Académique Documents
Professionnel Documents
Culture Documents
(Wells, 2008) Suprapubic or Urethral Catheter What Is The Optimal Method of Bladder Drainage After Radical Hysterectomy
Transféré par
dadupipaTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
(Wells, 2008) Suprapubic or Urethral Catheter What Is The Optimal Method of Bladder Drainage After Radical Hysterectomy
Transféré par
dadupipaDroits d'auteur :
Formats disponibles
GYNAECOLOGY
GYNAECOLOGY
Suprapubic or Urethral Catheter:
What Is the Optimal Method of Bladder
Drainage After Radical Hysterectomy?
Tiffany H. Wells, MD, FRCSC,1 Helen Steed, MD, FRCSC,1,2 Valerie Capstick, MD, FRCSC,1,2
Alexandra Schepanksy, MD, FRCSC,1,2 Michelle Hiltz, MSc,1 Wylam Faught, MD, FRCSC1,2
1
University of Alberta, Department of Obstetrics and Gynecology, Edmonton AB
2
Department of Gynecologic Oncology, Cross Cancer Institute, Edmonton AB
Abstract été utilisé pour la vidange postopératoire de la vessie à la suite
d’une HAR, le cathétérisme suspubien (CSP) constitue une
Background: Lower urinary tract dysfunction is a common morbidity méthode de rechange pouvant être avantageuse.
related to radical hysterectomy (RAH). Although transurethral
catheterization (TUC) has traditionally been used for postoperative Objectifs : Déterminer, au moyen d’une étude de cohorte
bladder drainage following RAH, suprapubic catheterization (SPC) rétrospective, l’incidence de l’infection des voies urinaires (IVU), la
is an alternative method that may be advantageous. durée de l’hospitalisation postopératoire et le délai avant l’essai de
miction chez les femmes ayant fait l’objet d’un cathétérisme
Objectives: To determine, by means of a retrospective cohort study,
suspubien ou transurétral à la suite d’une HAR motivée par un
the incidence of urinary tract infection (UTI), duration of
cancer du col utérin de stade précoce.
postoperative hospital stay, and time to trial of voiding in women
catheterized suprapubically or transurethrally after RAH for early Méthodes : Deux cent douze patientes ayant subi une HAR et une
stage cervical cancer. stadification, en présence de cancers du col utérin de stades
Methods: Two hundred twelve patients who underwent RAH and IA1 + LVS, 1A2 et 1B1 à Edmonton entre 1996 et 2006, ont
staging for stage IA1 + LVS, 1A2, and 1B1 cancer of the cervix in participé à l’étude. Trois gynécologues-oncologues ont effectué
Edmonton between 1996 and 2006 were included in the study. les chirurgies en question. Des données opératoires,
Three gynaecologic oncologists performed the surgeries. postopératoires et démographiques ont été tirées des dossiers de
Operative, postoperative, and demographic data were extracted ces patientes. Les patientes ont fait l’objet d’un cathétérisme
from patient records. Patients were catheterized either suspubien (groupe CSP) ou transurétral (groupe CTU), à la
suprapubically (SPC group) or transurethrally (TUC group) discrétion du chirurgien. Des essais comparatifs et une analyse de
according to the surgeon’s discretion. Comparative tests and régression multivariée ont été utilisés pour comparer certains
multivariate regression analysis were used to compare outcome critères d’évaluation entre les groupes et pour neutraliser l’effet
measures between the groups and to adjust for confounding des variables confusionnelles.
