupture of membranes. Am J Perinatol 2005;22:1–4.
63. Hellemans P, Verdonk P, Baekelandt M, Joostens M, Franx M. Gerris J. 77. Lee SE, Park JS, Norwitz ER, Kim KW, Park HS, Jun JK. Measurement
Preliminary results with the use of the ROM-check immunoassay in the of placental alpha-microglobulin-1 in cervicovaginal discharge to diagnosis
early detection of rupture of the amniotic membranes. Eur J Obstet rupture of membranes. Obstet Gynecol 2007;109:634–40.
Gynecol Reprod Biol 1992;43:173–9.
78. Mulhair L, Carter J, Poston L, Seed P, Briley A. Prospective cohort study
64. Eriksen NL, Parisi VM, Daoust S, Flamm B, Garite TJ, Cox SM. Fetal investigating the reliability of the AmnioSens method for detection of
fibronectin: a method for detecting the presence of amniotic fluid. spontaneous rupture of membranes. BJOG 2009;116:313–8.
Obstet Gynecol 1992;80:451–4. 79. Cowett RM, Hakanson DO, Kocon RW, Oh W. Untoward neonatal effect
of intraamniotic administration of methylene blue. Obstet Gynecol
65. Rutanen EM, Pekonen F, Karkkainen T. Measurement of insulin-like
1976;48(Suppl):74s-75s.
growth factor binding protein-1 in cervical/vaginal secretions: comparison
with the ROM-check Membrane Immunoassay in the diagnosis of ruptured 80. Plunkett GD. Neonatal complications [letter to the editor]. Obstet Gynecol
fetal membranes. Clinic Chimica Acta 1993;214:73–81. 1973;41:476–7.
JUNE JOGC JUIN 2010 l 569
Vous aimerez peut-être aussi
- Noninvasive Prenatal Testing (NIPT): Applied Genomics in Prenatal Screening and DiagnosisD'EverandNoninvasive Prenatal Testing (NIPT): Applied Genomics in Prenatal Screening and DiagnosisLieve Page-ChristiaensPas encore d'évaluation
- Frozen Section Pathology: Diagnostic ChallengesD'EverandFrozen Section Pathology: Diagnostic ChallengesAlain C. BorczukPas encore d'évaluation
- Lower Genital Tract Precancer: Colposcopy, Pathology and TreatmentD'EverandLower Genital Tract Precancer: Colposcopy, Pathology and TreatmentPas encore d'évaluation
- Practical Gynecologic Pathology: Frequently Asked QuestionsD'EverandPractical Gynecologic Pathology: Frequently Asked QuestionsJian-Jun WeiPas encore d'évaluation
- Diagnosis of Endometrial Biopsies and Curettings: A Practical ApproachD'EverandDiagnosis of Endometrial Biopsies and Curettings: A Practical ApproachPas encore d'évaluation
- The Placenta and Neurodisability 2nd EditionD'EverandThe Placenta and Neurodisability 2nd EditionIan CrockerPas encore d'évaluation
- Fetal-Placental DisordersD'EverandFetal-Placental DisordersNicholas S. AssaliÉvaluation : 5 sur 5 étoiles5/5 (1)
- Pheochromocytomas, Paragangliomas and Disorders of the Sympathoadrenal System: Clinical Features, Diagnosis and ManagementD'EverandPheochromocytomas, Paragangliomas and Disorders of the Sympathoadrenal System: Clinical Features, Diagnosis and ManagementLewis LandsbergPas encore d'évaluation
- Adrenal Disorders: Physiology, Pathophysiology and TreatmentD'EverandAdrenal Disorders: Physiology, Pathophysiology and TreatmentAlice C. LevinePas encore d'évaluation
- Gap Junction Structure and Chemical Regulation: Direct Calmodulin Role in Cell-to-Cell Channel GatingD'EverandGap Junction Structure and Chemical Regulation: Direct Calmodulin Role in Cell-to-Cell Channel GatingÉvaluation : 3 sur 5 étoiles3/5 (1)
- Translational Research in Breast CancerD'EverandTranslational Research in Breast CancerDong-Young NohPas encore d'évaluation
- Pregnancy Tests Explained (2Nd Edition): Current Trends of Antenatal TestsD'EverandPregnancy Tests Explained (2Nd Edition): Current Trends of Antenatal TestsPas encore d'évaluation
- Endometrial Gene Expression: An Emerging Paradigm for Reproductive DisordersD'EverandEndometrial Gene Expression: An Emerging Paradigm for Reproductive DisordersJoanne Kwak-KimPas encore d'évaluation
