Académique Documents
Professionnel Documents
Culture Documents
CPG Cap
Transféré par
Rhodora BenipayoTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
CPG Cap
Transféré par
Rhodora BenipayoDroits d'auteur :
Formats disponibles
In GOD We Trust!
ANGONO MEDICS HOSPITAL CPG-CAP
Rainbow Village No.1, Quezon Avenue, Angono, Rizal Form No. AMH MR-037-2017 Rev.01
Page 10f 2
_________________________________________________________________________________
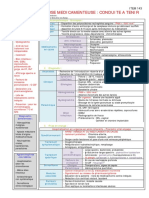
COMMUNITY ACQUIRED PNEUMONIA IN ADULTS
Name of Patient:______________________________ Case No:____________ Date: _______________
Clinical Diagnosis: Diagnostic Tests:
Cough, fever, difficulty of breathing and/or Chest X-ray (as recommended for all patients clinically
chills within the past 24 hours to less than 2 weeks diagnosed of Pneumonia)
associated with tachypnea (RR>20 breaths/ min.) Gram stain and culture of appropriate pulmonary
tachycardia (CR>100/min) and fever (T>37.8`C with at secretions and pre-treatment blood cultures may be
least one abnormal chest finding of diminished breath requested when drug resistance is suspected and for
sounds, ronchi, crackles or wheezes. etiologic diagnosis.
Classify patients by risk categories to help determine the need for hospitalization.
Only moderate and high risk CAP should be admitted.
Clinical Features according to Risk:
Put a check mark on the signs/symptoms noted on the patient for proper classification/ diagnosis.
LOW RISK MODERATE RISK HIGH RISK
Stable Vital Signs: Unstable Vital Signs: Any of the clinical feature of moderate
RR <30 breaths/ min. RR > 30 breaths/ min. risk CAP plus any of the following:
PR <125 beats/min. PR > 125 beats/ min.
SBP > 90 mmHg Temp > 40`C or < 35`C Shock or signs of hypo perfusion
DBP> 60 mmHg
None or stable co-morbid Unstable co morbid condition ____hypotension
conditions such as the ff: ____altered mental state
No evidence of aspiration ____uncontrolled DM ____urine output <30mL/hr.
____active malignancies ____hypoxia (PaO2<60mmHg) or
Chest X-ray: ____progressing neurologic dse. ____acute hypercapnia
Localized infiltrates ____congestive heart failure (CHF) (PaCO2>50mmHg)
No evidence of pleural effusion ___ unstable coronary artery dse.
Not progressive within 24 hrs. ____renal failure on dialysis Chest X-ray:
____uncomp/decomp.COPD
As in moderate risk CAP
Evidence of extra pulmonary
sepsis (hepatic, hematologic,
gastrointestinal, endocrine)
Suspected Aspiration
Chest X-ray:
Multilobar infiltrates
Pleural effusion or abscess
Progression of findings to >50%
in 24 hrs.