variables. Résultats : Le groupe CTU comptait une proportion de patientes
Results: The TUC group had a higher proportion of patients with UTI présentant une IVU (27 %) plus élevée que celle que comptait le
(27%) than the SPC group (6%) (P < 0.001). The SPC group had groupe CSP (6 %) (P < 0,001). Les participantes du groupe CSP
a shorter postoperative hospital stay (4.8 vs. 5.7 days; P < 0.001) ont connu une hospitalisation postopératoire plus courte
and an earlier trial of voiding (2.7 vs. 4.4 days; P < 0. 001). (4,8 jours, par comparaison avec 5,7 jours; P < 0,001) et un essai
Following regression analysis, statistically significant differences de miction plus précoce (2,7 jours, par comparaison avec
remained for UTI and time to initiation of a trial of voiding. 4,4 jours; P < 0,001). À la suite de l’analyse de régression, nous
constations toujours des différences significatives sur le plan
Conclusion: After RAH for early stage cervical cancer, suprapubic
statistique en matière d’IVU et de délai avant la mise en œuvre
catheterization is associated with a lower rate of UTI and an
d’un essai de miction.
earlier trial of voiding than transurethral catheterization.
Conclusion : À la suite d’une HAR motivée par un cancer du col
Résumé utérin de stade précoce, le cathétérisme suspubien est associé à
un taux moindre d’IVU et à la tenue plus précoce d’un essai de
Contexte : Le dysfonctionnement des voies urinaires basses est une miction, par comparaison avec le cathétérisme transurétral.
morbidité courante associée à l’hystérectomie radicale (HAR).
J Obstet Gynaecol Can 2008;30(11):1034–1038
Bien que le cathétérisme transurétral (CTU) ait traditionnellement
INTRODUCTION
Key Words: Radical hysterectomy, suprapubic catheter, urinary
tract infection, urinary bladder urgery is commonly used in treatment for women with
Competing Interests: None declared. S early cervical cancer (stages IA and IB1) who have mini-
Received on August 27, 2007 mal medical comorbidity. Urinary dysfunction is the most
Accepted on February 4, 2008 common morbidity related to radical hysterectomy,
1034 l NOVEMBER JOGC NOVEMBRE 2008
Suprapubic or Urethral Catheter: What Is the Optimal Method of Bladder Drainage After Radical Hysterectomy?
occurring postoperatively in approximately 30% of RAH All patients were administered antibiotics preoperatively
patients.1–3 The majority of these women will experience and were catheterized intraoperatively, either
acute neurogenic bladder dysfunction during the postoper- transurethrally (using a Foley catheter with 16 French
ative period, with difficulty in voiding, high post-void resid- gauge, 5.3 mm diameter) or suprapubically (using a
ual volumes, and changes in bladder compliance. Perivesical Bonanno catheter with 14 British gauge, 2.1 mm diameter).
edema, hematoma, fibrosis, and autonomic denervation of Exclusion criteria for the study were an incomplete medical
the bladder may contribute to this postoperative urinary chart, incorrect surgical coding, intraoperative cystotomy or
dysfunction after RAH, but the pathophysiology of postop- ureteric injury, RAH at the time of Caesarean section, RAH
with PLN for malignancy other than cervical, and a past
erative urinary dysfunction remains incompletely under-
history of pelvic radiotherapy.
stood.4,5 Despite the frequency of occurrence of urinary
dysfunction following RAH, no consensus exists on its Demographic data including patient age, parity, history of
appropriate management in the postoperative period. CS, and stage of disease were obtained from health records.
Transurethral catheterization has traditionally been used to Maximum tumour dimension and tumour histology were
facilitate postoperative bladder drainage following RAH, retrieved from surgical pathology reports. Operative data,
but suprapubic catheterization is an alternative method that including surgeon’s name, operating time, and estimated
may have distinct advantages. Possible benefits of SPC over blood loss, were recorded from operative records. Our out-
TUC include earlier spontaneous voiding, improved facili- comes of interest (the incidence of UTI, LOHS, and time to
TOV) were extracted from the medical records.
tation of voiding trials, improved patient comfort,
decreased incidence of urinary tract infection, earlier ambu- Patients were assigned to one of two groups on the basis of
lation, and shorter duration of hospital stay.6,7 the method of catheterization used at the time of surgery.