- Fast Facts: Myelofibrosis: Reviewed by Professor Ruben A. MesaD'EverandFast Facts: Myelofibrosis: Reviewed by Professor Ruben A. MesaPas encore d'évaluation
- Clinical Ophthalmic Oncology: RetinoblastomaD'EverandClinical Ophthalmic Oncology: RetinoblastomaJesse L. BerryPas encore d'évaluation
- Neuroendocrine Disorders in ChildrenD'EverandNeuroendocrine Disorders in ChildrenMehul DattaniPas encore d'évaluation
- Practical Cytopathology: Frequently Asked QuestionsD'EverandPractical Cytopathology: Frequently Asked QuestionsHuihong XuPas encore d'évaluation
- Human Stem Cell Manual: A Laboratory GuideD'EverandHuman Stem Cell Manual: A Laboratory GuideSuzanne PetersonPas encore d'évaluation
- Complications of CSF Shunting in Hydrocephalus: Prevention, Identification, and ManagementD'EverandComplications of CSF Shunting in Hydrocephalus: Prevention, Identification, and ManagementPas encore d'évaluation
- Guide to Pediatric Urology and Surgery in Clinical PracticeD'EverandGuide to Pediatric Urology and Surgery in Clinical PracticePas encore d'évaluation
- Chronopharmaceutics: Science and Technology for Biological Rhythm Guided Therapy and Prevention of DiseasesD'EverandChronopharmaceutics: Science and Technology for Biological Rhythm Guided Therapy and Prevention of DiseasesBi-Botti C. YouanPas encore d'évaluation
- Cerebrospinal Fluid in Clinical NeurologyD'EverandCerebrospinal Fluid in Clinical NeurologyFlorian DeisenhammerPas encore d'évaluation
- Follicular Lymphoma: Current Management and Novel ApproachesD'EverandFollicular Lymphoma: Current Management and Novel ApproachesNathan H. FowlerPas encore d'évaluation
- Diagnosis and Management of Cholangiocarcinoma: A Multidisciplinary ApproachD'EverandDiagnosis and Management of Cholangiocarcinoma: A Multidisciplinary ApproachJames H. TabibianPas encore d'évaluation
- Practical Pediatric Urology: An Evidence-Based ApproachD'EverandPractical Pediatric Urology: An Evidence-Based ApproachPrasad GodbolePas encore d'évaluation
- Glandular Lesions of the Uterine Cervix: Cytopathology with Histologic CorrelatesD'EverandGlandular Lesions of the Uterine Cervix: Cytopathology with Histologic CorrelatesPas encore d'évaluation
- Peptide and Protein DeliveryD'EverandPeptide and Protein DeliveryChris Van Der WalleÉvaluation : 2 sur 5 étoiles2/5 (1)
- Hormones and Embryonic Development: Advances in the BiosciencesD'EverandHormones and Embryonic Development: Advances in the BiosciencesG. RaspéPas encore d'évaluation
- Human Afflictions and Chromosomal Aberrations: International Series of Monographs in Pure and Applied Biology: Modern Trends in Physiological SciencesD'EverandHuman Afflictions and Chromosomal Aberrations: International Series of Monographs in Pure and Applied Biology: Modern Trends in Physiological SciencesPas encore d'évaluation
- Receptors of Cell Adhesion and Cellular RecognitionD'EverandReceptors of Cell Adhesion and Cellular RecognitionPas encore d'évaluation
- Neurodevelopmental Disorders: Comprehensive Developmental NeuroscienceD'EverandNeurodevelopmental Disorders: Comprehensive Developmental NeurosciencePas encore d'évaluation
- Clinical Precision Medicine: A PrimerD'EverandClinical Precision Medicine: A PrimerJudy S. CrabtreePas encore d'évaluation
- Diseases of the Liver and Biliary TreeD'EverandDiseases of the Liver and Biliary TreeAnnarosa FloreaniPas encore d'évaluation
- Cancer Treatment and the Ovary: Clinical and Laboratory Analysis of Ovarian ToxicityD'EverandCancer Treatment and the Ovary: Clinical and Laboratory Analysis of Ovarian ToxicityPas encore d'évaluation
- Active Surveillance for Localized Prostate Cancer: A New Paradigm for Clinical ManagementD'EverandActive Surveillance for Localized Prostate Cancer: A New Paradigm for Clinical ManagementPas encore d'évaluation