These patients are suitable for These patients need to be These patients warrant admission
outpatient care (Grade A)6 hospitalized for parenteral therapy in the intensive care unit (Grade A)6
(Grade A)6
ER Nurse on Duty: Resident on Duty: Attending Physician:
Because here at AMH – the Patient is our No.1 Concern! RMB/2017
TREATMENT: SUPPORTIVE CARE:
Initial empiric therapy based on initial risk Oxygen, hydration and anti-pyretics may be given
stratification is recommended. Among patients if needed
with identified etiologic agent, appropriate
antimicrobials should be instituted. (See
recommended table below)
ANTIBIOTICS DOSAGE ANTIBIOTICS DOSAGE
Low Risk CAP
(all taken orally)
B-lactams: B-lactams w/ B-lactamase
Amoxicillin 500mg TID Inhibitor:
Trim/ sulfonamide: Co-amoxiclav 625mg TID or 1gm BID
Cotrimoxazole 160/800mg BID Sultamicillin 750mg BID
Macrolides: 2nd gen.Caphalosporins:
Azithromycin 500mg OD Cefuroxime Axetil 500mg BID
Clarithromycin 500mg BID
Moderate Risk CAP
Macrolides: 2nd gen, Cephalosporins
Erythromycin IV 0.5-1g q 6h Cefuroxime IV 1.5g q 8h
Azithromycin PO or IV 500mg q 24h Cefoxitin IV (w/anaerobic 1-2g q 8h
Clarithromycin PO or IV 500mg q12h activity)
Gatifloxacin PO or IV 400mg q 24h 3rd gen. Cephalosporins
B-lactams w/ B-lactamase Ceftriaxone IV 1-2g q 24h
inhibitor: Cefotaxime IV 1-2g q 8h
Sulbactam-Ampicillin IV 105g q 8h
High Risk CAP
(all routes are IV)
Macrolides: 3rd gen Cephalosporins:
Erythromicin 0.5-1g q 6h Ceftriaxone 1-2g q 24h
Azithromycin 500mg q 24h Cefotaxime 1-2g q 8h
Clarithromycin 500mg q 12h Ceftizoxime 1-2g q 8h
Gentamicin 3mg/kg q 2h Anti-pseudomonal B-lactams:
Netilmicin 7mg/kg OD Ceftazidime
Tobramycin 3mg/kg q 24h Cefepime 2g q 8h
B-lactams w/ B-lactamase Ticarcillin-clavulanate 2g q 8-12h
inhibitor Piperacillin-tazobactam 3.2g q 6h
Subactam-Ampicillin 1.5g q 6-8h Sulbactam-cefoperazone 2.25-4.5g q 6-8h
Imipenem 1.5g q 12h
Meropenem 500mg q 6h
Others 1-2g q 8h
Oxacillin
Clindamycin 1-2g q4-6h
Metronidazole 600mg q 8h
500mg q 6-8h
Streamlining Empiric Antibiotic Therapy: Hospital Discharge:
In selected patients, switch to oral therapy Patients with stable vital signs for 24 hours and
when signs of infection are resolving within 72 able to maintain oral intake may be discharged.
hrs.
Ward NOD: QA Validation:
Vous aimerez peut-être aussi
- Memoire Fin D'étudeDocument38 pagesMemoire Fin D'étudeJoao Tio MendesPas encore d'évaluation
- Urgences Spécifiques en Oncologie ThoraciqueDocument28 pagesUrgences Spécifiques en Oncologie ThoraciqueLoulou popPas encore d'évaluation
- Cours Infirmier TransplantationDocument20 pagesCours Infirmier Transplantationhela bergaouiPas encore d'évaluation
- Cours Infirmier TransplantationDocument20 pagesCours Infirmier TransplantationibtihelantriPas encore d'évaluation
- NeurologieDocument11 pagesNeurologieمحمد شوقيPas encore d'évaluation
- PALUDISMEDocument22 pagesPALUDISMEAbenekPas encore d'évaluation
- PaludismeDocument40 pagesPaludismeMrTriumphant100% (3)
- 71021protocole de Traitements Covid Dans Les Hopitaux RegionauxDocument7 pages71021protocole de Traitements Covid Dans Les Hopitaux RegionauxStonefalconPas encore d'évaluation