We hypothesized that SPC after RAH and pelvic The method of catheterization was determined solely by the
lymphadenectomy for early stage cervical cancer is associ- surgeon’s preference. Demographic data and operative data
ated with a decreased incidence of UTI, a shorter length of were compared between groups to determine whether the
hospital stay and an earlier postoperative trial of voiding two groups differed significantly other than in mode of
when compared with TUC. catheterization. Outcomes of interest, including incidence
of UTI, LOHS, and time to TOV, were compared between
MATERIALS AND METHODS the two groups. A UTI was documented if a patient had
dysuria and a positive urine dipstick test (for leucocytes and
We performed a retrospective cohort study using the nitrites), a urine culture with >105 CFU/mL, microscopy
records of women with stage IA1 + LVSI, 1A2, and IB1
with ³ 5 leukocytes/high power field, or if a patient was
cervical cancer who had RAH and PLN performed in
treated for a UTI. All UTIs between the time of surgery and
Edmonton, Alberta, between January 1996 and March
the six-week follow-up visit were recorded. Universal
2006. In all cases, a type II RAH and PLN was performed
screening for UTIs in the postoperative period is not per-
by one of three gynaecologic oncologists, assisted by gynae-
formed in our institution; only patients with symptoms
cology residents. Each type II RAH included resection of
were investigated. LOHS was the total number of days
the cervicovesical fascia, the proximal uterosacral and
from admission to discharge. Time to initiation of trial of
rectovaginal ligaments, a portion of the upper vagina, and
voiding was defined as the number of days from insertion
the medial half of the parametria and cardinal ligaments.
of catheter to first voiding attempt (discontinuation of TUC
or clamping of SPC). The actual timing of TOV was deter-
ABBREVIATIONS mined by the individual surgeon. Transurethral catheters
were removed as early as the second postoperative day or as
CFU colony forming unit
late as the seventh postoperative day. Suprapubic catheters
CS Caesarean section were commonly clamped to begin TOV on the second
EBL estimated blood loss postoperative day, but in some cases were clamped later.
LOHS length of hospital stay
PLN pelvic lymphadenectomy
The chi-square test, Cochran-Mantel-Haenszel’s row mean
RAH radical hysterectomy
score statistic, and Wilcoxon rank-sum test (non-
parametric) were used for analysis of categorical parame-
SPC suprapubic catheterization
ters, ordinal response variables, and continuous measures,
TOV trial of voiding
respectively. Statistical significance was set at P < 0.05 for
TUC transurethral catheterization
all tests. Regression analysis was performed to adjust for
UTI urinary tract infection
confounding variables that were estimated to have the most
NOVEMBER JOGC NOVEMBRE 2008 l 1035
GYNAECOLOGY
Table 1. Patient characteristics
TUC (n = 134) SPC (n = 78) P
Median age, years (range) 40.00 (20–78) 40.50 (21–78) 0.939
Median parity (range) 2.00 (0–9) 2.00 (0–7) 0.817
Previous CS, % (n) 15.9 (21) 6.4 (5) 0.043
FIGO Stage, % (n)
IA 46.3 (62) 42.3 (33) 0.576
IB 53.7 (72) 57.7 (45)
Median tumour size, mm (range) 3.0 (0–60) 5.0 (0–60) 0.382
Histology, % (n)
Squamous 51.5 (69) 44.9 (35) 0.455
Adeno 29.8 (40) 29.5 (23)
Other 18.7 (25) 25.6 (20)
Table 2. Operative information
TUC (n = 134) SPC (n = 78) P
Surgeon
A 46% (62) 0% (0) < 0.001
B 37% (49) 100% (78)
C 17% (23) 0% (0)
Median operative time, minutes (range) 187 (89–318) 169 (105–295) 0.016
Median estimated blood loss, mL (range) 600 (200–6000) 500 (200–2300) 0.094
effect on each outcome of interest. Adjusted odds ratios proportion of patients in the TUC group had undergone
were calculated for binary responses using logistic regres- previous CS than in the SPC group (15.9% vs. 6.41%; P =
sion analysis. All statistical analyses were performed using 0.043) (Table 1). Significantly more patients in the SPC
SAS Version 9.1 (SAS Institute Inc., Cary NC). group than in the TUC group had surgery performed by
surgeon B. Initially, all three surgeons used TUC only; in
Ethics approval for the study was obtained from the
2000, surgeon B switched to use of SPC exclusively. The
Research Ethics Board of the Cross Cancer Institute and
SPC group was associated with a shorter operative time
the University of Alberta.