- Neuroendocrine Tumors: Surgical Evaluation and ManagementD'EverandNeuroendocrine Tumors: Surgical Evaluation and ManagementJordan M. CloydPas encore d'évaluation
- French 2lp15 1trim1Document2 pagesFrench 2lp15 1trim1Mamoun BelkacemPas encore d'évaluation
- BacillusDocument38 pagesBacillusHanaa ZianiPas encore d'évaluation
- DiabetesDocument32 pagesDiabetesAlif AbqoPas encore d'évaluation
- Anses Ra2022Document38 pagesAnses Ra2022Fabrice De OliveiraPas encore d'évaluation
- Dénombrement Et IdentificationDocument98 pagesDénombrement Et Identificationbenali anfalPas encore d'évaluation
- Les Agents AntimicrobiensDocument33 pagesLes Agents AntimicrobiensKenz L'AïdPas encore d'évaluation
- Fiche Pratique 2 Principaux Types de Syndromes DiarrheiquesDocument1 pageFiche Pratique 2 Principaux Types de Syndromes DiarrheiquesFrançois NiemePas encore d'évaluation
- Immu SpecifiqueDocument9 pagesImmu SpecifiqueDalili SVTPas encore d'évaluation
- 1201 FCD Criteres Microbiologiques 2016 Produits Ls MP 28012016Document59 pages1201 FCD Criteres Microbiologiques 2016 Produits Ls MP 28012016Olfa Ben MoussaPas encore d'évaluation
- Les Armes Biologiques ModernesDocument26 pagesLes Armes Biologiques ModernesIrish Coffee BoyPas encore d'évaluation
- La Reconnaissance Du Soi Et Du Non SoiDocument6 pagesLa Reconnaissance Du Soi Et Du Non SoiRonan PerennesPas encore d'évaluation
- QCMDocument13 pagesQCMNassim OuabouPas encore d'évaluation
- Le DR Stefan Lanka Expose La Fraude ViraleDocument5 pagesLe DR Stefan Lanka Expose La Fraude ViraleMika DeverinPas encore d'évaluation
- Fiche 04 Ac AntinucleaireDocument7 pagesFiche 04 Ac AntinucleaireNabil BahouraPas encore d'évaluation
- ATB Bucco Dentaire Argumentaire V3Document75 pagesATB Bucco Dentaire Argumentaire V3Jean Philippe TranPas encore d'évaluation
- 2 10 s1 Hygiene Hospitaliere Version CRDocument32 pages2 10 s1 Hygiene Hospitaliere Version CRkoummanePas encore d'évaluation
- TP 121Document14 pagesTP 121alan muzanPas encore d'évaluation
- Cours de Genétique Humaine-1 - 2014Document88 pagesCours de Genétique Humaine-1 - 2014Soussou SouadPas encore d'évaluation
- Les ECN en 51 Dossiers Transversaux - Tome 1Document276 pagesLes ECN en 51 Dossiers Transversaux - Tome 1Saruzayo Hagiis100% (1)
- Vaccinations - Les Vérités Indésirables - (PDF OCR) (PDFDrive)Document601 pagesVaccinations - Les Vérités Indésirables - (PDF OCR) (PDFDrive)Technique Incomplete100% (2)
- HémophilieDocument4 pagesHémophiliedaynoPas encore d'évaluation
- Helicobacter Pylori Caractères Bactériologiques, Méthodes Diagnostiques Et Sensibilité Aux AntibiotiquesDocument6 pagesHelicobacter Pylori Caractères Bactériologiques, Méthodes Diagnostiques Et Sensibilité Aux AntibiotiquesAhmed BelhadriPas encore d'évaluation
- MMV Notions de BaseDocument10 pagesMMV Notions de BaseProfessor LatePas encore d'évaluation
- Jim Humble II MMS en Afrique Traiter Le VIH Et Le Cancer Jan 2010Document8 pagesJim Humble II MMS en Afrique Traiter Le VIH Et Le Cancer Jan 2010tarpan9Pas encore d'évaluation
- Vaccination QUESTIONSDocument10 pagesVaccination QUESTIONSSoukainaPas encore d'évaluation
- Pasteur L'imposteurDocument10 pagesPasteur L'imposteurGuillaume ParisotPas encore d'évaluation
- Virologie GeneraleDocument147 pagesVirologie GeneraleDuhoranenayo DieudonnePas encore d'évaluation
- Faster LaminarairflowDocument29 pagesFaster LaminarairflowjosebolisPas encore d'évaluation
- Prevalence de La Syphilis Chez Les Demandeurs de La Serologie Syphilitique Au Laboratoire Du CHU TlemcenDocument98 pagesPrevalence de La Syphilis Chez Les Demandeurs de La Serologie Syphilitique Au Laboratoire Du CHU Tlemcenservice informatiquePas encore d'évaluation
- 4SV31DVWB0023D06 DevoirSVT-U06Document5 pages4SV31DVWB0023D06 DevoirSVT-U06sarah.neptuneeePas encore d'évaluation