- 05 Drépanocytose Et Grossesse - Protocole GGOLFB 2017Document5 pages05 Drépanocytose Et Grossesse - Protocole GGOLFB 2017Stéphane DonohPas encore d'évaluation
- Cat NeurologieDocument11 pagesCat NeurologieH GooPas encore d'évaluation
- CAT Devant Une TBCDocument3 pagesCAT Devant Une TBCGrace KellyPas encore d'évaluation
- 2015 11 Protocole Parcours de Soins VFDocument12 pages2015 11 Protocole Parcours de Soins VFzouiche KhadidjaPas encore d'évaluation
- Corrigé Des TRAVAUX DIRIGÉS 3 Et 4 Année 2022Document7 pagesCorrigé Des TRAVAUX DIRIGÉS 3 Et 4 Année 2022SOphieSat100% (1)
- Cat Neonat ModifiéDocument75 pagesCat Neonat ModifiéAbdelghani InousPas encore d'évaluation
- OapDocument5 pagesOapLuc TiendrebeogoPas encore d'évaluation
- Traitement Des Exacerbations Aigues Des BPCODocument6 pagesTraitement Des Exacerbations Aigues Des BPCOedhazard1988Pas encore d'évaluation
- Les Conduites À Tenir en InfectieuxDocument43 pagesLes Conduites À Tenir en Infectieuxقريوي مصطفىPas encore d'évaluation
- Protocole Therapeutique Pour La Prise en Charge Ambulatoire Du Covid-19 A L'Ihu Mediterranee Infection 29 JANVIER 2021Document6 pagesProtocole Therapeutique Pour La Prise en Charge Ambulatoire Du Covid-19 A L'Ihu Mediterranee Infection 29 JANVIER 2021no pain no gainPas encore d'évaluation
- Urgences CAT Très PratiqueDocument49 pagesUrgences CAT Très PratiqueAbdelkader Hocini50% (2)
- PEC Gestante Covid 10092021Document11 pagesPEC Gestante Covid 10092021CristinaCaprosPas encore d'évaluation
- Asthme Aigu Grave 2017 PDFDocument46 pagesAsthme Aigu Grave 2017 PDFSerigne Sohibou GayePas encore d'évaluation
- Le Guide Des Anti-InfectieuxDocument97 pagesLe Guide Des Anti-InfectieuxChrist en ellePas encore d'évaluation
- TD12 TransfusionDocument22 pagesTD12 TransfusionAbderrahmenPas encore d'évaluation
- Eclampsie en ReanimationDocument29 pagesEclampsie en ReanimationEbePas encore d'évaluation
- UntitledDocument282 pagesUntitledThe Curious الفضوليPas encore d'évaluation
- Drepanocytose Cas Clinique PediatrieDocument16 pagesDrepanocytose Cas Clinique PediatrieEya EL KAMELPas encore d'évaluation
- Syndrome ThoraciqueDocument3 pagesSyndrome ThoraciqueganlibalamPas encore d'évaluation
- KHH Handbook 2020Document69 pagesKHH Handbook 2020saraliciatinahPas encore d'évaluation
- Primaquine PEC en Zone D'éliminationDocument42 pagesPrimaquine PEC en Zone D'éliminationDdsn DibaPas encore d'évaluation
- Compile Des CAT - CopieDocument21 pagesCompile Des CAT - CopieYoussra haderPas encore d'évaluation
- Malaria TTT Urgences Rev-2021Document7 pagesMalaria TTT Urgences Rev-2021stephanekoffi16Pas encore d'évaluation
- BonUsageAntibiotiques1 PDFDocument40 pagesBonUsageAntibiotiques1 PDFMamadou MbaoPas encore d'évaluation
- Spilf Groupe Reco Spilf Icd Escmid 2022Document10 pagesSpilf Groupe Reco Spilf Icd Escmid 2022jean duval destinPas encore d'évaluation
- Protocole de Prise en Charge Des Pathologies en Pediatrie IDocument11 pagesProtocole de Prise en Charge Des Pathologies en Pediatrie IAbba aliPas encore d'évaluation
- Choc Et Pancreatite AigueDocument39 pagesChoc Et Pancreatite AiguePauline SeignéPas encore d'évaluation