than the TUC group (median = 169 vs. 187 minutes; P =
0.016). There was no significant difference in EBL between
RESULTS
groups (Table 2).
Of 264 patients identified through surgical coding logs, 212
met the inclusion criteria. Of the excluded patients, 24 had A significantly higher proportion of patients in the TUC
malignant pathology other than cervical, 12 had a procedure group developed UTI than in the SPC group (27% vs. 6%;
other than RAH with PLN, five had preoperative radiother- P = 0.003). The median LOHS was significantly shorter in
apy, four had medical records that could not be located, the SPC group than in the TUC group (4 days vs. 6 days; P <
three had cancer staging > IB1, two had RAH at the time of 0.001), and median time to initiation of TOV was also
CS, and two had intraoperative cystotomy. shorter in the SPC group (3 days vs. 4 days; P < 0.001)
(Table 3).
There were 134 patients in the TUC group and 78 patients
in the SPC group. Baseline characteristics, including age, Multivariate regression analysis was used to adjust for con-
parity, stage of disease, maximum tumour dimension, and founding variables. After correcting for surgeon, operative
histology did not differ between groups. In each group, time, and tumour size through multivariate analysis, the
patients with tumour diameters greater than 4.0 cm had relationship between the occurrence of UTI and the type of
been clinically staged as IB1, only to be found to have larger catheter used remained statistically significant (OR 0.12;
tumours at the time of pathology examination. A greater 95% CI 0.039 to 0.369, P = 0.002). If a patient was
1036 l NOVEMBER JOGC NOVEMBRE 2008
Suprapubic or Urethral Catheter: What Is the Optimal Method of Bladder Drainage After Radical Hysterectomy?
Table 3. Outcomes by method of catheterization
TUC (n = 134) SPC (n = 78) P
Urinary tract infection (n) 27% (36) 6% (5) 0.003
Median length of hospital stay, days (range) 6 (3–16) 4 (3–12) < 0.001
Median time to trial of voiding, days (range) 4 (2–7) 3 (2–5) < 0.001
catheterized transurethrally, the risk of developing a UTI incidence of UTI in the TUC group was significantly higher
was eight times greater than if the patient was catheterized than in the SPC group (35% vs. 6%; P < 0.001). This is
suprapubically. The difference in time to initiation of TOV important to note, because analyzing the outcomes for only
between the two study groups remained statistically signifi- one surgeon’s patients, although limiting generalizability,
cant (P < 0.001) after adjusting for surgeon, parity, tumour controls for the unmeasured surgical and postoperative
size, and previous CS. Operative date was chosen as a con- differences in care between physicians.
founder for LOHS because in 2000 the surgeons at our
institution began earlier postoperative feeding, resulting in The outcomes and variables we were able to study are lim-
earlier hospital discharge and shorter LOHS. After adjust- ited by the retrospective data collection. Despite this meth-
ing for surgeon, whether or not surgery was done before or odology, we were able to document any UTI up to six weeks
after 2000, and tumour size, the median LOHS was not after RAH and PLN, and conclude that any UTI detected
significantly different between the groups. after this point was not catheter-associated. LOHS,
although easily measured, is dependent on multiple vari-
DISCUSSION ables that cannot easily be controlled in retrospective
reviews. We were not able to show a difference in LOHS
This retrospective study assessed whether the method of
between groups when all patients were analyzed. However,
catheterization used postoperatively affected the incidence
in surgeon B’s patients, LOHS was significantly shorter in
of UTI, time to trial of voiding, and length of hospital stay.
the SPC group than in the TUC group, suggesting that the
Although a retrospective design may result in selection bias,
surgeon may not be the most important factor in determin-
most patient demographic and operative variables were
ing patients’ LOHS. Time to TOV is undeniably linked to
similar in the women catheterized suprapubically and those
method of catheterization because surgeons are more likely
catheterized transurethrally. We acknowledge, however,
to start an early trial of voiding in patients with an SPC. The
that significantly more women in the TUC group than
success of first TOV would be a more useful parameter to
women in the SPC group had a previous CS. It is plausible
compare between groups, but this was not consistently
that this difference and the resulting difficulty of bladder
recorded. A prospective study design would allow for more
dissection may have influenced the type of catheter chosen
outcomes to be evaluated and compared over a greater
by the surgeon or the timing of a postoperative voiding trial.
length of time. Valuable outcomes that could not be
Furthermore, a longer operative time may indicate that the
extracted retrospectively, such as patient satisfaction,
procedure was more difficult or involved a larger tumour,
mechanical difficulties with SPC, complications secondary
and these variables may also have influenced a surgeon in
to SPC insertion, likelihood of successful TOV with each
the choice of catheter. However, after regression analysis
method of catheterization, total duration of catheterization,
that adjusted for surgeon, operative time, and tumour size,
and long-term voiding dysfunction, would be important to
the difference between groups in the incidence of UTI and
include in a prospective study design.
time to TOV remained significant.
In this study only one surgeon (surgeon B) used SPC. This Although the benefits of SPC use have been demonstrated
surgeon initially used TUC only, but after learning of the in urogynaecology and general surgery patients,6–13 only
utility of SPC in urogynaecology procedures changed to the three studies evaluating the use of SPC after RAH and PLN
exclusive use of SPC. Despite regression analysis that con- have been published. Naik et al. reported a higher incidence
trols for surgeon, it is difficult to determine if the differ- of UTI on the third postoperative day in patients who were
ences in outcomes were related to the surgeon involved or performing intermittent self-catheterization than in patients
the mode of catheterization. To better control for this con- with SPC (42% and 18%, respectively),14 and van Nagell et
founder, we analyzed patients of surgeon B only. Surgeon al. described a 44% rate of UTI in patients with TUC com-
B’s patients with TUC had a significantly longer postopera- pared with 23% in patients with SPC.15 A small study (N =
tive stay than patients with SPC ( P < 0.001) and the 24) reported by Nwabineli et al. found no difference in the
NOVEMBER JOGC NOVEMBRE 2008 l 1037
GYNAECOLOGY
incidence of UTI after RAH and PLN between women 5. Jackson KS, Naik R. Pelvic floor dysfunction and radical hysterectomy. Int
J Gynecol Cancer 2006;16:354–63.
with TUC and with SPC.16 Our findings are consistent with
6. Schiøtz HA, Malme PA, Tanbo TG. Urinary tract infections and
previous reports, and further demonstrate the benefit of asymptomatic bacteriuria after vaginal plastic surgery. A comparison of
using SPC through a reduction in postoperative catheter suprapubic and transurethral catheters. Acta Obstet Gynecol Scand
1989;68(5):453–5.
associated infection. We have demonstrated for the first
time the earlier initiation of a voiding trial associated with 7. Bergman A, Matthews L, Ballard CA, Roy S. Suprapubic versus
transurethral bladder drainage after surgery for stress urinary incontinence.
SPC after RAH and PLN. Obstet Gynecol 1987 Apr;69(4):546–9.