- PaludismeDocument33 pagesPaludismeLeonel TamaPas encore d'évaluation
- Protocole Therapeutique Chirurgie AntsirabeDocument21 pagesProtocole Therapeutique Chirurgie AntsirabenaydandomalalaPas encore d'évaluation
- Item 143 Agranulocytose Medicamenteuse PDFDocument1 pageItem 143 Agranulocytose Medicamenteuse PDFPetit Suisse FramboiséPas encore d'évaluation
- Referents2009 Atelier Atb GeriatrieDocument64 pagesReferents2009 Atelier Atb GeriatrieMeriem HoudaPas encore d'évaluation
- PaludismeDocument3 pagesPaludismeAlaa SobhiPas encore d'évaluation
- Livret Internes 20111128135420Document226 pagesLivret Internes 20111128135420gabi38100% (1)
- Jni2017 Ei StradyDocument33 pagesJni2017 Ei StradyRima RimaPas encore d'évaluation
- DIU Réa Médicaments en Cardiologie PédiatriqueDocument91 pagesDIU Réa Médicaments en Cardiologie PédiatriqueYoucef KelkouliPas encore d'évaluation
- PheoDocument42 pagesPheoSi LaPas encore d'évaluation
- CAS CLINIQAUEJUIN 2014 Nouveau Document Microsoft Office Word - PDF FilenameDocument10 pagesCAS CLINIQAUEJUIN 2014 Nouveau Document Microsoft Office Word - PDF FilenameAnis Ali-khodjaPas encore d'évaluation
- Cat Devant UnemeningiteDocument34 pagesCat Devant UnemeningiteSaid AssowehPas encore d'évaluation
- Exercices Evcf Et Evcp TinaDocument246 pagesExercices Evcf Et Evcp TinaLarbi Bouamrane AbdelkaderPas encore d'évaluation
- N°6 Intox Au ParacetamolDocument29 pagesN°6 Intox Au ParacetamolYacouba DembelePas encore d'évaluation
- Cas Cliniques ToxicoDocument75 pagesCas Cliniques ToxicoAya Eljazouli100% (1)
- Cardiomyopathie Du PrripztDocument15 pagesCardiomyopathie Du PrripztTHERESE BEHEPas encore d'évaluation
- PreeclampsieDocument46 pagesPreeclampsieManel KammounPas encore d'évaluation
- PaludismeDocument33 pagesPaludismeYounesPas encore d'évaluation
- CAS CLINIQAUE Nouveau Document Microsoft Office Word - PDF Filename UTF-8''CDocument9 pagesCAS CLINIQAUE Nouveau Document Microsoft Office Word - PDF Filename UTF-8''CAnis Ali-khodjaPas encore d'évaluation
- Protocole CHU PE - HTA GravidiqueDocument6 pagesProtocole CHU PE - HTA Gravidiquenganvtk.hmuPas encore d'évaluation
- Les Médicaments de L'hémostaseDocument10 pagesLes Médicaments de L'hémostaseLahcen ElmoumouPas encore d'évaluation
- Compte Rendu D'hospitalisationDocument6 pagesCompte Rendu D'hospitalisationAmir Na DzPas encore d'évaluation
- Emergency GuidelinesDocument11 pagesEmergency GuidelinesamirwassiPas encore d'évaluation
- Examen LaboDocument66 pagesExamen LaboGhizlan GharibPas encore d'évaluation
- Doc4 Suivi Therapeutique Pharmacologique ISDocument20 pagesDoc4 Suivi Therapeutique Pharmacologique ISMou SinayPas encore d'évaluation
- Les thérapies ciblées modernes du cancer du sein : mécanismes et application cliniqueD'EverandLes thérapies ciblées modernes du cancer du sein : mécanismes et application cliniquePas encore d'évaluation
- 7.hydrocéphalie de L'enfant Et NourissonDocument46 pages7.hydrocéphalie de L'enfant Et NourissonAlpha BaPas encore d'évaluation
- 13-10-14 Syndrome Inflammatoire Mise Au PointDocument121 pages13-10-14 Syndrome Inflammatoire Mise Au Pointjacques yiborPas encore d'évaluation