We recognize that a growing proportion of radical hysterec- 8. McPhail MJ, Abu-Hilal M, Johnson CD. A meta-analysis comparing
tomies are being performed laparoscopically, and that RAH suprapubic and transurethral catheterization for bladder drainage after
abdominal surgery. Br J Surg 2006 Sep;93(9):1038–44.
patients are likely to be discharged early from hospital
9. Baan AH, Vermeulen H, van der Meulen J, Bossuyt P, Olszyna D, Gouma
regardless of method of catheterization. However, we sug- DJ. The effect of suprapubic catheterization versus transurethral
gest that the use of SPC rather than TUC in this group catheterization after abdominal surgery on urinary tract infection: a
randomized controlled trial. Dig Surg 2003;20(4):290–5.
would also result in a lower incidence of UTI and an early
TOV after hospital discharge. 10. Andersen JT, Heisterberg L, Hebjørn S, Petersen K, Stampe Sørensen S,
Fischer-Rasmussen W, et al. Suprapubic versus transurethral bladder
drainage after colposuspension/vaginal repair Acta Obstet Gynecol Scand
CONCLUSION 1985;64(2):139–43.
In women who have had radical hysterectomy and pelvic 11. Perrin LC, Penfold C, McLeish A. A prospective randomized controlled trial
lymphadenectomy for early stage cervical cancer, use of a comparing suprapubic with urethral catheterization in rectal surgery. Aust N
suprapubic catheter is associated with a significantly lower Z J Surg 1997 Aug;67(8):554–6.
incidence of UTI and an earlier trial of voiding than use of a 12. Schiøtz HA, Malme PA, Tanbo TG. Urinary tract infections and
asymptomatic bacteriuria after vaginal plastic surgery. A comparison of
transurethral catheter.
suprapubic and transurethral catheters. Acta Obstet Gynecol Scand
1989;68(5):453–5.
REFERENCES
13. Shapiro J, Hoffmann J, Jersky J. A comparison of suprapubic and
1. Naik R, Nwabinelli J, Mayne C, Nordin A, de Barros Lopes A, Monaghan transurethral drainage for postoperative urinary retention in general surgical
JM. Prevalence and management of (non-fistulous) urinary incontinence in
patients. Acta Chir Scand 1982;148(4):323–7.
women following radical hysterectomy for early stage cervical cancer. Eur J
Gynaecol Oncol 2001;22:26–30. 14. Naik R, Maughan K, Nordin A, Lopes A, Godfrey KA, Hatem MH. A
2. Parkin DE. Lower urinary tract complications of the treatment of cervical prospective randomised controlled trial of intermittent self-catheterisation
carcinoma. Obstet Gynecol Surv 1989;44:523–9. vs. suprapubic catheterisation for post-operative bladder care following
3. Bandy LC, Clarke-Pearson DL, Soper JT, Mutch DG, MacMillan J, radical hysterectomy. Gynecol Oncol 2005; 99:437–42.
Creasman WT. Long-term effects on bladder function following radical 15. van Nagell JR, Penny RM, Roddick JW. Suprapubic bladder drainage
hysterectomy with and without postoperative radiation. Gynecol Oncol
following radical hysterectomy. Am J Obstet Gynecol 1972;113(6):849–50.
1987;26:160–8.
4. Kindermann G, Deus-Thiede G. Postoperative urological complications 16. Nwabineli NJ, Walsh DJ, Davis JA. Urinary drainage following radical
after radical hysterectomy for cervical cancer. Baillieres Clin Obstet hysterectomy for cervical carcinoma—a pilot comparison of urethral and
Gynaecol 1988;2:933–41. suprapubic routes. Int J Gynecol Cancer 1993;3:208–10.
1038 l NOVEMBER JOGC NOVEMBRE 2008
Vous aimerez peut-être aussi
- Année Prépa Electricité, Deuxième PartieDocument221 pagesAnnée Prépa Electricité, Deuxième PartieAbdelkader Faklani DouPas encore d'évaluation
- Geometrie Pour Dao2 PDFDocument161 pagesGeometrie Pour Dao2 PDFlekouf43100% (1)
- ANNONCES ASSISTANTS MATERNELS-Disponibilités Secteur Lyautey Du 12 Juin 2020Document3 pagesANNONCES ASSISTANTS MATERNELS-Disponibilités Secteur Lyautey Du 12 Juin 2020younes amaraPas encore d'évaluation
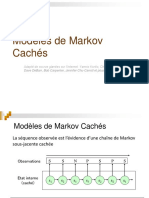
- 3 - Modeles de Markov CachesDocument34 pages3 - Modeles de Markov CachesWISSALPas encore d'évaluation
- GISEMENTDocument4 pagesGISEMENTTouré AbdoulPas encore d'évaluation
- TP 1Document1 pageTP 1djennati100% (1)
- Unite 71 Manuel OpératoireDocument110 pagesUnite 71 Manuel OpératoireAbdessalem Bougoffa50% (2)
- PdM3 Guide Corrige Vrac Repros C4Document2 pagesPdM3 Guide Corrige Vrac Repros C4Eva BteichPas encore d'évaluation
- TD6 PhysiqueDocument4 pagesTD6 PhysiqueEric DeumoPas encore d'évaluation
- Corrige TD 8 1920 2Document5 pagesCorrige TD 8 1920 2friends diaryPas encore d'évaluation
- Api RestDocument8 pagesApi RestfogoPas encore d'évaluation
- Ajust ExpoDocument4 pagesAjust ExpoMme_Sos100% (1)
- ChapitreDocument8 pagesChapitreAchour IfrekPas encore d'évaluation
- Serco FDocument26 pagesSerco FRV PenrroiPas encore d'évaluation
- CC 1 Analyse Natalia Borbón TorresDocument3 pagesCC 1 Analyse Natalia Borbón TorresNatalia Borbon TorresPas encore d'évaluation
- Cours ExcelDocument80 pagesCours ExcelLahcen Boufouss100% (1)
- NF EN 1431 (Mai 2009)Document19 pagesNF EN 1431 (Mai 2009)Fatima BouhajaPas encore d'évaluation
- Sujet Bac 2023 Guinee Niger MathsDocument5 pagesSujet Bac 2023 Guinee Niger Mathsmr.4chiffrePas encore d'évaluation
- TP Conduction CompletDocument10 pagesTP Conduction Complethamza layachi75% (4)
- TD Regime de Neutre TTDocument4 pagesTD Regime de Neutre TTOlivier FLOHRPas encore d'évaluation
- Cours Lignes de Transmission Séance Adaptation D'impédance 2011 2012Document8 pagesCours Lignes de Transmission Séance Adaptation D'impédance 2011 2012benlamlihPas encore d'évaluation
- Poly JavaDocument176 pagesPoly JavaLeonzoConstantiniPas encore d'évaluation
- FeuilletageDocument25 pagesFeuilletageLē JøkērPas encore d'évaluation
- W - 250 - 275 - 325 - 350 - 400 - 1 K..p..Document28 pagesW - 250 - 275 - 325 - 350 - 400 - 1 K..p..joviadoPas encore d'évaluation
- Howto L3 IntervlanroutingDocument7 pagesHowto L3 IntervlanroutingWilford ToussaintPas encore d'évaluation
- GPM Tle C 3e Edition.Document258 pagesGPM Tle C 3e Edition.Pierrot Jules AMOUSSOU100% (2)
- Exercices Chapitre 3 FractionsDocument3 pagesExercices Chapitre 3 FractionsTony GRACAPas encore d'évaluation
- DS SDM S1 2015 CorrectionDocument2 pagesDS SDM S1 2015 CorrectiondsiscnPas encore d'évaluation
- Algèbre 1 V. Def 2017-2018Document141 pagesAlgèbre 1 V. Def 2017-2018Alexis Rosuel100% (1)
- Rapport Optimisation Sur MatlabDocument13 pagesRapport Optimisation Sur MatlabLino YETONGNONPas encore d'évaluation