- Fibromyalgie 5Document7 pagesFibromyalgie 5sylvain bergPas encore d'évaluation
- 2005 06 14 Urgences Chez Patient Cirrhotique DR J-P MULKAYDocument5 pages2005 06 14 Urgences Chez Patient Cirrhotique DR J-P MULKAYNoadia RafararisonPas encore d'évaluation
- Affiche Infection MFA BRDocument1 pageAffiche Infection MFA BRdelfinnePas encore d'évaluation
- PéritonitesDocument16 pagesPéritonitesMohamed BoudouPas encore d'évaluation
- EBOOK Pascal Boniface - Geopolitique Du Covid-19 PDFDocument55 pagesEBOOK Pascal Boniface - Geopolitique Du Covid-19 PDFstaros100% (2)
- m2 Semio Sémiologie de La FièvreDocument34 pagesm2 Semio Sémiologie de La Fièvreأغا ني100% (1)
- Les Tendinites Des Fléchisseurs Au Poignet Et À La MainDocument16 pagesLes Tendinites Des Fléchisseurs Au Poignet Et À La MainurgencemainnicePas encore d'évaluation
- Planche Dépression CaractériséeDocument5 pagesPlanche Dépression CaractériséeSamia BelabbasPas encore d'évaluation
- Le Diabète 2020Document9 pagesLe Diabète 2020Hanane JibetPas encore d'évaluation
- Révision 3 Internes Avec CorrigéDocument10 pagesRévision 3 Internes Avec CorrigéRamzi RzPas encore d'évaluation
- Esprit Metaphore SanteDocument8 pagesEsprit Metaphore SantegrubanPas encore d'évaluation
- Tableau Folie Naheulbeuk JDR PDFDocument1 pageTableau Folie Naheulbeuk JDR PDFSolène BouillonPas encore d'évaluation
- Cour 01 Toxico DefinitionDocument9 pagesCour 01 Toxico DefinitionBrandon AustinPas encore d'évaluation
- 00 917Document9 pages00 917hizballah27Pas encore d'évaluation
- Introduction À La Semiologie NeurologiqueDocument12 pagesIntroduction À La Semiologie NeurologiqueSekou BoiguilePas encore d'évaluation
- Guide de PEC Des Méningite PurulenteDocument69 pagesGuide de PEC Des Méningite Purulentechouli mohamedPas encore d'évaluation
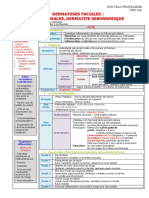
- 109 Dermatoses Faciales Acne - , Rosace - E, Dermatite Se - Borrhe - IqueDocument3 pages109 Dermatoses Faciales Acne - , Rosace - E, Dermatite Se - Borrhe - IqueAboubacar SomparePas encore d'évaluation
- Insuffisance Cardiaque de LDocument10 pagesInsuffisance Cardiaque de LAsma BdfPas encore d'évaluation
- 20-Infection À VIH - 2017Document12 pages20-Infection À VIH - 2017Sebbar SebbardPas encore d'évaluation
- Wcms 301237Document97 pagesWcms 301237chelcy kezetminPas encore d'évaluation
- Sf1 Resume FeedbackDocument15 pagesSf1 Resume FeedbackKhadija Barro ComptepleinPas encore d'évaluation
- Rsca 1Document9 pagesRsca 1Mohammed BoumlikPas encore d'évaluation
- Péricardites Mai 2023 Final-1Document20 pagesPéricardites Mai 2023 Final-1Lamine SavadogoPas encore d'évaluation
- Cancer Du ReinDocument27 pagesCancer Du ReinBelhadj AyoubPas encore d'évaluation
- Richaud 2010Document5 pagesRichaud 2010Hèla HassenPas encore d'évaluation
- 4 - ParamyxovirusDocument47 pages4 - ParamyxovirusIman Ahmed100% (3)
- Bible Medecine Interne Finale (Gratien) - 115141Document270 pagesBible Medecine Interne Finale (Gratien) - 115141Joel IrakizaPas encore d'évaluation
- Emm 117Document116 pagesEmm 117Boubacar IbrahimPas encore d'évaluation